|
Table of Content - Volume 15 Issue 1 - July 2020
Study of serum beta-HCG in second trimester as predictor of preeclampsia
Tripti Markam1*, Ishita Priyam Singh2, Bharati Misra3
1,2Post Graduate resident, 3Professor and HOD, Department of Obstetrics and Gynaecology, M.K.C.G. Medical college, Berhampur, Odisha, India. Email: trips.143@gmail.com
Abstract Background: Hypertensive disorders in pregnancy are one of the major causes of maternal morbidity and mortality. Hypertensive disorders in pregnancy account for 14% of all maternal deaths. An ideal predictor of the disease, the application of which could significantly alter the associated morbidity and mortality, remains elusive. Aim and objective: To study whether raised maternal serum beta hCG in second trimester is associated with increased incidence of Preeclampsia Methodology: 450 antenatal women carrying singleton pregnancy, fulfilling all inclusion and exclusion criteria were included in our prospective observational study. One venous sample were collected from each patient for beta hCG between 12-20 weeks. Patients followed up upto delivery. Outcome measured as development of preeclampsia during pregnancy. All relevant patient data and investigations were analysed statistically using Statistical version 16 [SPSS]. Results and discussion: The incidence of Preeclampsia was 26.88% in our study. In our study among 450 women, 121 developed PE with cut-off value of beta hCG value >82500 mIU/ml. The cut-off value for overall PE group and for mild preeclampsia group are same as 82500mIU/ml. Key Word: serum beta-HCG.
INTRODUCTION Preeclampsia is a potentially serious complication of pregnancy with increasing significance worldwide. Preeclampsia is a cause of 9-26% of global maternal mortality and a significant proportion of preterm delivery and maternal and neonatal morbidity. Worldwide preeclampsia and eclampsia are responsible for approximately 14% of maternal death per year.1 In India the prevalence of preeclampsia is 8% and it is second most common cause of maternal death after haemorrhage.2 Beta hCG is a glycoprotein, its molecular weight is 36000-40000 dalton. It consist alpha and beta subunits having 92 and 145 amino acid.3 Alpha subunit is biochemically similar to LH, FSH and TSH, where beta subunit is relatively unique to hCG. hCG is chemically and functionally similar to pituitary leutinizing hormone.4 Placental GnRH have control on hCG formation. Doubling Time of beta-hCG is 1.4 – 2 Days, The blood and urine value reaches maximum level ranging from 100-200 IU/ml between 60 – 70 days of pregnancy.4 Half life is 36 hours. The concentration falls slowly reaching a low levels of 10-20 IU/ml between 100-130 days, there after level remains constant throughout pregnancy with a slight secondary peak at 32 weeks. Normal level of hCG in nonpregnant state- 5mIU/ml, pregnant state- >25 IU/ml and in postmenopausal women- upto 14 IU/ml.5 In most normal pregnancy at hCG level below 1200mIU/ml the hCG levels usually doubles every 48-72 hours and normally increases by at least 60% every two days. In early pregnancy, a 48 hours increase of hCG by 35% can still be considered normal.6 Between 1200-6000 mIU/ml serum hCG level usually takes 72-96 hours to double. After 6000 mIU/ml it takes over four or more days to double.7-9 When it reaches 7200mIU/ml a yolk sac and in 10,800mIU/ml or greater than that a visible embryo with heart beat should be seen.10 Immunological response in preeclampsia developes in two stages. 1.Abnormal placentation and spiral artery remodelling – This is due to decreased placental HLA-G expression. HLA-G has a major role in placentation and blood flow development as observed in a normal pregnancy. There is a failure of extravillous trophoblast invasion and spiral artery remodelling. This is due to failure of interaction of extravillous trophoblast with uterine NK-cells and HLA-C receptors.11 2.Preeclampsia – It is associated with widespread systemic inflammation and endothelial dysfunction. The immune dysfunction are as follows:- There is decreases in regulatory T-cells both in number and function. There is insufficient shift from TH1 to TH2 as opposed to normal pregnancy where Th2 predominance is observed. There is a higher level of cytokinin abnormality with increased concentration of TNF-alpha, IL-6, IL-1beta, IL-8 and lower concentration of IL-10. In preeclampsia there is abnormal maternal-fetal immune interaction. Present study was conducted to see whether raised maternal serum beta hCG in second trimester is associated with increased incidence of Preeclampsia.
