|
Table of Content - Volume 13 Issue 2 - February 2020
Vaishali Agrawal1, Kiran Mahendra Rajole2*
1Associate Professor, 2Assistant Professor, Department of Obstetrics and Gynaecology, SMBT Institute of Medical Sciences and Research Centre, Dhamangoan, Nashik, INDIA. Email: kiran_rajole@yahoo.co.in
Abstract Background: Caesarean sections (CS) have become increasingly common in both developed and developing countries. Women having vaginal birth after caesarean (VBAC) or trial of scar (TOS) are at high-risk as it is associated with medical and legal implications. Aim: To assess the outcome of pregnancy in women with previous caesarean section with respect to type of delivery, maternal and perinatal complications. Material and Methods: Descriptive longitudinal study was carried out on 69 pregnant women with history of previous CS. Results: Mean age of females was 27.36years.Seventy percent cases were pregnant for second time. In 76.7% cases, gestational age was between 37 to 39 weeks. Out of 69 cases, 66.7% had FTND, 21.7% had LSCS and 11.6% had forceps assisted vaginal delivery. Among 17 cases with ARM and oxytocin injection, 82.4% had vaginal delivery and 17.6% had LSCS. Out of 15 cases with LSCS, 6 had fetal distress, 5 had meconium stained liquor, 3 had non-progress and 1 had scar dehiscence. Among 15 cases with LSCS, 80% had healthy new-borns, 13.3% had babies with low APGAR score and 6.7% had still births. Conclusion: Higher rates of successful and safe trail of labour and vaginal birth after previous CS can be achieved through careful selection of cases, prompt interventions at appropriate timing (like augmentation with oxytocin and instrumental vaginal delivery) and close monitoring with the help of partograph and other available techniques. Keywords: VBAC, Trial of Scar (TOS), TOLAC, Partograph, LSCS.
INTRODUCTION Caesarean sections (CS) have become increasingly common in both developed and developing countries. The international healthcare community has considered the ideal rate for caesarean sections to be between 10-15%.[1]Epidemic of CS is an immediate concern and deserves serious international attention.2 The phrase “once a caesarean, always a caesarean” which dictated obstetric practice in 1970 now changed to “once a caesarean section, always a hospital delivery.2 As a result of this, increasing number of women are facing the issue of mode of delivery in their subsequent pregnancies. Women having vaginal birth after caesarean (VBAC) or trial of scar (TOS) are at high-risk as it is associated with medical and legal implications.3 At places equipped with facilities to handle maternal and neonatal complication, the prognosis of the VBAC and that of repeat caesarean section (CS) group is almost identical in terms of perinatal and maternal deaths. However, in absence of this, elective repeat CS yields better prognosis.[4] With complete elimination of operative risk, less hospital stay and lower expenses, VBAC seems to be better than elective CS. But both methods have certain risks for mother and new born, which makes decision of choice difficult. So present study was planned to assess the outcome of pregnancy in women with previous caesarean section with respect to type of delivery, maternal and perinatal complications.
MATERIAL AND METHODS An observational descriptive longitudinal study was carried out at Tertiary Centre in Mumbai for the study duration of one year. Institutional Ethics Committee (IEC) was taken before the start of study. Sixty nine pregnant women with history of previous caesarean section (CS) coming to hospital for delivery and ready to give consent for participation were included in study. Exclusion criteria were cases with previous CS requiring repeat elective caesarean section (e.g. Placenta previa, malpresentations, Cephalo-pelvic disproportion), cases with previous CS where vaginal trial of labour can-not be recommended (e.g. abruption, cord prolapse) and cases with previous CS who did not attain active stage of labour (i.e. 3cm of cervical dilation) (e.g. cases delivered by caesarean before they reached active phase oflabour due to protracted latent phase). After taking written informed consent, detailed history and thorough examination was under taken to exclude any contraindication for vaginal trial of labour. After completing the preliminaries required at admission, patient was monitored continuously by trained personnel. Required parameters like Name, age, gravida, parity, previous obstetric history, type of operation, indication of previous caesarean section, postpartum complications, history of present pregnancy noted on admission. On examination general status, pulse, blood pressure, uterine activity, scar tenderness, gestational age, presentation, lie, fetal heart rate, cervical dilatation, effacement station were assessed. Patient and relative informed about risk of vaginal trial and possibility of repeat caesarean section. Careful observation of impending, signs of uterine rupture (i.e. pulserate, fetal heart, scar tenderness, blood pressure and progress of labour) was done. Patients in early labour were examined one hourly and above parameters were noted. Patients attending active stage of labour (i.e. 3cm of cervical dilatation) were attended every half –an-hourly. The partograph was plotted for these patients starting from zero hour. Referring to ABC of labour care5, active stagepartograph was used. This partograph was charted from active stage of labour (i.e. 3cm of cervical dilatation). The zero of cervico-gram correspond to the starting of active stage of labour of the patients. It contains only action line, as intervention to accelerate labour in the latent phase is not associated with an improvement in outcome. The two action lines shows, expected progress of cervical dilatation in multiparous (left) and primiparous (right) women. Rates of cervical dilation and descent were recorded. Augmentation with oxytocin and instruments was done where indicated. Maternal morbidities, intra-operative complications, indications for forceps and CS were noted down. Assessment of new-borns were done with APGAR score and other parameters. Data was entered in Microsoft Excel and analysed with SPSS. V16. Frequency, proportion, mean and standard deviation were as descriptive statistics. Chi-square test and student t test were used as inferential statistics. Statistical significance was set at p<0.05. Graphs and tables were used at appropriate places to present the data.
