|
Table of Content - Volume 15 Issue 3 - September 2020
Comparative study between intravenous paracetamol infusion versus intramuscular tramadol as intrapartum labor analgesic
Neha Majotra¹*, Aakash Jerath², Priyanka Parihar3, Surinder Kumar4
1,3Post Graduate Resident, ²Registrar Medicine, 4Professor & HOD, Department of Obstetrics & Gynaecology, SMGS Hospital, Government Medical College, Jammu, INDIA. Email: drnehamajotra15@gmail.com
Abstract Background: This study was done to compare the efficacy of intravenous paracetamol infusion and intramuscular tramadol injection as labour analgesic. Method: This prospective-randomized study was conducted in 200 primigravidae at term pregnancy in active labour, distributed into two groups of 100 women each receiving single dose of intravenous 1000mg Paracetamol and other 100mg intramuscular tramadol. Pain intensity was recorded by Mc Gills pain intensity scale before, one and three hours after drug administration. Labour events were recorded in partograph. Perinatal outcome and maternal complications were observed. Results: No difference in pain intensity is seen before drug administration. After 1 h of drug administration, in paracetamol group, 5% women had horrible pain, and 45% had distressing pain, while in tramadol group, 19% women had horrible pain and 66% had distressing pain. After 3 h of drug administration, in paracetamol group, 18% had distressing pain, while in tramadol group, 21 % women had horrible pain and 57% had distressing pain. Labor duration in paracetamol and tramadol group was 4.3h and 6.2 h, respectively. In paracetamol group, nausea is seen in 3% and vomiting in 3%, while in tramadol group, nausea is seen in 7% and vomiting in 5%. Conclusion: Intravenous paracetamol is more effective labor analgesic with fewer maternal adverse effects and shortens labor as compared to intramuscular tramadol. Keywords: Intravenous paracetamol, Intramuscular tramadol, Labor analgesic.
INTRODUCTION Labor pain is among the most excruciating pain experienced by women. Labor pain affects maternal psychology and course of labor causing apprehension, anxiety, and stress. Pain during the first stage of labor originates predominantly due to cervical dilatation and uterine muscle wall ischemia leading to lactate accumulation. During the late first stage and second stage of labor, the vagina and perineum form additional sources of pain. The associated increase in sympathetic activity leads to increased oxygen consumption, respiratory alkalosis, and metabolic acidosis which could lead to decreased oxygen being transferred to the fetus. Thus, pain relief during labor is expected to reduce maternal stress and improve maternal and perinatal outcome1. Obstetric analgesia and anaesthesia have evolved from vague possibility to reality. The non-pharmacological techniques of analgesia include emotional support, relaxed birth environment, psycho-somatic preparation, yoga, acupuncture, and transcutaneous electrical nerve stimulation (TENS). 2The commonly used and more effective are pharmacological techniques include opioids like pethidine and tramadol though the regional analgesia is gold standard nowadays and routinely used in modern obstetric anaesthesia in developed countries. The newer advances like combined spinal epidurals, low dose epidurals, patient-controlled intravenous, inhalational, and epidural analgesia have revolutionized obstetric anaesthesia. But most of modern obstetric analgesia practices involve participation of expert anaesthesiologist, costly equipment, and continuous monitoring facilities which unfortunately cannot be available in routine obstetric practice in the developing countries where a majority of obstetric services are in the hands of midwives, trained nurses, and non-specialist doctors. In such situations, a method with minimum technicality is desired. Paracetamol, the mode of analgesic action of which has still not been fully elucidated but probably is a centrally acting drug which inhibits prostaglandin synthesis, has recently been made available as intravenous preparation. 2,6Various studies have proved intravenous paracetamol as effective analgesic agent which is safe, effective, inexpensive, and requires no special monitoring . However, there are no significant trials regarding paracetamol analgesic effect on labor pain in women. If proved to be an effective analgesic agent in labor, paracetamol being inexpensive and simple to administer could be a boon agent of obstetric analgesia in developing countries. Only a few studies have documented safety and efficacy of intravenous paracetamol as a labor analgesic . 4-7Tramadol hydrochloride is a centrally acting analgesic opioid. Intramuscular tramadol hydrochloride is commonly used in labor analgesia in developing countries as it is inexpensive; no special monitoring is required and has been widely studied and proved for its safety and efficacy in labor analgesia . There is no study comparing these two as labor analgesics. So, we undertook this study with the aim to compare efficacy and safety of single dose 1,000 mg intravenous paracetamol with 100 mg intramuscular tramadol hydrochloride as labor analgesic in primigravidae women during active phase of labor.
