|
Table of Content - Volume 13 Issue 2 - February 2020
Perioperative complications with recurrent caesarean section
Aparajita Mishra1, Surekha Gawade2*, Shilpa Chaudhari3
1Pg Resident, 2Assistant Professor,3Professor & HOD, Department of Gynaecology, Smt Kashibai Navale Medical College, Pune, Maharashtra, INDIA. Email: aparajita3101@gmail.com, surekha.gawade10@gmail.com, drshilpachaudhari15671@gmail.com
Abstract Background: Pregnancy with previous caesarean has become common now a days because of further increase in the rate of primary caesarean section. There has been increase in the rate of caesarean section in India from 8.5% in (2005-06) to 17.2% (2015-16). Method: Observational prospective study in 400 cases done during the period of September 2017 to September 2018 (1 year) to study the incidence and type of surgical difficulties in patient with repeat Caesarean section and on table complication that were seen consecutively in the department of obstetrics and gynecology , tertiary care hospital, Pune Maharashtra. Results: In the present study intraoperative complications were seen more in cases with previous 3 sections like adhesions (75 %), scar dehiscence (25 %), thinned out LUS (75 %), hemorrhage (50 %). Scar dehiscence was observed more in emergency LSCS compared to elective LSCS. Bladder injuiry was present in 3 cases. In the present study PPH, placenta previa, adhesions was common causes of hemorrhage. In the present study hysterectomy was done in 2 cases, one was done in previous 1 caesarean section due to atonic PPH and other was done in previous 2 caesarean section due to placenta previa. NICU admissions are more seen in cases of emergency caesarean section (fetal distress, neonatal sepsis). Perinatal death was seen in total 4 cases out of them two results from prematurity and rest two due to early and late onset sepsis. Conclusion: The evaluation of our study data shows a significant increase in maternal morbidity with repeat Caesarean section. Our study, in light of this background, will help us to provide information on the probable complications of placenta previa and adhesions in particular, guiding patients away from elective CS and directing them towards vaginal delivery after caesarean section. Key Words: caesarean section, Lower segment caesarean section, Postpartum haemorrhage, Vaginal birth after caesarean section, Lower uterine segment.
INTRODUCTION Caesarean section is defined as the birth of fetus through incision on anterior abdominal wall and uterine wall after the period of viability. Pregnancy with previous caesarean has become very common now a days because of the increase in the rate of primary caesarean section. There has been increase in the rate of caesarean section in India from 8.5% in (2005-06) to 17.2% (2015-16).1,2. The increase in the rate of caesarean sections are mainly due to advent of newer and safer aesthetic techniques and availability of the blood, better antibiotics, more meticulous fetal monitoring with better neonatal care facilities. One of the commonest indications of caesarean section is previous caesarean section. According to one of the largest studies, serious maternal morbidity increases with further increasing number of caesarean deliveries specifically from the triad of placenta previa, placenta accreta and caesarean hysterectomy 3,4,5. The risk of complications increases with increase in the number of caesarean section due to formation of adhesions and scarring. Scar rupture is another catastrophic complications associated with previous caesarean section. It has also been reported that complication rate is higher in emergency caesarean sections as compared to elective ones.5,6 Caesarean section (CS) is the surgical intervention which is done to ensure the safety of both the mother and the fetus when vaginal delivery is not possible (emergency CS) or when there is danger to the mother or fetus with vaginal delivery (elective CS)7. Incidence varies from 10% to 25% in developed countries 8. In India the rate of caesarean section delivery has further increased from 3 per cent to 10 percent between 1992-93 and 2005-06 (IIPS, 2007) which is much lower compared to some developing nations like Brazil and China 9. But as India is the second most populous country in the world, a small percentage increase affects a huge number of the people. Based on DLHS-3 data (2007-2008), the caesarean section delivery rate in India is 9.2 per cent. However, a substantial inter-state variation of CS further exists in India. The rate of CS is higher in urban areas compared to rural counterparts for all the states. After any laparotomy, it is common to develop scar tissue, adhesions and bladder extension. Multiple CS is associated with more difficult surgeries associated with increased blood loss compared with a planned second CS. The risk of major complications increases with number of previous CS. Scaring and adhesion formation is known to cause increase in the major complication rates from 4.3 to 12.5% 10. Intra peritoneal adhesions have varying incidence from 5.5% to 42.5% 11. Women with a history of CS have a higher risk of hemorrhage, placenta previa, uterine rupture, stillbirth in the following pregnancies, which contributes to maternal as well as fetal morbidity. The present study aims at knowing the various intraoperative complications encountered during repeat caesarean sections with respect to those undergoing primary CS.
