|
Table of Content - Volume 16 Issue 1 - October 2020
Safety and feasibility of non-descent vaginal hysterectomy (NDVH): A prospective study
Sanubar Rehman1, Shyamkumar Sirsam2*
1Resident, 2Professor & HOD, Department of Obstetrics and Gynaecology, Government Medical College, Akola, Maharashtra, INDIA. Email: sanubarrehman@gmail.com
Abstract Background: Among women undergoing hysterectomy for benign disease, non-descent vaginal hysterectomy appears to be superior other techniques, as it is associated with faster return to normal activities. So, we conducted a study, to evaluate the feasibility and safety of non descent vaginal hysterectomy among the patients with benign conditions in our institute. Methodology: A prospective study was conducted among patients undergoing NDVH for benign uterine pathology attending the Department of Obstetrics and Gynaecology of a tertiary care hospital Maharashtra. The study duration was from November 2017 to October 2019. Cases needing hysterectomy for benign conditions, uterine size ≤12 weeks, no history of active infection and PAP smear negative for intra epithelial lesions were included in the study. Cases with suspected adnexal pathology, endometriosis, immobile uterus and genital malignancy were excluded from the study. After detailed evaluation and pre anesthetic checkup about 150 patients underwent NDVH. Intra operative and post operative complications were noted and analysed. Results: Majority of them were AUB-L (48%) in the present study. Entire removal of the uterus was done 66.00% cases which were in majority of the case. About 2.00% had bladder injury, 2.67% had haemorrhage and one case had rectal injury intra operatively. About one case each had fever and RV fistula; three cases had spinal headache and vault discharge and rest did not have any post operative complications. The mean duration of the hospital stay was 3.41 ± 0.86 days with range of 3 to 8 days. Conclusions: The blood loss was less among the patients who underwent this procedure. Intra operative complications were less with most common ones including the bladder injury and haemorrhage. Considering the indication frame, NVDH is one of the best hysterectomy techniques in terms of less complications and faster recovery. Key words: Benign lesions; Non descent vaginal hysterectomy; Safety
INTRODUCTION Non descent vaginal hysterectomy is considered safe for benign uterine conditions1. This technique was first performed by Haene’y in 1934. Among women undergoing hysterectomy for benign disease, non-descent vaginal hysterectomy appears to be superior to laparoscopic hysterectomy and abdominal hysterectomy, as it is associated with faster return to normal activities. On the other hand, vaginal hysterectomy can be performed under regional anaesthesia, with lower healthcare costs, with lesser complications and faster recovery2,3. It is preferred in obese patients and in patients in whom the risks of general anaesthesia are higher. It is also more cosmetic as there is no scar. Furthermore, chances of ureteric injury, bladder injury, paralytic ileus and haemorrhage are less in the vaginal route when compared with abdominal routes3. When technically feasible, vaginal hysterectomy should be performed in preference to abdominal hysterectomy because of more rapid recovery and fewer febrile episodes postoperatively1. This approach is preferred in the patients who are overweight and obese4,5. However, the success of the procedure depends on the proper selection of cases and the learning curve of the technique among the gynaecologists. With this background we conducted a study, to evaluate the feasibility and safety of non descent vaginal hysterectomy among the patients with benign conditions in our institute.
