|
Table of Content - Volume 15 Issue 3 - September 2020
Study of etiological factors, maternal and foetal outcome in Oligohydraminos
Dantam Hymavathi Devi1, Ramana Bai Ramavath2*
1Associate Professor, 2Assistant Professor, Department of Gynaecology, Katuri Medical College & Hospital, Chinakondrupadu, Guntur, Andhra Pradesh, INDIA. Email: asyspoo664@gmail.com
Abstract Background: Oligohydramnios is a severe and common complication of pregnancy. Oligohydramnios has got significant impact on neonatal outcome and maternal morbidity. Aim and objective: To study the etiological factors, maternal and foetal outcome in patients with oligohydramnios. Methodology: Present study was a prospective study carried out in pregnant women presenting with oligohydramnios to Department of OBGY. Data was collected with pre tested questionnaire. Data included demographic data, clinical history and clinical examination. Obstetrical Ultrasound was done. All women were closely monitored throughout their antenatal, intrapartum and postpartum periods. Maternal and fetal outcome noted. Data was analysed with appropriate statistical test. Results: Majority of the patients in our study were from the age group of 20-25 years (55%) followed by 26-30 years (30%). In our study, 63% were in the gestation age of >37 weeks. Among 100 patients, 62% patients required caesarean section with Most common indication of foetal distress (72.58%) followed by CPD (12.91%). Low birth weight babies were 51.06%. APGAR score measured <7 at 1 minute in 62.76% and <7 at 5 minutes in 40.42% newborns. Key Word: Oligohydraminos.
INTRODUCTION During the intrauterine development, the foetus is surrounded by the amniotic fluid. Both maternal and foetal factors contributes to the development of liquor amnii.1,2 Queenan et al.3 described the correlation of AFV with fetal and placental weight in grams. Amount of AFV varies throughout the pregnancy. It increases from 1ml at seven weeks to 25ml at ten weeks, 400ml at 20 weeks reaches about 1 litre at 36 weeks. Thereafter it decreases progressively to about 800ml at term, as the pregnancy continues post term, further reduction occurs to the extent of 200ml at 42 weeks.4 Oligohydramnios is the condition in which the amount amniotic fluid is reduced to <200 ml at term. According to Phelan et al.5, if AFI <5cm it will be considered as oligohydramnios and Jeng et al. 6 considered it if AFI <8cm as oligohydramnios. amniotic fluid volume assessment is an useful method to identify the fetus at risk for adverse obstetric and perinatal outcome. Maternal factors associated with oligohydramnios are Preterm premature rupture of membranes, Uteroplacental insufficiency, Preeclampsia, Postdated pregnancy, Autoimmune disorders and Drugs like ACE inhibitors, PG synthesis inhibitors. Foetal factors contributing are Chromosomal abnormalities, Congenital anomalies, Intrauterine growth restriction, Intra uterine fetal demise and Fetal infections. Some of the placental factors are also responsible for oligohydramnios like abruption placenta.7,8 Maternal outcome is not affected adversely due to oligohydramnios. However maternal morbidity is indirectly increased by higher rate of induction and cesarean deliveries. Oligohydramnios also increase the caesarian section rate for fetal distress up to 41%. 9 Perinatal mortality and morbidity is significantly increased in oligohydramnios particularly if it occurs remote from term. Hence antepartum fetal surveillance is mandatory in pregnant women with Oligohydramnios. Present study was conducted to find out the etiological factors, maternal and fetal outcome in patients of oligohydramnios.
MATERIAL AND METHODOLOGY Present study was a prospective study carried out in department of OBGY at a tertiary health care centre. Study population was pregnant women presenting with oligohydramnios to Department of OBGY. Inclusion Criteria: 1. Women with Singleton pregnancy with AFI ≤ 5cm 2.women with gestational age 28-42 weeks 3. Women with intact membranes. Exclusion criteria: 1. Women with premature rupture of membrane 2. Intrauterine fetal death 3. Women with Post dated pregnancy. Study was approved by ethical committee of the institute. A valid written consent was taken from patients after explaining study to them. Data was collected with pre tested questionnaire. Detailed history including age, parity, previous menstrual history, last menstrual period, obstetric history were recorded. A through clinical examination was done. Clinical examination included blood pressure, BMI, cardiovascular and respiratory systemic examination and obstetric examination. The study population were subjected to a detailed history taking including age of the patient, parity, last menstrual period, previous menstrual history, obstetric history, past medical and surgical history, family history, personal history were taken. Followed by complete physical examination including general examination (including Ht, Wt, BMI, BP recorded at each visit, presence of anemia and pedal edema), cardiovascular and respiratory systemic examination, obstetric examination were done. Base line investigations like urine albumin, sugarand deposits, Hb%, OGCT, blood grouping and typing, HIV, VDRL, and HbsAg test were done. Obstetrical Ultrasound was done. In ultrasound, Fetal presentation, gestational age, liquor status, placental localization, and anomalies if present were noted. Amniotic fluid index was measured by the Phelan’s technique. In this technique uterus was divided into four quadrants by an imaginary lines drawn through the linea nigra and the umbilicus. Maximum deepest vertical pocket from the each quadrant was measured. Sum total of the four measurement gives the value of AFI. Women with AFI of ≤ 5 were considered as Oligohydramnios. All women were closely monitored throughout their antenatal, intrapartum and postpartum periods. Type of delivery, indication for casaerean section, intrapartum and post partum complications were noted. Foetal outcome was noted in terms of APGAR score, birth weight and mortality. Data was entered in Excel sheet and analysed using Statistical package for social sciences (SPSS v 21.0, IBM).