MATERIALS AND METHODS Observational prospective study in 400 cases done during the period of September 2017 to September 2018 (1 year) to study the incidence and type of surgical difficulties in patient with repeat Caesarean section and on table complications that were seen consecutively in the department of obstetrics and gynecology , tertiary care hospital, Pune Maharastra during a one year study period as mentioned above. Pregnant women admitted in the Department of Obstetrics and Gynaecology with the history of previous caesarean section (one or more) and patients not willing for VBAC were randomly selected and included in the study. Pregnant women with the history of any other major open abdomino-pelvic surgeries, with multiple pregnancy, polyhydramnios, abruptio placenta and with any medical illness like severe hypertension, jaundice, heart disease and severe anemia were also excluded from the study. Patients were selected according to the inclusion and exclusion criteria. Case histories of repeat caesarean deliveries were studied and the data were recorded . The existing methods of performing caesarean procedures did not affect the study. The particular difficulties we encounter while operating a repeat cesarean section were meticulously noted. The observed intraoperative problems were analysed and categorized in relation to age , parity, number of C-section, for both previous and present pregnancy. The decision for caesarean section was taken based on clinical evaluation of progression of labor , fetal condition, station and its position (in pelvis) ,maternal conditions and patients not willing for VBAC ( vaginal birth after caesarean section). All the intraoperative details were noted and complications were managed promptly. RESULT The present study shows maximum no of sections were done in the age group of 20-24 yrs (40%), followed by 25-29 yrs ( 27.5%). No of caesarean section done in teenage pregnancy is 7.5% and elderly is 5%.
TABLE 1: AGE WISE DISTRIBUTION OF PREVIOUS CAESAREAN SECTION
TABLE 2: RELATIONSHIP OF COMPLICATIONS WITH BMI
Out of 400 cases 240 (60%) patients have Normal BMI 18-24.9, 110 (27.5%) are overweight, rest 50 (12.5%) belong to Obsese class 1. TABLE 3: INCIDENCE OF EMERGENCY AND ELECTIVE LSCS
In the present study no of cases that underwent emergency Caesarean section were slightly more than elective caesarean section. TABLE 4: NUMBER OF PREVIOUS CESAREAN SECTION
Out of 400 cases of repeat C-sections studied, 276 (69%) cases had undergone previous 1 Caesarean section, 120 (30%) cases had undergone previous 2 Caesarean sections and 4 (1%) cases had undergone previous 3 Caesarean sections.
TABLE 5: RELATIONSHIP OF INTRAOPERATIVE COMPLICATIONS WITH NO OF PREVIOUS SECTION
In the present study, complications were seen more in cases with previous 3 sections like adhesions (75 %), scar dehiscence (25 %), thinned out LUS (75 %), hemorrhage (50 %). Scar dehiscence was more in case of emergency LSCS compared to elective LSCS. Bladder injuiry was seen in 3 cases out of that 2 had dense adhesion and bladder was opened, another 1 case had serosal injuiry of bladder. Repair of bladder injuiries were done and postoperative period was uneventful. In the present study PPH, placenta previa, adhesions was common causes of hemorrhage. All cases of hemorrhage were successfully managed. In the present study hysterectomy was done in 2 cases one was done in 1 previous caesarean section due to atonic PPH and other was done in 2 previous caesarean section due to placenta previa.
TABLE 6: TYPES OF ADHESIONS AND THEIR INCIDENCES
In the present study , total 34 cases has adhesions present between parietal peritoneum and anterior surface of uterus , parietal peritoneum and omentum in 28 cases, followed by adhesions between rectus muscle and peritoneumin total 14 cases. These adhesions led to prolonged operative time, increased blood loss and bladder injuries and delay in delivery of fetus. TABLE 7: RELATIONSHIP OF POSTOPERATIVE COMPLICATIONS WITH NO OF PREVIOUS CS
Postoperative complications has increased as the no of previous CS increased because of intraoperative complications that required prolonged operative time and increased tissue handling.
