|
Table of Content - Volume 14 Issue 2 - May 2020
Study of vaginal discharge in perimenopausal age group
Ganesh Tondge1, Poonam Desai2, Shailesh Vaidya3, Prakash Patil 4, Suvarna Kale5, Mayuri Dixit6
1Associate Professor & HOD, 2,4IIIrd Year Junior Resident, 3Associate Professor, 5Assistant Professor, 6Senior Resident, Department of Obstetrics & Gynecology, S R T R, G M C, Ambajogai, Dist. – Beed, Maharashtra INDIA.
Email: dpoonam1319@gmail.com
Abstract Background: Perimenopause begins several years before menopause. Vaginal discharge in this perimenopausal age group may be physiological i.e. leucorrhea or pathological i.e. vaginitis discharge. Vaginitis is usually because of infections like Candida species, Trichomonas vaginalis and Bacterial vaginosis. Sometimes the discharge originates from Cervical neoplasm. Cervical cancer associated with discharge can be successfully treated if detected early. Aims and objective:1) To assess incidence of different causes of vaginal discharge in perimenopausal age group. 2) To assess incidence of malignancy in patient of vaginal discharge in study group. 3) To evaluate effect of different treatment modalities in the study. Methods: Patients of age group 45-55 years presented to gynecological OPD from Dec. 17 to Oct. 19 with vaginal discharge were examined. all necessary investigations were done to evaluate cause and treated according to the cause and then evaluation was done. Results: Main cause of discharge was infection 50%, leucorrhea 21%, nonmalignant cervical lesion 13%, premalignant lesion 11.5 %, cervical malignancy 2.5 %. Acute cervicitis being the main cause wise distribution in case of infection and secondly bacterial vaginosis. Erosion (73.09%) was the main cause among non-malignant lesions. On per speculum hypertrophied unhealthy cervix (5.5%), visible growth on cervix and hard nodular cervix seen in 1.5 and 2% respectively. On pap smear results acute inflammatory smear 39%, ASCUS 5.5%, LSIL 4%, HSIL 1.5%, squamous cell carcinoma 1.5 %, AGCUS 1.5%. Majority 55% were given kit 2 and kit 6 as treatment and 22% were advised vaginal douche. Conclusion: Incidence of vaginal discharge in perimenopausal women coming to the outpatient department of gynecology is very high of which infection are most common and for that oral antibiotic are found to most effective. Out of 200 number of cases of vaginal discharge 5 (2.5%) number of cases turned out to be malignancy and 23 (11.5%) turned to be premalignant lesion. All malignancies were of cervical cancer for which radiotherapy is preferred choice.
Keywords: perimenopause, vaginal discharge, leukorrhea, cervical cancer
INTRODUCTION
Women are the nucleus of the society. The focus now is to provide holistic health care that values women participation and cooperation, health care experience, in which the women is the true owner and caretaker of her body. Perimenopause begin several years before menopause. The average length of perimenopause is 4 years, but for some women this stage may last only a few months or continue for 10 years. In our area usually the menopause occurs around 50 to 54 year age so perimenopausal age group is considered as 55 year. Vaginal discharge in this perimenopausal age group may be a normal physiologic occurrence or a pathological. When considering the causes of vaginal discharge, it is useful first to distinguish between non-infectious and infectious causes; Noninfectious Causes are Physiological and Non-Physiological. Infectious Causes includes Vaginal discharge like Candida species, Trichomonas vaginalis, Bacterial vaginosis and Cervical discharge like Neisseria gonorrhea Chlamydia trachomatis, Herpes simplex virus. Atrophic vaginitis must also be considered in the differential of vaginal discharge. Non infective cervical lesion may produce excessive secretion which pours out at the vulva. Such lesions are cervical ectopy, chronic cervicitis, mucous polyp and ectropion (cervical glands are exposed to the vagina). Patient history and physical examination findings may suggest a diagnosis. Most of the time a presumptive diagnosis is made based on the nature of the discharge (clinical diagnosis), which is often inaccurate and incomplete. To address the limitations of clinical diagnosis, the World Health Organization (WHO) developed and advocated the syndromic management approach, but this management has some disadvantage. Over the age of 45 in women, cervical cancer occurrence is 60% whereas over 65 ages the occurrence percentage is 20% approximately. Infection with HPV (Human Papilloma Virus) plays as important cervical carcinoma contributor. To assess the incidence of vaginal discharge in perimenopausal women and possible incidence of malignancy this study is undertaken also there is evaluation of different modalities. In Indian women poor genital hygiene is a major cause of leucorrhea. Screening of all symptomatic women complaining of leucorrhea is necessary to detect cause and to pick up any cervical epithelial abnormalities, as precursor lesions of cancer cervix largely remain asymptomatic. Pap smear screening for cervical cancer and precancerous conditions has been proved to be very effective in cervical cancer prevention and in reducing mortality. The Bethesda System 2001 has clearly mentioned criteria and fixed terminologies making it easy for physician to understand and plan the treatment accordingly Pap smear testing related to cervical cancer presence drastically reduces in morbidity and mortality through early detection, diagnosis and management of cervical cancer. This cytological testing is one of the merest tools available to find the occurrence of cervical cancer.