MATERIALS AND METHODS The study was conducted in the Postgraduate Department of Obstetrics and Gynaecology, SMGS Hospital, Government Medical College, Jammu for a period of one year during 2018-2019.Two hundred (200) primigravidae women in age group 20-35 yrs were selected from those who were admitted in obstetrics emergency ward of SMGS Hospital. The particulars of the patients were noted according to prescribed proforma. INCLUSION CRITERIA:
(Active phase of labour is described as cervical dilatation more than or equal to 3cm, cervical effacement more than or equal to 60% and uterine contractions.) EXCLUSION CRITERIA: -Gestational age <37 completed weeks
This study was single –blinded prospective randomised study . Informed consent was taken from the subjects . The women were randomly distributed in two Groups; paracetamolgroup-100 women and tramadol group- 100 women. All the women in paracetamol group received 100 ml intravenous infusion; Containing 1000 mg of paracetamol single dose over 15 min. All the women in tramadol group received100 mg intramuscular single dose in upper and outer quadrant of gluteal region with a 2ml syringe. Pain intensity before administering drug was recorded by Mc Gills pain intensity scale. Women included in study, were evaluated with detailed history, general physical examination and obstetric examination, including vaginal examination were done and all the required investigations were carried out. Labour was monitored using partograph (paperless). Measurement of pain relief was done with measurement of pain relief was done with Mc Gills pain intensity scale after 1 and 3 h of drug administration. Foetal monitoring was done using a non-stress test. Mode of delivery, neonatal outcome, duration of labour, drug delivery interval and side effects of drugs in both the groups were noted. At the end of study, data was compiled and analysed using t-test and chi-square Statistical Test. The pain scale used in the study was “Mc Gills pain intensity scale”.
Table 1: Mc Gills pain intensity scale
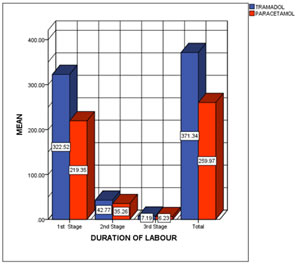
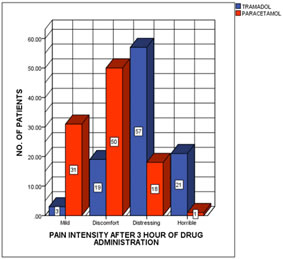
RESULTS The mean age of women in Tramadol group was 25.71±3.32 years and the mean age of women in Paracetamol group was 26.21±3.07 years. The difference was not statistically significant between the two groups (p=0.27).The mean gestational age of women in Tramadol group was 38.76±1.05 years and the mean age of women in Paracetamol group was 38.50±1.52 years. The difference was not statistically significant between the two groups(p=0.16).The mean dilatation of women in Tramadol group was 3.55±0.62 cm and the mean dilatation of women in Paracetamol group was 3.59±0.64 cm. The difference was not statistically significant between the two groups(p=0.65). The mean effacement of women in Tramadol group was 67.9±7.56% and the mean effacement of women in Paracetamol group was 68.1±8.35%. The difference was not statistically significant between the two groups(p=0.858). Using Mcgills pain intensity scale, 32 women (32%) in the Paracetamol group had horrible pain, 64 women (64%) had distressing pain and 4 women (4%) had discomfort at the point of entry into the study. In the Tramadol group, 24 women (24%) had horrible pain, 66 women (66%) had distressing pain and 10 women (10%) had discomfort. The pain intensity using Mcgills scale between the two groups before drug administration was statistically insignificant (p =0.15).After 1 hour of intravenous Paracetamol administration, 5 women (5%) had horrible pain, 45 women (45%) had distressing pain, 45 women (45%) had discomfort and 5 women (5%) had mild pain. In the Tramadol group, 19 women (19%) had horrible pain, 66 women (66%) had