MATERIALS AND METHODS A prospective study was conducted among patients undergoing NDVH for benign uterine pathology attending the Department of Obstetrics and gynaecology of a tertiary care hospital Maharashtra. The study duration was from November 2017 to October 2019. Cases needing hysterectomy for benign conditions, uterine size ≤12 weeks, no history of active infection and PAP smear negative for intra epithelial lesions were included in the study. Cases with suspected adnexal pathology, endometriosis, immobile uterus and genital malignancy were excluded from the study. A pilot study was conducted on 50 study subjects and found that the most common indication of NDVH was AUB-L and that accounted for 35% of the cases. Using this proportion, with 95% confidence interval and 10% absolute error we found the minimum sample size to be 143. For our convenience we included 150 study subjects in the present study which fitted the eligibility criteria of the protocol. Written informed consent was taken from patients for evaluation. All the patients included in the study were subjected to detailed history and clinical examination. All the preoperative investigations including Hb, CBC, Renal and Liver function tests, HIV, HbsAg, Ultrasonography, PAP smear were done. Fitness was attained and patient was posted for NDVH. One dose of antibiotic was given pre operatively. Antibiotics were continued upto postoperative day 3. Pre anaesthetic evaluation was done before the surgery. All the patients posted for NDVH were operated under regional anaesthesia, spinal. After cleaning and draping, Sims speculum was inserted and cervix was held with vulsellum. Hydrodissection was done while a few cases were operated without hydrodissection. Circumferential incision was taken around the cervix, and pubo-vesico-cervical ligament was cut and bladder pushed up. Both anterior and posterior pouches were opened. Uterosacral and cardinal ligaments were clamped, cut and ligated. Bilateral uterine arteries were clamped cut and ligated. The next step depended upon the size of the uterus. Uterine bisection, myomectomy, coring, debulking or combination of these is effective morcellation techniques which were performed when required. Lastly uterine cornual structures containing round ligament, ovarian ligament and fallopian tube were clamped, cut and ligated to deliver specimen out. Specimen was sent for histopathology. Data regarding age, parity, uterine size, removal technique, blood loss, time of surgery, intra operative and postoperative complications, and hospital stay were analysed and evaluated. Time required for surgery was calculated from the first incision till complete vault closure. Blood loss during surgery was noted by the number of mops used. On an average one fourth soaked mop contained 50ml, one half soaked 100ml and fully soaked mop contain 200ml of blood. Post operative pain was measured as per visual analogue pain scale and pain score was calculated for each patient. Statistical analysis: All the data was collected and entered in Microsoft Excel. The data was analysed using Epi info version 7.2. The qualitative data was expressed in terms of percentages and to test the difference between two proportions chi square or fisher’s exact test has been used. The quantative data was expressed in terms of mean and standard deviation. All the analysis was 2 tailed and the significance level was set at 0.05.
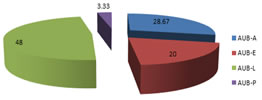
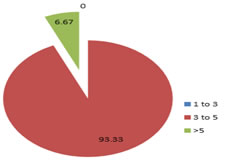
RESULTS We included 150 cases of non descent vaginal hysterectomy in the present study. Insert table 1 here— The mean age of the study subjects was 44.26 ± 4.83 years with range of 38 to 60 years. Majority of them were in the range of 41 to 45 years. About 38.00% were having parity of one, 34.00% had parity of two, 24.67% had parity more than three and 3.33% were primipara in the present study. About 3.33% had having normal uterus size, 18% were 6 weeks, 38.67% were 8 weeks, 26% were 10 weeks and 14% were 12 weeks in the present study. Insert chart 2 here— About 48.00% were AUB-L, 28.67% were AUB-A, 20.00% were AUB-E and 3.33% were AUB-P in the present study. Insert table 3 here— Entire removal of the uterus was done 66.00% cases which were in majority of the case. 14.67% underwent bisection, 6.67% underwent bisection + Myomectomy, and 6.00% underwent Myomectomy. 