AIMS AND OBJECTIVE
- To assess incidence of vaginal discharge in perimenopausal women’s coming to outpatient department.
- To assess incidence of malignancy in patients of vaginal discharge.
- To assess incidence of different causes of vaginal discharge.
- To evaluate effect of different treatment modalities.
MATERIALS AND METHODS
This is a random selective hospital based follow up study conducted at rural tertiary care Hospital, between duration December 2017 to October 2019 in patients coming to the outpatient department of gynecology.
SELECTION CRITERIA: 1) Age group 45-55 years 2) Patients coming with complaint of vaginal discharge.
EXCLUSION CRITERIA: 1) Less than 45 and more than 55 years 2) Pre diagnosed patients, patients coming with bleeding per vaginum or menstrual irregularities.
METHODS
- Patients of age group 45-55 years come to gynecological outpatient department fulfilling selection criteria had a detailed medical history, clinical examination and appropriate investigation done.
- Diagnosis of vaginal discharge done to assess cause of abnormal vaginal discharge. Patients are to be treated according to the cause. Then evaluation is to be done.
- Data collection sheet includes patient’s information, nature of vaginal discharge, per speculum findings, per vaginal finding, diagnosis of vaginal discharge, other investigation done to make diagnosis, treatment given.
- Patient with malignancy detected referred to cancer hospital for radiotherapy. Results were analyzed using percentage.
OBSERVATIONS AND RESULTS
Total 1240 patients of age group 45 to 55 come to outpatient department in study duration of which 645 of women complains of vaginal discharge. Out of which 200 cases selected randomly for study with consent.
Table 1: Distribution of causes of vaginal discharge
Causes |
Number of cases |
Percentage |
Leukorrhea |
42 |
21% |
Infection
|
100 |
50% |
Non-Malignant Lesion |
26 |
13% |
Cervical Malignancy |
5 |
2.5% |
Premalignant Lesion |
23 |
11.5% |
Atrophic Vaginitis |
4 |
2% |
Total |
200 |
100% |
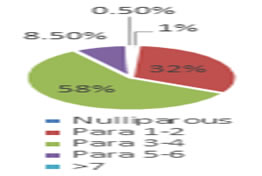
Graph 1: showing parity wise distribution
Table 2: Cause wise distribution in case of infection (n=100)
Causes |
Number of cases |
Percentage |
Trichomoniasis |
19 |
19% |
|
Vaginal Candidiasis |
15 |
15% |
Bacterial Vaginosis |
21 |
21% |
Cervicitis |
Acute |
30 |
30% |
Chronic |
3 |
3% |
Nonspecific Vaginitis |
9 |
9% |
Herps Simplex Vaginitis |
3 |
3% |
Total |
100 |
100% |
Table 3: Cause wise distribution of non-malignant cervical lesions (n=26)
Cause |
Number of cases( n) |
Percentage |
Erosion |
19 |
73.09% |
Chronic inflamed hypertrophic cervix |
3 |
11.53% |
Polyp |
2 |
7.69% |
Fibroid |
1 |
3.84% |
Cervical descent |
1 |
3.84% |
Total |
26 |
100% |
Table 4: Per speculum examination findings
Table 5: Distribution of cervical malignancies and premalignant lesion
Cervical malignancy |
Number of cases |
Percentage |
Premalignant lesion |
23 |
82.14 % |
Malignant lesion |
5 |
17.86 % |
Total |
28 |
100 % |
Table 6: shows in Cervicovaginal Cytology Interpretation / Results by Bethesda System
PAP smear interpretation |
No of cases |
percentage |
Acute inflammatory smear |
78 |
39 |
Acute cervicitis |
31 |
15.5 |
Chronic cervicitis |
6 |
3 |
Inadequate smear |
7 |
3.5 |
Negative for intraepithelial lesion |
49 |
24.5 |
ASCUS |