distressing pain, 15 women (15%) had discomfort after 1 hour of drug administration. The difference in the two groups was statistically significant. (p=0.001).After of Paracetamol administration, 1 woman (1%) had horrible pain, 18 women (18%) had distressing pain, 50 women (50%) had discomfort and 31 women (31%) had mild pain. In the Tramadol group, 21 women (21%) had horrible pain, 57 women (57%) had distressing pain, 19 women (19%) had discomfort and 3 women (3%) had mild pain after 1 hour of drug administration. The difference in the two groups was statistically significant. (p=0.001).Women who had lower segment caesarean section (LSCS) were excluded for comparison of duration of labor. 8 women in the paracetamol group had LSCS, and 9 women in the tramadol group had LSCS. The mean duration of the active phase of first stage of labour in the Paracetamol group was 219.35 ±15.27 min (3.6 ±0.3 h) and the Tramadol group was 322.52 ±20.96 min (5.4 ±0.3 h). The difference in the mean duration of the active phase of first stage of labour between the Paracetamol and Tramadol groups was statistically significant (p=0.0001).The mean duration of the second stage of labour in the Paracetamol group was 35.26 ±5.13 min and in the Tramadol group was 42.77±2.09 min. The difference in the mean duration of second stage of labour between the Paracetamol and Tramadol groups was statistically significant (p=0.0001).Total duration of labour from enrolment in study to delivery in the neomol group was 259.97 ± 14.47 min and in the Tramadol group was 371.34 ± 19.50 min. The difference in the total duration of labour from enrolment in study to delivery between the Paracetamol and Tramadol groups was statistically significant (p=0.0001).Drug to delivery interval in the Paracetamol group was 2.93±0.0.46 h and in the Tramadol group was 3.18±0.44 h. The difference in the two groups was significant (p=0.0001).
Figure 1: Comparison of duration of labour in different stages of labour (min)
Table 2: Pain intensity of the women in paracetamol and tramadol group using McGills scale
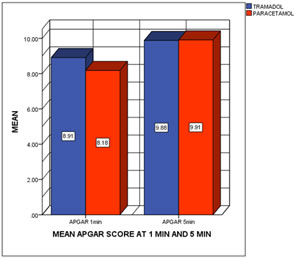
Figure 2 Figure 3 Figure 4 Figure 5 Figure 2: Comparison of pain intensity before drug administration in both the groups; Figure 3: Comparison of pain intensity after 1 hr of drug administration in both the groups; Figure 4: Comparison of pain intensity after 3 hr of drug administration in both the groups; Figure 5: Comparison of mean Apgar at 1 and 5 min in both the groups
The mean Apgar score of neonates in the Paracetamol group at 1 min was 8.39±1.02 and at 5 min was 9.91±0.35. The mean Apgar score of the neonates in the Tramadol group at 1 min was 8.47±1.10 and at 5 min was 9.88±0.36. The difference was statistically insignificant (p=0.55).The mean birth weight was 2.62±0.32 kg in the Paracetamol group and 2.54±0.25 kg In the Tramadol group. The difference was statistically insignificant between the two groups (p=0.0502). In the Paracetamol group, nausea was seen in 3% followed by vomiting in 3%. Nausea was the most common side effect in the tramadol group(7%) followed by vomiting (5%).No women in the Paracetamol and Tramadol group had respirator depression, foetal tachycardia. Foetal bradycardia was seen in 2% in the paracetamol group and 1% in tramadol group. One women in the Tramadol group had PPH. The differences in nausea and vomiting were statistically insignificant between the two groups. In Paracetamol group, 92 % women had vaginal delivery as compared to Tramadol group about 91% had vaginal delivery. One woman in the Paracetamol group, had ventouse assisted vaginal delivery. 8 women in the Paracetamol group had LSCS and 9 women in the Tramadol group had LSCS.
