|
Table of Content - Volume 16 Issue 2 - November 2020
A study of histopathological correlation of abnormal uterine bleeding with clinical symptoms
Neha G Jagdale1*, Prabhakar Gawandi2, Vidya Tirankar3
1MS, 2Associate Professor, 3Professor and Head, Department of obstetrics and gynaecology, Dr V.M. Government Medical college, Solapur, Maharashtra, INDIA. Email: docneha19@gmail.com
Abstract Background: Abnormal uterine bleeding is a significant clinical entity. AUB and its subgroup, heavy menstrual bleeding (HMB), are common conditions affecting 14–25% of women of reproductive age and have a significant impact on their physical, social, emotional and/or material quality of life. Aim and objective: To study the histopathological correlation of abnormal uterine bleeding with clinical symptoms Methodology: The present study was carried out at tertiary care centre from Aug 2016 to Aug 2018 in the department of OBGY. 182 cases of AUB were selected randomly from IPD and OPD. A detailed history was taken and investigations were carried out. Results And Discussion: Clinico-histopathological Correlation of two component of PALM – COEIN classification done by using Z - test for difference b/w proportion, Statistically more significant (p < 0.05) categories were AUB-A (12.08vs. 21.97 %), AUB-M (4.39 vs. 8.79 %), AUB L and A (6.59 vs nil).
INTRODUCTION Abnormal Uterine Bleeding (AUB) is defined as any bleeding that is excessive in duration, frequency or amount for that patient.1 AUB, further definitions may be subdivided based on the volume of menstruation, regularity, frequency, duration, chronicity, and timing related to reproductive status. AUB can occur at any age in various forms and has different modes of presentation. Abnormal uterine bleeding during reproductive age can result from a broad spectrum of conditions ranging from physiological process to malignant lesions involving organic, systemic, and hormonal responses. Abnormal uterine bleeding is the most common complaint encountered in perimenopausal age group causing significant physical and mental morbidity and financial burden on these patients. 2 AUB interferes with a woman’s physical, social, emotional and material quality of life.3 Abnormal uterine bleeding is responsible for more than one third of gynecologic consultations and nearly two-thirds of hysterectomies.4 AUB may be due to fibromyoma, adenomyosis, endometrial polyp, ovarian tumour, pelvic inflammatory disease (PID), endometrial hyperplasia, endometrial carcinoma, hormonal imbalance (like hypothyroidism), orhypothalamic-pituitary diseases. In a large number of patients, AUB occurs without any systemic causes or any organic lesions of the genital tract and for this, the term dysfunctional uterine bleeding was used. The key to successful clinical management is to recognize or identify the causative factors responsible. This can be achieved by thorough clinical examination, ultrasonography and histopathological examination. When no systemic and pelvic cause is evident to the clinician, histopathological examination remains the only alternative to reach the diagnosis, after ruling out the organic causes. Endometrial sampling could be effectively used as the first diagnostic step in AUB, although at times, its interpretation could be quite challenging to the practising pathologists. This study was done to evaluate the histopathology of endometrium for identifying the endometrial causes of AUB and to correlate clinical findings of AUB with histopathology report. Aim and objective: To study the histopathological correlation of abnormal uterine bleeding with clinical symptoms
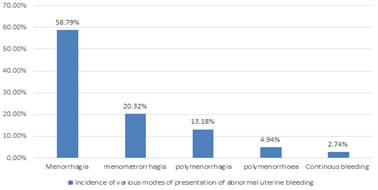
MATERIAL AND METHODS Present study was a hospital based prospective observational study conducted out in the Department of Obstetrics and Gynaecology, at tertiary health care centre. Study duration was September 2016 to August 2018. Study population was patients with Abnormal Uterine Bleeding in 15-55 years age group. Inclusion Criteria: 1. All cases from perimenarchal to perimenopausal patients of abnormal uterine bleeding (unpredictable, irregular, excessive duration, abnormal volume, and /or abnormal frequency of menses and intermenstrual bleeding) 2. Patients willing to participate and follow up Exclusion criteria: 1. An established diagnosed case of pregnancy 2. Women with obvious cervical cause for vaginal bleeding Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study them. Patients of AUB coming to the outpatient department (OPD) and admitted as a case of AUB were included in the study. The demographic details were noted and structured history regarding previous and current menstrual history, followed by general ,physical, systemic and gynaecological examination. Based on history and detailed examination findings clinical diagnosis and allocation of cases to PALM – COEIN was done. Pelvic ultrasound to assess the uterus (Uterine size, endometrial thickness, the presence of endometrial thickness, endometrial polyp, adenomyosis, fibroids) and ovarian status ( Any cysts, mass and its characteristics) Have been done.1 