11 |
5.5 |
LSIL |
8 |
4 |
HSIL |
3 |
1.5 |
Squamous cell carcinoma |
3 |
1.5 |
AGCUS |
3 |
1.5 |
Adenocarcinoma |
0 |
0 |
Trichomoniasis |
1 |
0.5 |
Total |
200 |
100 |
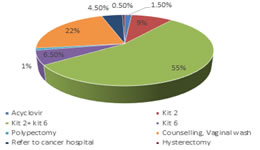
Graph 2: Management of the patients
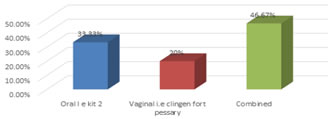
Graph 3: Vaginal candidiasis treated with oral vs vaginal treatment
Table 7: Association between cause of vaginal discharge and treatment given
Cause / treatment |
Acyclovir |
Kit 2 |
Kit 2 with 6 |
Kit 6 |
Polypectomy |
Counselling, vaginal wash |
Refer |
Hysterectomy |
Total |
Leucorrhea |
0 |
0 |
0 |
0 |
0 |
42 |
0 |
0 |
42 |
infection |
3 |
14 |
76 |
6 |
0 |
1 |
0 |
0 |
100 |
Non-Malignant Lesion |
0 |
0 |
22 |
0 |
2 |
1 |
0 |
1 |
26 |
Cervical Malignancy |
0 |
|
0 |
0 |
0 |
0 |
5 |
0 |
5 |
Premalignant Lesion |
0 |
0 |
11 |
7 |
0 |
0 |
5 |
0 |
23 |
Atrophic Vaginitis |
0 |
3 |
1 |
0 |
0 |
0 |
0 |
0 |
4 |
Total |
3 |
18 |
110 |
13 |
2 |
44 |
9 |
1 |
200 |
DISCUSSION
This is a random selective hospital based follow up study conducted on 200 perimenopausal women with vaginal discharge from age group 45 to 55 year in rural tertiary care hospital by using case record form and other necessary means with a focus on incidence diagnosis and treatment of their symptoms and underlying disease. The present study shows incidence of vaginal discharge among perimenopausal age group is 52.01%. It indicates high incidence of vaginal discharge in perimenopausal age group. This shows that majority of perimenopausal women attending hospital presents with vaginal discharge. Mean age in years was 48.8+ 3.15, ranging from 45 to 55 years. In present study it was seen that majority 58% were para 3-4, and secondly 32% were para 1-2, whereas least is in parity more than 7 (0.5%) followed by nulliparous 1%.In present study majority patients showed isolated vaginal discharge 45%, 20.5 had itching, 17.5% had pelvic discomfort, 11% had dysuria, 4% had dyspareunia, and 2.5% had fever. Present study showed that majority of cases had infection (50%), followed by leucorrhoea in 21%, non-malignant cervical lesion in 13%, premalignant lesion in 11.5%, cervical malignancy in 2.5% and atrophic vaginitis in 2%. Thus, infection is most important causing gynaecological morbidity. The infection is due to poor personal hygiene because of an awareness towards health, poverty and low socioeconomic strata in rural area. premalignant lesion is third common cause in perimenopausal vaginal discharge. Thus, study concludes at least one Pap smear screening test of cervix of all women between age 45 to 55 year, which can decrease gynaecological morbidity and mortality of cervical carcinoma. In present study there were 100 cases of infection. There are variety of infection that causes vaginal discharge. Many infections can be categorised based on the character of discharge. Among them majority 33% had cervicitis, followed by 21% had bacterial vaginosis, 19% had trichomoniasis, 15% had vaginal candidiasis,9% had nonspecific vaginitis and 3% had Herps Simplex Vaginitis. In present study 3 patients had herpes simplex. In present study there were 26 cases of non-malignant cervical lesion. Among them majority 73.09% had erosion, 11.53% had Chronic inflamed hypertrophic cervix, 7.69% had polyp, 3.84% had fibroid and 3.84% had cervical descent. Thus, hormonal