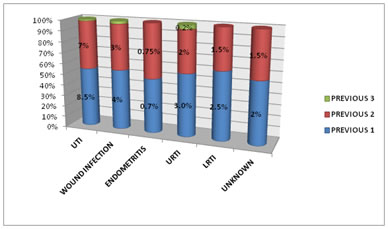
FIGURE 2: CAUSES OF POSTOPERATIVE FEBRILE MORBIDITY Most common cause of postoperative febrile morbidity in the present study was UTI followed by wound infection.
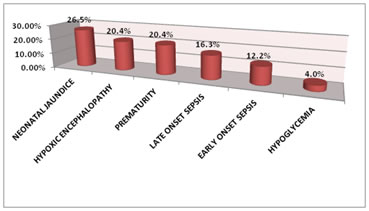
TABLE 8: CAUSES OF NICU ADMISSIONS
FIGURE 3: CAUSES OF NICU ADMISSIONS NICU admissions are seen more in cases of emergency caesarean section (fetal distress, neonatal sepsis). Among them most common cause of NICU admission was neonatal jaundice , seen in 13 (26.5%) , prematurity was seen in 10 (20.4%) , Early and late neonatal infection in 8 (16.3%), 6 (12.2%) and hypoglcemia in 2 (4.08%). Perinatal death was seen in total 4 cases out of them two results from prematurity and rest two due to early and late onset sepsis.
DISSCUSSION INTRAOPERATIVE COMPLICATIONS AND A NUMBER OF PREVIOUS CAESAREAN SECTIONS. Multiple caesarean sections predisposes to an increased risk of severe dense adhesions, scar dehiscence ,uterine rupture, abnormal placentation, significant hemorrhage, bladder injuries and caesarean hysterectomies. In a study conducted by Farkundah 12 showed that incidence of complications were more in women with 2 previous caesarean sections, the most common complications were dense adhesions (35.5%), followed by thinned out lower uterine segment (16.6%), ruptured uterus (1.1%), and bladder injuiry (1.1%).In a study by Mahale et al 13 incidence of abnormal placentation was more with 3 or more caesarean sections (2%) as compared with 2 previous caesarean sections. In the present study , complications were seen more in cases with previous 3 sections like adhesions ( 75 %), scar dehiscence ( 25 %), thinned out LUS ( 75 %), hemorrhage ( 50 %). Scar dehiscence was more in cases with emergency LSCS compared to elective LSCS. Bladder injuiry was present among 3 cases out of that 2 had dense adhesion and bladder was opened, another 1 case had serosal injury of bladder. Repair of bladder injuries were done and postoperative period was uneventful. In the present study PPH, placenta previa, adhesions was common causes of hemorrhage. All cases of hemorrhage were successfully managed. In the present study hysterectomy was done in 2 cases one was done in 1 previous caesarean section due to atonic PPH and other was done in 2 previous caesarean section was done due to placenta previa. CAESAREAN DELIVERY AND ADHESIONS In a study conducted by Lyell DJ 14 showed that the incidence of adhesion development after primary caesarean section ranges from 46-65%. In a retreospective study conducted by Morales et al 15 in 542 women found that the incidence of adhesions was greater among women who underwent repeat caesarean delivery and the percentage of women with adhesions increased with each subsequent caesarean delivery. Nisenblat 16 et al demonstrated that dense adhesions were significantly more common among women who underwent third or more caesarean section than among women who undergo their second caesarean section. In the present study adhesions were seen in 13.7%, 35%, 75% in previous one and previous two and previous three caesarean section respectively. In the present study in total 34 cases adhesions were present between parietal peritoneum and anterior surface of uterus , parietal peritoneum and omentum in 28 cases, followed by adhesions between rectus muscle and peritoneumin in total 14 cases. These adhesions led to prolonged operative time, increased blood loss and bladder injuries and delay in delivery of fetus which were managed by adhesiolysis and in some cases incision was taken higher up. THINNED OUT LOWER UTERINE SEGMENT In a study conducted in 240 repeat caesarean sections by khursheed F, Sirichand P, jatoi N 12 observed that there was high incidence of extremely thinned out lower uterine segment (16.6%), in women with previous two sections as compared to women with previous one caesarean section 8.7% and 8.3% in previous 3 caesarean sections. In present study thinned out lower uterine segment was seen in 14.4% of cases with one previous section and 15% in two previous sections and 75% of the cases with three previous caesarean section. CAESAREAN SECTION AND SCAR DEHISCENCE In a study conductedin 240 repeat caesarean section by khursheed F, Sirichand P, Jatoi N 12 observed that scar dehiscence was seen in 7.8% of women with previous one caesarean section, 4.4% with previous two caesarean section and 5.5% in previous 3 caesarean sections. In present study scar dehiscence was found in 6 cases (1.5 %). Out of these cases scar dehiscence was seen in 0.7%, 2.5%, 25% of women with previous