4.00% underwent debulking and 2 each cases underwent coring and bisection + polypectomy in the present study. About 89.33% of the patients underwent hydro dissection. The mean blood loss was 155.07ml with a range between 100ml to 300ml and a standard deviation of 54. About 2.00% of the cases were converted to TAH. The mean duration of surgery was 54.73 ± 12.68 minutes with range of 30 to 120 minutes. Majority of the timings were in the range of 45 to 90 minutes in the present study. Insert table 4 here— About 2.00% had bladder injury, 2.67% had haemorrhage and one case had rectal injury intra operatively. About one case each had fever and RV fistula; three cases had spinal headache and vault discharge and rest did not have any post operative complications. About 57.67% had pain score of less than 3, 42.00% had pain score of 3 to 5 and 1.33% had pain more than 5 in the present study. Insert chart 5 here— The mean duration of the hospital stay was 3.41 ± 0.86 days with range of 3 to 8 days. Majority of them had less than 5 days of hospital stay. Insert table 6a here— The mean blood loss among AUB-A was 152.33ml, AUB-E was 120.00ml, AUB-L was 173.57ml and AUB-P was 130ml in the present study. There was significant difference between the blood loss among the different diagnosis. Insert table 6b here— The blood loss among the cases with hydro dissection was 155.30ml and cases without hydro dissection were 153.15ml and this difference was not statistically significant. Table 1: Demographic particulars of the study sample
Chart 2: Distribution of the study subjects based on diagnosis
Table 3: Distribution of the study subjects based on procedure done
Table 4: Distribution of the study subjects based on complications in study subjects
Chart 5: Duration of hospital stay in study subjects
Table 6a: Distribution based on the blood loss among different diagnosis
Table 6b: Distribution based on the blood loss with use of hydro dissection
Table 7: Comparison of blood loss among the different studies
DISCUSSION For most of the 20th century, the two modalities used to perform surgical removal of the uterus included the total abdominal hysterectomy and vaginal hysterectomy. The evidence detailing the differences in patients’ experience between these two approaches was notable. Non descent vaginal hysterectomy had advantages over the abdominal hysterectomy and laproscopic hysterectomy1,2. With this background, we conducted a study to evaluate the non descent vaginal hysterectomy cases in our setup. The mean age of the study subjects was 44.26 ± 4.83 years with range of 38 to 60 years. Majority of them were having parity of less than 2 and size of uterus was normal in about 3.33% of the cases. Majority of the cases in the present study were AUB-L (48%) followed by AUB-A (28.67%). Similar inferences were reported by study conducted by Shanti S et al..6 (2017). Dysfunctional uterine bleeding and fibroid uterus were the most common indications for hysterectomy in the studies conducted by Murali MS et al..7 (2019), Patil VM et al.8 (2015), Saha R et al..9 (2012), Zahan A et al..10 (2015), Shinde S et al..11 (2015) and Mishra N et al..12 (2017). The most common removal technique of the procedure in the present study was complete removal of uterus in 66%. About 14.67% underwent bisection, 6.67% underwent bisection + Myomectomy, and 6.00% underwent Myomectomy. 4.00% underwent debulking and 2 each cases underwent coring and bisection + polypectomy. Saha R et al..9 (2012) reported about 43 cases had bisection, 19 cases had Myomectomy and 5 cases were described as morcellation technique in their study. Shinde S et al..11 (2015) reported about 24% underwent bisection, 18% had bisection with enucleation of myoma and 8% morcellation/wedge resection. Zahan A et al..10 (2015) reported about 22% cases underwent bisection, 14% had Myomectomy and 6% had slicing and de bulking. Shanti S et al..6 (2017) reported that among 25 cases, 11 cases had bisection, one case had Myomectomy, five cases had coring and four cases had coring and Myomectomy in their study. Mishra N et al..12 (2017) reported that about 53.84% underwent bisection with Myomectomy, 17.94% bisection only, 16.66% had bisection with morcellation and 11.53% had removal of intact uterus. Ramesh kumar R et al..14 (2018) inferred that combination of the debulking techniques was used in 90% of the cases with myomectomy being the most common single debulking technique used in 61.5% of the cases followed by coring in 36.9% of the cases. Dewan R et al..15 (2004) reported that morecellation techniques were employed in 32 cases (64%). Insert table 7 here--- Majority of the studies had average blood loss with was