change during perimenopausal age group makes erosion to be common non-malignant cervical lesion. On per speculum examination it was seen that majority 80.5% had no gross pathology, whereas 10.5% had cervical erosion, 5.5% had Hypertrophied, unhealthy cervix, 2% had hard nodular cervix and 1.5% had visible growth on cervix. In present study, 5 cervical malignancies confirmed by cervical biopsy, 23 cases were premalignant lesion diagnosed by PAP smear. Present study showed that in Cervicovaginal Cytology Interpretation / Results by Bethesda System it was seen that majority 39% showed acute inflammatory smear, followed by 24.5% Negative for intraepithelial lesion, 15.5% Acute cervicitis, 5.5% ASCUS, 4% LSIL, 3.5% inadequate smear, 3% chronic cervicitis, 1.5% each HSIL, Squamous cell carcinoma, AGCUS respectively and 0.5% trichomoniasis. Thus, PAP smear is simple test that detect changes to the cell of cervix that may lead to cervical cancer. So, PAP smear reduces the mortality and morbidity of cervical cancer. This cytological screening should gain much popularity and should be accessible to all. It is recommended as a part of routine medical examination in gynaecology practice. In present study it was seen that in management of patient majority 55% were given kit 2 with kit 6, 22% were given Counselling and were told to do regular vaginal wash, 9% had only kit 2, 6.5% had only kit 6, 4.5% were referred to cancer hospital, 1.5% were given acyclovir, 1% underwent polypectomy, and 0.5% had hysterectomy .In present study, among 15 cases of vaginal candidiasis 46.67% were given combined treatment, i.e. kit 2 and clindamycin vaginal pessary 33.33% were given oral i.e. Kit 2 and 20% were given clindamycin vaginal pessary. In study population all women are of rural background so because of lack of knowledge about genital area as well as due to poverty and illiteracy vaginal treatment is not much useful in treating candidiasis as compare to oral treatment. Perimenopausal discharge in gynaecology is not a new subject. But it needs increasing awareness and further attention. Since the problems are specific to this age group, setting up of PAP smear screening is desirable for efficient management.
CONCLUSION
- Incidence of vaginal discharge in perimenopausal women coming to the outpatient department of Gynaecology is 52.01%.
- Out of 200 number of cases of vaginal discharge 5 (2.5%) number of cases turned out to be malignancy and 23 (11.5%) turned to be premalignant lesion.
- Among the cause of vaginal discharge most frequent cause is infection 100 cases (50%) followed by leukorrhea 21%, non-malignant cervical lesion 13% and minimally consist of cervical malignancy 2.5% and atrophic vaginitis 2%.
- In treatment of vaginal discharge in absence of malignancy oral antibiotic are found to most effective All malignancy found out to cancer cervix for which radiotherapy is preferred choice.
ACKNOWLEDGEMENTS
Authors would like to thank Dr Shailesh Vaidya sir (associate Professor), Dr Ganesh Tondage sir (associate Professor and Head, Department of obstetrics and gynaecology Swami Ramanand Teerth Government Rural Medical College Ambajogai, Maharashtra, India), all staff personnel from Department of Obstetrics and Gynecology and all participants participated for their support during study.