Endometrial material is obtained by conventional D and C. Wherever applicable hysterectomy specimens have been obtained and subjected to histopathology examinations. In all suspected cases of Uterine malignancy and endometrial hyperplasia, endometrial sample is obtained by convention D and C/ fractional curettage. As per the histopathological findings possible underlying causes have been categorized and clinical diagnosis then correlated with histologybased final diagnosis. Endometrial histology was correlated in case of AUB-O and AUB-E with the clinical assignment. Data will be analyzed and descriptive statistics were presented as frequencies, percentages and bar charts. Z test will be applied to known the significance of correlation. RESULTS The total no. of cases admissions for AUB were 182. In our clinical study, AUB was commonly seen among 41‑ 45 years of age group. 5 cases (2.74%) are in age group 21‑ 25 years, 10 (5.49 %) cases are in an age group 26‑ 30 years, 20 (10.98 %) cases are in age group 31‑ 35 years, 28 (15.38 %) cases are in the age group 36‑ 40 years, 78 (42.85%) cases are in the age group 41‑ 45 years, 32 cases (17.58 % ) are in the age group 46 – 50 years and very few cases are seen in the age group of 46‑ 55 year. Maximum no. of women 75 CASES were para 3-4 (38.46 %) while 15 cases (8.24 %) were nulliparous, other 38 women were para 1-2 and remaining 54 women were para 5 or more. Menorrhagia and menometrorrhagia were found in 107 (58.79%) and 37 (20.32%) cases respectively. The incidence of polymenorrhagia were found in 24 (13.18%) cases, polymenorrhoea in 09 (4.94 %) cases and continuous bleeding in 5 (2.74%) cases. (fig 1) The PALM and COEIN components accounted for 52.74% and 47.25 %, respectively. OVULATORY DISORDERS (AUB-O) was assigned to be the major aetiology in 68/182 (37.36 %) in overall and 68/86(79.06 %) in the FUNCTIONAL group, whereas LEIOMYOMA (AUB-L) was the proposed major contributor in the STRUCTURAL group accounting for 55/182 (30.21) of overall and 55/ 96(57.29 %). (table1) AUB-O and AUB-E classes of COEIN component only could be evaluated histologically. COEIN component, constituted 55 /182 (30.21%) cases in overall of AUB CASES, with AUB O constituted 50/182 (27.47%) cases IN OVERALL. (table2) We studied different type of hyperplasia in endometrium. Simple hyperplasia was common among the AUB patients i.e., 6.04% and complex hyperplasia without atypia was found in 3 cases 1.64% and atypical hyperplasia was seen in only 1.1 % of cases. Out of 182 cases, Menorrhagia was the most common presenting bleeding pattern in around 107 cases and out of 107, 60 cases were associated with proliferative type of endometrium on histopathology. (table 3) Correlation was done by using Z - test for difference b/w proportion. The difference was more significant statistically (p <0.05)on clinical and the histopathological diagnostic correlation (Table 12). Values did not differ significantly in cases of AUB-L. On the other hand, histopathology could diagnose more cases in comparison with clinical-based diagnosis in the categories of AUB-A (12.08vs. 21.97 %), AUB-M (4.39 vs. 8.79 %). The difference was more significant (p < 0.05) statistically in AUB – A, AUB - M and cases having both adenomyosis and leiomyoma (6.59 % vs.nil). The instance where the clinical diagnosis was described to significantly more number of cases than those confirmed by histology was in AUB-E (9.89 vs. 2.74 %), AUB – O (37.36 vs 27.47%). (table 4 ) Figure 1: Incidence of various modes of presentation of abnormal uterine bleeding
Table 1: Distribution of cases as per clinical diagnosis (PALM – COEIN) Classification
Table 2: Distribution of cases as per histopathology-based diagnosis
Table 3: Histopathological correlation of AUB cases with their clinical symptoms
Table 4: Correlation of clinical and histopathology-based diagnosis
DISCUSSION The age distribution of AUB in our study revealed that 42.85 % of cases belonged to the 5th decade (41‑50 years) as mentioned in. The reason for the increased incidence of abnormal uterine bleeding in this age group (41‑50 years) may be due to the fact that these patients are in their climacteric period. Similarly, the study conducted by Abdulla et al.., 2011 showed 33.1% cases of AUB in the 5th decade which coincides with the present study. 5 The incidence of AUB increased as the parity increased. There were 15 cases (8.24%) were nulliparous, and out of 91.16% of women, 38 (20.87%) were para1-2 and 75 (38.46%) were para 3-4 and 54 (29.67%) were para 5 or more. Similarly, Sinha p et al. conducted a prospective study found that the incidence of AUB increased as the parity increased.6 In our study, patients presented with different types of AUB; the commonest presenting feature was menorrhagia (58.79 %).Nayak et al.., 1996 found menorrhagia in 49.1% of cases similar to our study. 