comparable with our study. An interesting thing to note was the blood loss among the cases with hydro dissection was 155.30ml and cases without hydro dissection were 153.15ml and this difference was not statistically significant. Among AUB-A cases the blood loss was significantly higher when compared with other types of AUB in the present study. About 2.00% had bladder injury, 2.67% had haemorrhage and one case had rectal injury intra operatively. Saha R et al..9 (2012) reported that among 50 cases studied, 3 cases had difficulty in opening the pouch of douglas and four cases had difficulty in reaching myoma. Zahan A et al..10 (2015) reported that about 42% had difficulties during the procedure. Hiran Chaminda SH et al..16 (2015) reported that one case needed blood transfusion due to haemorrhage in their study. About one case each had fever and RV fistula; three cases had spinal headache and vault discharge and rest did not have any post operative complications. Saha R et al..9 (2012) reported that about ten cases had post operative pain, two cases had fever and seven cases had haemorrhage requiring transfusion. Gayatri SB et al..13 (2017) reported that there was bladder injury in a patient with 2 previous LSCS and rectal injury due to large fibroid with difficult extraction post operatively with fecal fistula possibly due to unwanted pressure on the rectum by the speculum. Failure of NDVH was due to inaccessible fundal fibroid in two cases. Mishra N et al..12 (2017) reported that about 2.56% had conversion to TAH, 1.2% had primary haemorrhage, 1.28% vault haematoma, 10.25% had pyrexia, 5.12% urinary tract infection and 1,28% had urinary tract fistula. Zahan A et al..10 (2015) reported that about 2% had bladder injury, 4% had vaginal cuff infection, 6% had secondary haemorrhage and 8% had urinary tract infection. Shanti S et al..6 (2017) reported that about two cases had fever, two cases had urinary tract infection and one case had retention of urine. Ramesh kumar R et al..14 (2018) reported that only 5 cases had post-operative complications. Blood transfusion was required in 2 cases and 3 cases had post-operative fever. Surgical challenges were faced in two thirds of the cases (64.6%). There were 15 cases with previous lower segment cesarean section and 12 cases of nulliparity. Adenexal pathology was seen in 10 cases and 5 cases had cervical or isthmic fibroid. Hiran Chaminda SH et al..16 (2015) reported that about 1.8% of the cases had urinary tract infection in their study. Similar inferences were reported by studies conducted by Patel A et al..17 (2015) and Shinde S et al..11 (2015) The mean duration of the hospital stay was 3.41 ± 0.86 days with range of 3 to 8 days. Studies conducted by Zahan A et al..10 (3.1 days), Shanti S et al..6 (4-5 days), Gayatri SB et al.13 (3 days) and Dewan R et al..15 (3 days) had concordant inferences with our study. The mean duration of surgery was 54.73 ± 12.68 minutes with range of 30 to 120 minutes. Studies by Shanti S et al..6 (60 minutes), Gayatri SB et al..13 (90 minutes), Ramesh kumar R et al..14 (50% of the cases had less than 90mins), Dewan R et al..15 (54.5minutes) and Murali MS et al..7 (40minutes) reported varied operating times. Our study when compared to other study had faster operating time on an average basis. The limitation of the present study was that it was a cross sectional study and covered single tertiary care center. Multicenter randomised controlled trials comparing NVDH with other techniques will give better picture of the safety and ease of the technique. Nonetheless, it is one of the study which adds up to the research gap on NVDH procedure.
CONCLUSIONS To conclude our experience with non-descent vaginal hysterectomy, the most common diagnosis was AUB-L and common uterine size was 8 weeks. The blood loss was less among the patients who underwent this procedure. The mean blood loss differed significantly among different diagnosis. Use of hydro dissection did not influence the blood loss in the cases and is entirely dependent upon the skill of the surgeon. Intra operative complications were less with most common ones including the bladder injury and haemorrhage. Post operatively one case had fever and three had spinal headache. The mean hospital duration stay was 3 days and mean duration of surgery was around 54 minutes. Considering the indication frame, NVDH is one of the best hysterectomy techniques in terms of less complications and faster recovery.
REFERENCES
Policy for Articles with Open Access:
|
|
 Home
Home