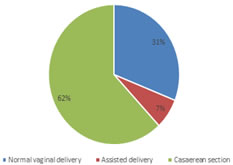
RESULTS Majority of the patients in our study were from the age group of 20-25 years (55%) followed by 26-30 years (30%). Patients above the age of 35 years were only 2%. (table 1) In our study, 64% of the cases in oligohydramnios group were primigravida, 34 % were second or third gravida. 2% of patients were 4th and above gravida. In our study, 63% were in the gestation age of >37 weeks, 30% between 33-37 weeks and 7% between 28-32 weeks. In our study, 37% were isolated oligohydramnios with no identifiable cause, 30% were post dated pregnancy, 11% were IUGR, 17% were hypertensive diseases, 4% were congenital anomalies. (table2) Among congenital anamolies, infantile polycystic kidney disease, MCKD, Single umbilical artery and microcephaly was seen. Out of total 100 patients 65% were induced and 35% had spontaneous onset of labour. Among 100 patients, 62% patients required caesarean section, 31% patients were delivered by normal vaginal delivery. 7% patients delivered by assisted delivery. (fig 1) Among the indications for caesarean section in oligohydramnios. Most common indication for caesarean section was foetal distress (72.58%) followed by CPD (12.91%). Failed induction (8.06%) and malpresentation (6.45%) were other indication. (table 3) In our study we found that non stress test was non reactive in 53% patients and was reactive in 47% patients. Doppler ultrasound findings showed 22 % abnormal patterns. It included decreased diastolic flow in umbilical artery or increased diastolic flow in middle cerebral artery. (table 4) Table 5 shows distribution of oligohydramnios patients according to foetal outcome. Out of 100 patients 94 were alive. There were 6 perinatal deaths. Cause of death were Meconium Aspiration Syndrome (2), Hyaline membrane disease (2)and septicaemia (2). 3 of these 6 were premature. In our study, majority of the newborns had birth weight ≤ 2.5 kg (51.06%) followed by 2.6 to 3 kg (29.79%). Newborns with weight of 3.1-3.5 kg were 11.70% and 3.6-4 kg weight was observed in 7.45% newborns. None of the newborn weighed above 4 Kgs. Thus low birth weight babies were 51.06%. We calculated APGAR score of these newborns. It measured <7 at 1 minute in 62.76% and <7 at 5 minutes in 40.42% newborns.
Table 1: Distribution of oligohydramnios patients according to age group
Table 2: Distribution of oligohydramnios patients according to etiological factors
Figure 1: Distribution of oligohydramnios patients according to mode of delivery
Table 3: Distribution of oligohydramnios patients according to indications of Caesarean section
Table 4: Distribution of oligohydramnios patients according to maternal outcome
Table 5: Distribution of oligohydramnios patients according to foetal outcome
DISCUSSION Majority of the patients in our study were from the age group of 20-25 years (55%) followed by 26-30 years (30%). This is comparable to Guin et al. 10 study in 2011 Similar findings were seen in Biradar KD et al. and Patel PK et al.. in contrast to our study Vidyasagar et al. showed 80.49% patients were from the age group of 20-25 years .11-13 In our study, 64% of the cases in oligohydramnios group were primigravida, 34 % were second or third gravida. 2% of patients were 4th and above gravida. Similar findings were seen in Vidyasagar V et al. 13 and Biradar KD et al. 11 In our study, 63% were in the gestation age of >37 weeks, 30% between 33-37 weeks. It is comparable with the study conducted by Moses V et al.. 14 This may be due to either uterine insufficiency or reduced fetal urine production. In our study, 37% were isolated oligohydramnios with no identifiable cause, 30% were post dated pregnancy, 11% were IUGR, 17% were hypertensive diseases, 4% were congenital anomalies. Among congenital anamolies, infantile polycystic kidney disease, MCKD, Single umbilical artery and microcephaly was seen. The study conducted by Maryam A et al.15, found that preeclampsia is highly associated during pregnancy. Similarly, the study conducted by Sasahara J et al..,16 found that Preeclampsia and PROM show more risk to oligohydramnios. In our study, Out of total 100 patients 65% were induced and 35% had spontaneous onset of labour. Among 100 patients, 62% patients required caesarean section. Similar study done by Biradar et al. 11 found 62% incidence of caesarean section. Other studies showed different results like Sowmya K et al. (50%) Bansal D et al. (47%) and Golan et al. (35.2%). 17-19 We found that Most common indication for caesarean section was foetal distress (72.58%) followed by CPD (12.91%). Similar results were seen in the study conducted by Moses et al. 14 and Padma S et al.. 20 In our study low birth weight babies were 51.06%.in study by Biradar et al. 11 38.6% low birth weight babies were seen. In our study APGAR score measured <7 at 1 minute in 62.76% and <7 at 5 minutes in 40.42% newborns. Similar study done by Sriya V et al. and Zhang J et al. found APGAR score <7 at 1 minute in 38.8% and 13.3% respectively.21,22
CONCLUSION Oligohydramnios are associated with high maternal and fetal complications. Timely intervention by an obstetrician will help to reduce maternal and fetal complications.
REFERENCES
Policy for Articles with Open Access:
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home