one, previous two, previous three caesarean section . CAESAREAN SECTION AND HEMORRHAGE The reason for excessive blood loss after caesarean section includes uterine atony, adhesions, adherent placenta and trauma. In a study conducted by Isreal 16, 2 or more caesarean delivery was associated with greater rates of excessive blood loss than previous 1 caesarean delivery. Silver et al 17 observed that among women who delivered by caesarean delivery without labour, the risk of transfusion of more than or equal to 4 units of red blood cells was associated with increased number of caesarean deliveries. In the present study PPH, placenta previa, , placenta accrete, adhesions, abruption, and extension of uterine incision was common causes of hemorrhage. All cases of hemorrhage were successfully managed BLADDER INJURIES Injuiry to the bladder is significantly more frequent at repeat caesarean delivery . The incidence of bladder injuiry that was assessed in a cohort study of 14,757 caesarean deliveries performed at iarger academic center in Rhode island 18 over a period of 7 year was found to be 0.28%. and found that women who underwent a repeat caesarean section were almost 4 times likely to experience a bladder injuiry than women who underwent primary caesarean section. In our study out of 3 cases 0.3% had bladder injuiry in previous one caesarean section and with 1.6% in second section. Only serosal injuiry was seen in 1 cases and complete bladder injuiry was seen in 2 cases. All of them had repair and complete healing took place and were discharged without any dribbling after 14 days catheterization. CAESAREAN SECTION AND PLACENTA PREVIA In a cohort of 723 women with placenta previa in MFMU network study placenta accreta occurred in 3%, 11%,40%,61% of those having their first, second , third , fourth caesarean section. In the present study three cases of placenta previa were seen in previous 1 and 2 caesarean section. Out of that 1 leads to peripartum hysterectomy. FEBRILE MORBIDITY Lynch et al 19 showed an increasing incidence of UTI with each additional caesarean section 17.5%, 8.4%, and 17.9% after the third caesarean section respectively.In a study done by Saadiya Z (20), incidence of UTI increased with no of caesarean section, 3% in cases with 3 or less caesarean section and 24% in cases with more 3 or more sections. Most common cause of postoperative febrile morbidity in the present study was UTI followed by wound infection NICU admissions are more seen in cases of emergency caesarean section (fetal distress, neonatal sepsis). Among them most common cause of NICU admission was neonatal jaundice seen in 13 (26.5%) , prematurity was seen in 10 (20.4%) , Early and late neonatal infection in 8 (16.3%), 6 (12.2%) and hypoglcemia in 2 (4.08%). Perinatal death was seen in total 4 cases out of them two results from prematurity and rest two due to early and late onset sepsis. CONCLUSION The evaluation of our study data shows a significant increase in maternal morbidity with repeat Caesarean section. Placenta previa and adhesions seems to play a central role in all the risks. This problem can be overcome by identifying patients at risk during pregnancy in peripheral centers and directing these patients to referral centers, especially during the third trimester. Our study, in light of this background, will help us provide information on the probable complications of placenta previa and adhesions in particular, guiding patients away from elective CS and directing them towards vaginal delivery after CS Perioperative complications increases with each subsequent repeat caesarean section. Present study also showed increase risk of complications like adhesions, scar dehiscence, hemorrhage, bladder injuries, placental complications and hysterectomy. Adequate adhesion prevention strategies like meticulous hemostasis and peritoneal closure should be encouraged. The present study also showed the increased risk of postoperative febrile morbidity. Our results clearly demonstrate that with appropriate prenatal care and adequate preoperative preparation , maintenance of meticulous surgical techniques and careful postoperative follow up can dramatically reduce the intraoperative morbidity without any mortality.
ACKNOWLEDGEMENT Authors would like to thank to institutional head , head of department of obstetrics and gynaecology and all our colleagues from department of obstetrics and gynaecology. Smt kashibai navale medical college and general hospital for providing help and support for the project.
REFFERENCES
Policy for Articles with Open Access
|
|
 Home
Home