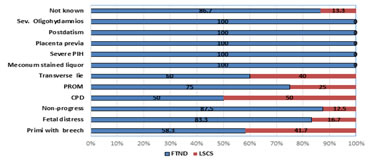
RESULTS Sociodemographic profile of study subjects is shown in table no.1. Highest number of women were of age 25 to 29 years (49.3%) followed by 20 to 24 years (29%) and 30 to 35 years (21.7%). Mean age of females was 27.36+/- 3.89 years. Seventy percent cases were pregnant for second time followed by second and third time pregnant females. In 76.7% cases, gestational age was between 37 to 39 weeks followed by 40 to 42 years (16.3%) and 34 to 36 years (7%). Two third women were booked and rest were not booked. Out of 69 cases, 66.7% had FTND, 21.7% had LSCS and 11.6% had forceps assisted vaginal delivery. Details of previous caesarean section are shown in table no. 2. Out of 54 women with vaginal delivery in present pregnancy the duration after previous CS was 2years in 24.1%, 2 to 4 years was in 40.7%, 4 to 6 years in 16.7%, 6 to 8 years in 13% cases and 8 to 10 years in 5.6% cases. Out of 15 women with LSCS in present pregnancy the duration after previous CS was 2years in 13.3%, 2 to 4 years was in 46.7%, 4 to 6 years in 13.3% and 8 to 10 years in 26.7% cases. Overall higher number of cases (42%) reported 2 to 4 years duration. Among 15 cases with transverse scar in previous CS, 73.3% had vaginal delivery and 26.7% had LSCS in current pregnancy. Statistical associations in any of above case were not significant. Among 69 cases, 17.4% of cases with indication of primi with breech presentation and fetal distress each as an indication of previous caesarean section. In 21.7% of cases indication of previous caesarean was not known. As shown in figure no.1, in all cases with severe oligohydramnios, post-datism, placenta previa, severe PIH and meconium stained liquor in previous pregnancy were having vaginal delivery in present pregnancy. Cases with CPD (50%), transverse lie (40%), breech presentation (41.7%), PROM (25%), fetal distress (16.7%) and non-progress (12.5%) in previous pregnancy had LSCS in current pregnancy. Association between indication of previous pregnancy CS and current pregnancy mode of delivery was not statistically significant. As seen in table no.3, 48 cases with ARM (artificial rupture of membrane), and 79.2% had vaginal delivery and 20.8% had LSCS. Among 17 cases with ARM and oxytocin injection, 82.4% had vaginal delivery and 17.6% had LSCS. While in 4 cases with no intervention, vaginal delivery and LSCS were done in 50% cases each. Association between intervention and mode of delivery was statistically highly significant. Out of 15 cases with LSCS, 6 had fetal distress, 5 had meconium stained liquor, 3 had non-progress and 1 had scar dehiscence. Among 8 cases with forceps delivery, 1 had fetal distress and 1 had maternal exhaustion and in 6 cases forceps delivery done to cut short 2nd stage of delivery. Out of 15 patients requiring repeat caesarean in 5 patient, morbidity due to fever, urinary tract infection, blood transfusion and wound infection was observed. As indicated in table no.4, all babies (100%) borne to 54 cases with vaginal delivery were healthy. Among 15 cases with LSCS, 80% had healthy new-borns, 13.3% had babies with low APGAR score and 6.7% had still births. Mean birth weight in vaginal delivery was 2.7 kg with SD of 0.40 to that of in repeat caesarean 2.93 kg with SD of 0.36. Association between birth weight of babies and mode of delivery was statistically not significant. Table 1: Demographic characteristics of study population
*FTND: Full term normal delivery; #LSCS: Lower (uterine) segment Caesarean section
Table no. 2: Details of previous caesarean section
Figure. no.1: Indications for previous caesarean section and mode of delivery in present pregnancy
Table 3: Interventions required for delivery
*ARM: Artificial Rupture of Membrane; #Oxy: Oxytocin
Table 4: Indications, intra-operative complications and morbidities in study participants.