DISCUSSION The probable mode of analgesic action of intravenous paracetamol is peripheral and central inhibition of COX and/or interaction with the serotonergic system. One gram of intravenous paracetamol should only be given when weight is more than 33 kg, and hepatic disorders are ruled out. It should not be repeated within 4 h and must not exceed four grams in 24 h . Tramadol is a pethidine like synthetic opioid having low affinity for opioid receptors, and unlike other opioids, it inhibits reuptake of noradrenaline and 5-hydoxytriptomin. It has no clinically significant respiratory depression at usual doses of 1–2 mg/kg body weight; however, concerns have been voiced over high placental permeability of tramadol and side effects like nausea, vomiting, and delayed gastric emptying which could lead to risk of aspiration; in case, general anaesthesia is required in an emergency situation. The findings of the present study suggest that paracetamol group had a significant decrease in pain intensity 1 and 3 h after intravenous paracetamol administration as compared to intramuscular tramadol group. About 75 % women in the paracetamol group had substantial relief of pain which lasted for 3 h. This might be explained by the fact that peak analgesic effect of paracetamol is seen at 1 h, and effect lasts for 4 to 6 h, while for intramuscular tramadol, onset is within 10 min, and action lasts for 2–3 h. Previously too, there have been concerns about analgesic effectiveness of tramadol as it is thought that its perceived analgesic efficacy may be due to at least in part, to its sedative effect rather than true reduction in perceived pain .There was a statistically significant reduction in the duration of first, second, and third stages of labor after administration of intravenous paracetamol. Hence total duration of labor was reduced in patients who received paracetamol as compared to tramadol. Drug to delivery interval as stated earlier was 2.93±0.0.46 h in paracetamol group and 3.18±0.44 h in tramadol group. A probable reason to explain that this could be the fact that tramadol causes sedation, although lesser than other opioids, leading to lesser mobility of women in labor which could lengthen the labor. Also lesser pain relief as compared to paracetamol group could be a cause of lengthened labor in these women. More studies are required to elucidate the effect of intravenous paracetamol on labor duration, because a decrease in labor duration has multiple potential benefits and better maternal and perinatal outcome. Neonatal outcome was favorable with both paracetamol and tramadol. However, side effects like nausea and vomiting were observed more in tramadol group, but no other major complications occurred with any of the drugs. In a study by Elbohoty et al.. in 2012, intravenous paracetamol infusion was compared with intravenous pethidine for labor analgesia. It was concluded that effectiveness of intravenous paracetamol and duration of action are comparable in both drugs, but paracetamol was associated with a fewer maternal side effects and also shortened labor . In another study by Abdollahi et al.. in 2014, comparing intravenous paracetamol with intramuscular pethidine, it was concluded that intravenous paracetamol was more effective. But no shortening of labor was observed with intravenous paracetamol and no difference in maternal and neonatal outcome . In a study by Lallar M et al.. in 2015, comparing Intravenous Paracetamol Infusion Versus Intramuscular Tramadol as an Intrapartum Labor Analgesic found intravenous Paracetamol is more effective labour analgesic than intramuscular Tramadol. However, there are limited studies available comparing intravenous paracetamol with intramuscular tramadol for labor analgesia in our knowledge, but it has already been seen in many studies that tramadol is a weaker labor analgesic than pethidine but has a better safety profile. More studies are required to elucidate the analgesic profile of intravenous paracetamol in labor as on initial studies it appears to be quite promising.
CONCLUSION Findings from our study demonstrate that intravenous Paracetamol is more effective labour analgesic than intramuscular Tramadol. Paracetamol also shortens the length of labour and has fewer maternal adverse effects than Tramadol. However, the neonatal outcome of both the drugs is favourable. So from our study, we can conclude that intravenous Paracetamol is simple, cost effective feasible option as labour analgesic. In developing countries with low health care resource settings, intravenous Paracetamol can be used as a labour analgesic instead of intramuscular Tramadol due to its better analgesic action, shortening of labour and fewer maternal side effects.
REFERENCES
Policy for Articles with Open Access:
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home