MATERIAL AND METHODS Present study was a Prospective observational study conducted in Department of OBGY, MKCG Medical College and hospital Berhampur during 2016-2018. Study population was Patient attending antenatal clinic of the department of obstetrics and gynaecology of MKCG Medical College and hospital Berhampur. Most of these patients came from in and around Ganjam district and consisted of both urban and semi urban population. The patients were mainly from low and middle income socioeconomic groups. Inclusion criteria: All antenatal patients between 12 – 20 weeks (as determined by LMP or Dating USG scan) with singleton pregnancy. 2. Patients willing to participate in the study Exclusion criteria: 1. Patients With multiple pregnancy 2. Patients With chronic hypertension or Known cases of diabetes mellitus 3. Patients With congenital anomalies 4. Patients With hydatidiform mole 5. Patients With intrauterine fetal disease 6. Patients who were Known case of hypothyroid or renal disease A total of 480 cases were selected out of which 450 patients completed the study and were followed till the end. Study was approved by ethical committee of the institute. A valid written consent was taken from patients after explaining study them. Data was collected with pre tested questionnaire. Data included demographic data, clinical history. A through clinical examination was done. Under aseptic precaution sampling was done by venipuncture, 5ml of blood was drawn out of which 3ml of blood was used for routine investigations and 2 ml of Blood for special investigations. Samples were collected once between 12-20 weeks. Serum β- hCG level was done by CLIA method (Chemiluminescence Immunoassay) between 12-20 weeks. Regular Blood Pressure monitoring with the same sphygmomanometer which is regularly calibrated was used. Blood Pressure measurement was done in semi supine position. The width of the cuff was kept large to avoid over diagnosis of hypertension. Keeping the rate of deflation to 2-3 mm Hg also prevented over diagnosing diastolic hypertension. Patients were followed up and outcome was noted. Data analysed with appropriate statistical tests.
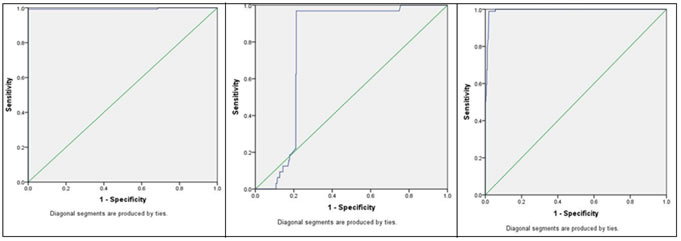
RESULTS Most of the patients (51.11%) attending the Antenatal clinic and included in our study were in the age group 20-25 years. Most of the patients (72.18%) in the study population were primigravida. Of the 450 patients followed, 121 women developed PE constituting a 26.88% of the study population. Thus, the incidence of Preeclampsia was 26.88% in our study. (table 1) When further subdivided, Out of these 121 Preeclamptic patients, 24 women had Early onset preeclampsia (onset < 34 weeks) whereas rest 97 had late onset (> 34 weeks) disease. About 60% women belonging to PE group had preterm delivery compared to 21% in case of normotensive group. These values were tabulated and analysed using Fischer’s exact test 2-tailed and the p value was statistically significant Majority of the women who developed PE were primigravida (about 78%). Only 21% of preeclamptic women were multipara. In our study we found that serum beta hCG were elevated in PE, more significantly elevated in severe PE when compared with normotensive group. This indicates that there exists an abnormal secretary function of the placenta in cases of PE. In our study among 450 women, 121 developed PE with cut-off value of beta hCG value >82500 mIU/ml. From ROC Curve analysis, Curve no- 1, it was found that for early second trimester(12-20weeks) beta hCG value above 82500mIU/ml, Sensitivity was 99.2% and specificity was 100% with a positive likelihood ratio of ∞ and negative likelihood ratio of 0.008. Next from ROC Analysis, Curve no -2, among mild PE group found that second trimester beta hCG value above 82500 mIU/ml, Sensitivity was 96.90% and specificity was 78.70%, with a positive likelihood ratio of 4.55 and negative likelihood ratio of 0.04. Lastly from ROC Analysis, Curve no -3, among severe PE group found that second trimester beta hCG value above 99950 mIU/ml, Sensitivity was 98.90% and specificity was 98.10%, with a positive likelihood ratio of 50.99 and negative likelihood ratio of 0.011. Table 1: Distribution of patients according to development of PE