7 This study focuses to categorize the patient of AUB as per the PALM- COEIN classification and is similar to studies by Khrouf et al. 8; Munro et al.9 ; Madhra et al. 10 ; Bahamondes and Ali 11 ; With this, necessary investigations can be easily done and better management of specific causes can be planned. According to the study done by Gouri et al. 12 in May'16, the category which had the most patients was ovulatory dysfunction (27%), followed by leiomyoma (24.7%). In a study done by Goel P et al. 13 ; ovulatory dysfunction was found to be the most common cause of AUB (28.3%) followed by leiomyoma (22.7%). In the study done by Qureshi and Yusuf 14 in 2013, leiomyoma was a most common category (25%) followed by ovulatory dysfunction (24%). In the study for Ratnani R et al. 15 in Sep'17, leiomyoma (35%) was the most common cause of AUB, followed by malignancy and hyperplasia, adenomyosis and ovulatory dysfunction. In the present study, leiomyoma was found in 30.21% of women and the endometrial category was applied for 9.89% patients. In present study, the most common finding was AUB O (27.47%), followed by fibroid 25.82% which was similar to study done by Hale et al.. 16,17 Another important cause of AUB was AUB-M, i.e. malignancy and hyperplasia. In the present study, endometrial hyperplasia accounted for 8.79 % of cases. The average age for women with endometrial carcinoma is 61 years, but 5–30 % of cases occur in premenopausal woman.18 In our study, proliferative endometrium was detected in 32.96 % cases, secretory endometrium in 16.48% cases and hyperplastic endometrium in 8.79% cases with menorrhagic cycle. Novak et al. found metropathia type of bleeding in 9%, menorrhagia in 51.5%, polymenorrhoea and irregular bleeding in 45% of their 66 cases of hyperplastic endometrium. 19According to Takreem et al. most frequent clinical diagnosis of endometrial hyperplasia was menorrhagia. (53.3%). 20 Bhattacherjee observed irregular bleeding in 56.2%, menorrhagia in 31.2% and metropathia type of bleeding in 12.5% of cases in his series of 32 cases having proliferative endometrium. 21 It is worth noting that majority of these patients suffered from menorrhagia and the endometrial histology showed no abnormality, it was either proliferative or secretary. The significant feature is that the clinical diagnosis in 40% of these cases was leiomyoma. In conclusion, histopathological examination of endometrium obtained by curettage remains a valuable approach to a clinical diagnosis particularly cases with menorrhagia ,metrorrhagia. According to Clinicopathological correlation of different components of PALM side and AUB-O along with AUB-E categories of the COEIN discloses significantly more cases to have structural causes (PALM) of AUB on the histopathological basis in comparison with the clinical assignment of the PALM component. In AUB-A (adenomyosis) the difference in clinical and histopathological diagnosis was significant. This reason explains the difference in clinical and histopathological diagnosis of a combination of AUB-A; L (adenomyosis and leiomyoma) which was also highly significant. This finding highlighted the importance of histological examination as an approving diagnostic tool in PALM component of AUB. Our observation is conferring with study conducted by Ramchandran et al. 6, Khan S et al. 22. In PALM component, AUB-L (Leiomyoma) the difference in clinical and histopathological diagnosis was not significant. The explanation may be that most symptomatic fibroids can be easily diagnosed by history and clinical pelvic examination. AUB-P (polyp) the difference in clinical and histopathological diagnosis was not significant (p>0.05) This observation differs from study conducted by Khan S et al. 22 who found the difference to be highly significant in case of polyps. In AUB-M (malignancy and hyperplasia) the difference in clinical and histopathological diagnosis was significant (p<0.05). This is due to that theclinically menstrual history is not particular and that bimanual examination reveals an ordinary small uterus that shows no obvious difference from the normal senile one in most cases. Similar observation was made by Devi J et al.. 23 In AUB-O (ovulatory disorders) the difference in clinical and histopathological diagnosis was also significant but, there can be AUB –O diagnose more clinically by taking proper menstrual history and further evaluation done by imaging. This is due to the fact that perimenopausal women have more anovulatory cycles. Infrequent, irregular, unpredictable menstrual bleeding that varies in amount, duration and character and is not preceded by any recognisable or consistent pattern of premenstrual syndrome or accompanied by any structural abnormality is not difficult to interpret. Conversely, regular monthly periods that are heavy or prolonged are more likely related to an anatomical cause or a bleeding disorder than to anovulation.
CONCLUSION According to Clinicopathological correlation of different components of PALM side and AUB-O along with AUB-E categories of the COEIN discloses significantly more cases to have structural causes (PALM) of AUB on the histopathological basis in comparison with the clinical assignment of the PALM component.
REFERENCES
Policy for Articles with Open Access:
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home