Table 5: Perinatal outcomes among study participants
DISCUSSION The decision for the elective repeat LSCS or trial of labour in should be based on thorough counselling and careful selection as cases with previous LSCS require special treatment in antenatal care period and during labour.6 Previous study reported, 60-80% success in VBAC (vaginal birth after caesarean section).2,6,7 In present study, rate of VBAC was slightly lower (54%). Balachandran et al3 reported 40% women with previous single delivery in their study which was comparable with present study finding. In current study, half of cases were of age 25 to 29 years with mean age of 27.36 years. Almost three fourth had gestational age of 37 to 39 weeks. Two third were booked and had full term normal delivery (FTND) while 11.6% required forceps delivery and 21.7% required LSCS. Study done by Patel et al8 reported 21 to 30 years as most common age group (84%), 26 years as mean age, 37 to 38 weeks as most common gestational age, FTND as most common mode of present delivery (63%) which were comparable with current study. Study done by Patel et al8 reported 91% cases with vaginal delivery had duration of more than 18 months since previous CS while 79% with LSCS had duration of more than 18 months since previous CS. Kalisa et al[9] reported prolonged labour, fetal distress and malpresentations as an indication for previous CS. They also reported higher rate of failed trial of labour in prolonged labour. In current study, vaginal delivery rate increase with the interventions for augmentation as compared to the caesarean rates which was statistically very significant. In current study, only one case was taken for repeat caesarean section for the indication of scar dehiscence. This was detected on partograph by fetal decelerations and maternal tachycardia. Fetal distress was also detected on partograph. When labour progress curve touched the action line of multigravida in partograph, patients were taken for caesarean section for the indication of non-progress. Patel et al8 reported failure to progress of labour (44.12%), fetal distress (20.58%), scar tenderness (32.35%) and prolonged latent phase (2.95%) as indication for present delivery LSCS. They also reported scar rupture (2.9%) and scar dehiscence (23.52%) as intra-operative complications. Study done by Balachandran et al3 reported malpresentation (13.88%), big baby (8.33%) and others as an indications for present LSCS. They also reported, post-partum haemorrhage (2.6%), scar dehiscence (1.5%) and adherent placenta (0.7%) as causes of maternal morbidities. Landon et al10, Mafatlal et al11 reported in their study that both repeat caesarean delivery and trial of labour was not risk free. Patel et al8 reported incidence of complication in caesarean group was 17.63% and 3.89% in VBAC group. Studies done by Shah SR et al6, Dodd J et al[12], and Mozurkewich EL et al[13] found no statistically significant difference in maternal morbidity rate. Association between birth weight of babies and mode of delivery was found to be statistical significant in study done by Balachandran et al3. Current study finding was different from this which reported statistically not-significant association. In present study, complications rate was more in babies born to LSCS deliveries. This finding was comparable with studies done by Patel et al8, Shah et al11 and Goel et al14 who reported lower complications rates in VBAC compared to LSCS.
CONCLUSION Previous vaginal birth after caesarean section yields higher success rate than cases with no previous vaginal delivery. Higher rate of vaginal delivery was observed in cases with spontaneous labour, higher levels of parity and cases receiving interventions for augmentation. Higher rates of successful and safe trail of labour and vaginal birth after previous caesarean section can be achieved through careful selection of cases, prompt interventions at appropriate timing (like augmentation with oxytocin and instrumental vaginal delivery) and close monitoring with the help of partograph and other available techniques
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home