Table 2: Distribution of patients according to severity of PE
Table 3: comparison of PE and Normotensive patients according to gestational age
Table 4: Statistical analysis according to mean B-HCG and age of patients (450)
ROC curve 1 ROC curve 2 ROC curve 3 ROC curve 1: ROC curve analysis for predicting PE on the basis of BHCG( 12-20 weeks); ROC curve 2: ROC curve analysis for predicting mild PE on the basis of BHCG( 12-20 weeks); ROC curve 3: ROC curve analysis for predicting severe PE on the basis of BHCG( 12-20 weeks)
Table 2: ROC Curve 2
Table 3: ROC Curve 3
DISCUSSION In our study of 450 patients, 121 patients developed Preeclampsia and rest 329 remained normotensive. The incidence of PE in our study was 26.88%. In their study of 164 cases, Vidyabati et al. found prevalence rate of PIH as 17.68% 114. Yadav et al. reported an incidence of PIH of 17.5% in 2014.12 Majority of the women who developed PE were primigravida (about 78%), in accordance with studies by other authors. Only 21% of preeclamptic women were multipara. Redman suggested that in later pregnancies there is development of protective immunologic mechanisms against paternal antigens.13 In an overview by Zuspan et al.. PIH occurs mainly in primiparous women (85%), who have 4-5 times higher risk than multiparous women.14 About 60% women belonging to PE group had preterm delivery compared to 21% in case of normotensive group. A prospective study done by Ye RW et al. 15 in China showed that PIH leads to preterm delivery and iatrogenic prematurity caused due to the necessity to terminate pregnancy. In our study among 450 women, 121 developed PE with cut-off value of beta hCG value >82500 mIU/ml. From ROC Curve analysis, Curve no- 1, it was found that for early second trimester (12-20weeks) beta hCG value above 82500mIU/ml, Sensitivity was 99.2% and specificity was 100% . Among mild PE group found that second trimester beta hCG value above 82500 mIU/ml, Sensitivity was 96.90% and specificity was 78.70%, with a positive likelihood ratio of 4.55 and negative likelihood ratio of 0.04. Among severe PE group found that second trimester beta hCG value above 99950 mIU/ml, Sensitivity was 98.90% and specificity was 98.10%, with a positive likelihood ratio of 50.99 and negative likelihood ratio of 0.011. Here the cut-off value for overall PE group and for mild preeclampsia group are same as 82500mIU/ml , it showes that this test is highly effective to diagnose PE, so it can be considered as a marker for prediction of PE in second trimester of pregnancy. This is similar to findings by Vidyabati et al.16 in 2010 that second trimester serum beta hCG levels increased significantly in those women who developed PIH and it has a predictive value. More recently , a California based study conducted by Towner D et al.17 and TacheV et al.18 in 2014 shows that adverse pregnancy outcome in terms of PIH/preeclampsia is more in women with elevated values although no specific cut off values have been mentioned in either study. Davidson EJ et al.19 in a retrospective case–control study in 2003, noted small but significant elevations in the concentrations of beta hCG in the second trimester serum of women who subsequently developed pregnancy-induced hypertension and pre-eclampsia. However, studies by Yadav K et al.20 and Pouta et al.21 did not observe any correlation between levels of beta hCG and development of PIH. The divergent points of maternal serum beta hCG with wide range of cut off values may be responsible for this result.
CONCLUSION Measuring serum beta hCG in early second trimester (12-20weeks) is a useful indicator to identify women who are likely to develop PE in the same pregnancy. Serum beta hCG value >82500mIU/ml can be considered as marker for predicting preeclampsia in second trimester of pregnancy. Also high levels are associated with increased severity of preeclampsia.
REFERENCES
Policy for Articles with Open Access:
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home