Funding: No funding sources Conflict of interest: None declared Ethical approval: The study was approved by the Institutional Ethics Committee Swami Ramanand Teerth Government Rural Medical College, Ambajogai, Maharashtra, India
REFERANCES
-
Ian Donald et al.. etiology and investigation of vaginal discharge by institute of obstetrics and gynecology, university of London, British medical journal 12214 Dec. 6, 1952
-
Ralph M. Neighbor, Ralph M. Neighbor, Robert L. Newman et al.. Incidence of cervical cancer in perimenopausal and postmenopausal women detected by Papanicolaou smears St. Luke's Hospital, Kansas City, Missouri, USA. PlumX Metrics Volume 124, Issue 4, p327-444
-
N B Mirza, H Nsanze, L J D’Costa et al.., Microbiology of vaginal discharge in Nairobi, Kenya, Br J Vener Dis 1983;59:186-8
-
Verapol Chandeying, Steven Skov, Marisa Kemapunmanuset al.. et al.. Evaluation of two clinical protocols for the management of women with vaginal discharge in southern Thailand Sex Transm Inf 1998;74:194–201
-
Joharah M. A1 Quaiz, et al.. patients with vaginal discharge: a survey in a university primary care clinic in Riyadh city in annuals of Saudi medicine vol 20 nos 3-4 2000
-
Sabina Cauci, Silvia Driussi, Davide De Santo et al.. Prevalence of Bacterial Vaginosis and Vaginal Flora Changes in Peri- and Postmenopausal Women, journal of clinical microbiology, June 2002, p. 2147–2152 0095-1137/02/$04.000 2003
-
Michael Dan MD Nurit Kaneti MD, Daniel Levin MD e t al Vaginitis in a Gynecologic Practice in Israel Causes and Risk Factors Infectious Diseases Unit, Wolfson Hospital, Holon, Israel in 2003 published in BIMAJ 2003;5:629-632
-
A Hoosen et al.. studied that management of vaginal discharge CME Journal in February 2004. Vol. 22 no. 2
-
Matthew R. Anderson, Kathleen Klink, Andreas Cohrssen et al.. Evaluation of Vaginal Complaints, Medline database JAMA. 2004; 291(11):1368-1379. doi:10.1001/jama.291.11.1368
-
Hennew et al.. Vaginal discharge reviewed: the adult pre-menopausal female Department of Obstetrics and Gynecology, Stellenbosch University and Tygerberg Hospital, Tygerberg, in 2005. SA Fam Pract 2005;47(2)
-
Twinkle N. Gandhi, Manish G. Patel, Mannu R. Jain et al.. prospective study of vaginal discharge and prevalence of vulvovaginal candidiasis in a tertiary care hospital Department of Microbiology, SMIMER, Surat, Gujarat, India. Int J Cur Res Rev, Vol 7 Issue 1 January 2015 Research Article
-
Abdolali CHALECHALE, Isaac KARIMI et al.. The prevalence of Trichomonas vaginalis infection among patients that presented to hospitals in the Kermanshah district of Iran in 2006 and 2007*Turk J Med Sci 2010; 40 (6): 971-975
-
-
Des Spence, Catriona Melville et al.. Vaginal discharge in Dec 2007 BMJ 2007;335:1147-51
-
Bhalla P1, Chawla R, Garg S et al.. Prevalence of bacterial vaginosis among women in Delhi, India. Indian J Med Res. 2007 Feb; 125(2):167-72.
-
Sanjay N Parate, Arushi Gupta, Ashwini Wadadekar et al.. Cytological Pattern of Cervical Smears in Leukorrhea, India. International Journal of Scientific Study |, January 2017, Vol 4, Issue 1
-
T Rosita Verteramo Ettore Calzolari Anna Marta Degener Raffaele Masciangelo Alfredo Patella et al.. trichomonas vaginalis infection: Risk indicators among women attending for routine gynecologic examination April 2008 https://doi.org/10.1111/j.1447-0756.2007.00692.
-
P Madhivanan, K Krupp, V Chandrasekaran, et al.. prevalence and correlates of bacterial vaginosis among young women of reproductive age in Mysore, India, Indian J Med Microbiol. 2008 Apr-Jun; 26(2): 132–137.
-
-
A.Nandakumar, T. Ramnath and Meesha Chaturvedi et al.. The magnitude of cancer cervix in India, Indian J Med Res 130, September 2009, pp 219-221
Policy for Articles with Open Access:
Authors who publish with MedPulse International Journal of Gynaecology, (Print ISSN: 2579-0870) (Online ISSN: 2636-4719) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home
