|
Table of Content - Volume 17 Issue 1 - January 2021
Rupture uterus: A 5-year review in a Tertiary care centre in South India
Maitri R Kulkarni1*, H C Lokeshchandra2
1Assistant Professor, Department of OBG, Pushpagiri Medical college, Thiruvalla, INDIA. 2Retired Professor and HOD, Department of OBG, Mysore Medical college and Research Institute, Mysore, INDIA. Email: my3_doc@yahoo.com
Abstract Background: To study the incidence, risk factors, maternal and foetal morbidity and mortality, associated with rupture uterus, in a tertiary care centre in southern India. Methods: A 5-year retrospective analysis of all cases of rupture uterus, carried out in Cheluvamba Hospital, attached to MMC and RI, Mysore Results: Total numbers of rupture uterus cases were 32 in a span of 5 years, with an incidence of 0.7%, with a total of 45,167 deliveries. Majority of the patients were multiparous (90%), within an age group of 20-25 years (60%). In 70% of the cases, rupture was due to previous LSCS scar. In patients with no previous scar, obstructed labour and transverse lie were the main causes, attributable for 9.3% of cases, each. Bladder injuries occurred in 31% of cases. Hysterectomy was performed in 53% of the cases and repair was possible in 43% of the cases. Still births were observed in 73% of cases, with 2 maternal deaths. Conclusion: Even in modern obstetrics, rupture uterus is still an obstetric emergency, costing lives and resources. Most of the cases were due to rupture of a previous LSCS scar. Thereby minimising the primary caesarean rates would reduce the incidence of rupture uterus. Good Antenatal care, timely referral, admission and intervention would help in reducing the maternal and foetal morbidity and mortality due to rupture uterus. Key Words: rupture uterus, obstructed labour, LSCS scar
INTRODUCTION Rupture uterus is one of the catastrophic complications of pregnancy and labour, with high feto-maternal morbidity and sometimes mortality. Although rupture uterus is commonly seen in scarred uterus, either due to previous caesarean, myomectomy or repeated dilatation and curettages. The incidence of scar rupture after 1 previous caesarean is about 1% with 60-80% success rate. Rupture of unscarred uterus can also occur although a rare event. The incidence of spontaneous uterine rupture being estimated as 1 in 8000 to 1 in 15000 deliveries. The causes of uterine rupture include, uterine over distention (due to multifetal pregnancy, polyhydramnios, or fetal anomalies), external or internal fetal version iatrogenic perforation, excessive use of uterotonics, failure to recognize labour dystocia with excessive uterine contractions against a lower uterine restriction ring. Symptoms and signs of uterine rupture include fetal bradycardia, variable decelerations, evidence of hypovolemia, loss of fetal station (detected during cervical examination), and severe or constant abdominal pain. If the foetus has been expelled from the uterus and is located within the peritoneal cavity, morbidity and mortality increases significantly. Diagnosis of uterine rupture is confirmed by laparotomy. Treatment of uterine rupture is immediate laparotomy with caesarean delivery and repair, if necessary, hysterectomy. Aims and Objectives To study the incidence, risk factors, maternal and foetal morbidity and mortality, associated with rupture uterus, in MMCandRI referral area.
MATERIALS AND METHODS A retrospective analysis of all cases of rupture uterus was done, over a span of 5 years at Cheluvamba Hospital, attached to MMC and RI, Mysore. An analysis of risk factors, maternal and fetal morbidity, mortality, and incidence of rupture uterus was done. All confirmed cases of rupture uterus at laparotomy were included in the study, whereas those with asymptomatic scar dehiscence were excluded. After obtaining the ethical clearance, the charts of these patients were analysed and the data regarding demographic characteristics, clinical presentation, risk factors, management, operative findings, maternal and fetal outcomes, and postoperative complications was studied. Statistical analysis with SPSS software using descriptive statistics, chi square tests, frequencies and percentages was performed.
RESULTS During the study period there were, 32 cases of rupture uterus with 45,167 deliveries with an overall incidence of 1 in 1411 deliveries accounting to 0.7%. There were 27 multigravidas (90%), whereas only 3 were primigravidae (10%). Most of the women were young belonging to the age group of 21-25 years (60%). Most of the women were either referred in labor from another hospital or unbooked altogether.
Table 1
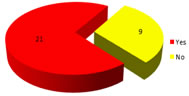
Among the 32 cases, 21(70%) occurred in scarred uteri whereas 9 occurred in unscarred uteri (30%).
Figure 1:
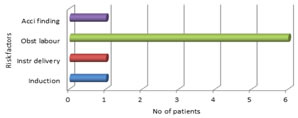
Obstructed labour was responsible for the greatest number of cases in unscarred uteri accounting upto 9.3% cases, followed by instrumental deliveries and induction of labour.
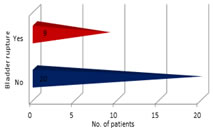
Figure 2: Intra operatively bladder rupture was found in about 31% of the cases. 1 case had a complete colporhexis.
Figure 3: The management included, a repair of uterus and repair with ligation of fallopian tubes, where possible. In most of the cases where uterus was not salvageable, a hysterectomy was resorted to. The choice of surgical procedure was based upon the type, location, and extent of tear; patient's hemodynamic status
Table 2:
Almost 25% of the women suffered severe post-operative morbidity, which included sepsis, pulmonary embolism, wound dehiscence, bladder atonia. There were also 2 maternal deaths
Figure 4: The fetal and neonatal morbidity and mortality was considerably high. There were 86.6% stillbirths versus 13.4% live births.
DISCUSSION Rupture uterus is an obstetric emergency of very serious nature leading to devastating complications, which can cost the lives of the mothers and unborn babies. Despite advancement in the field of medicine it still continues to be one of the dire emergencies daunting obstetricians1, albeit the reduction in the incidence of the occurrence as compared to previous decades2,3. With the increase in the rate of primary caesarean sections, the dynamics of the causation has shifted to scar rupture as the leading cause.4 It has been estimated that the rates of rupture are around 0.7% with a single low transverse 2.0% with low vertical scar, 0.5% with unknown scars, whereas it is significantly high as much as 4-9% with previous T shaped or classical incision5. Our study being limited by retrospective nature we were unable to assess the type or number of uterine scars. We found that most women were multiparous 90%, which is in agreement with other studies6. While obstructed labour continues to be the leading cause, followed by induction of labour and instrumental deliveries, in rupture of the unscarred uteri in our study, the major risk factors reported in other studies are grand multiparity, obstetrical trauma, fetal macrosomia, and mal-presentations7,8,9. The clinical presentation of the patients with rupture of the unscarred uterus was more dramatic with extensive tears, hypotension, and shock. Rupture of scarred uterus, on the other hand, was usually incomplete and transverse. Signs of shock were rarely a presenting feature in this group10. The consequences if unattended are life threatening, and the results depend on the timely referral and prompt management. Although many studies have not reported maternal deaths, some of the studies have reported up to 13% deaths1,6,11,12, there were 2 maternal deaths (6.25%) in our study given that most were referred cases. Fetal outcome also depends on the urgency of delivery. Rupture uterus qualifies for category 1 of caesarean, which means the delivery needs to happen within 30 minutes from the decision. The choice of surgery depends on various factors like type, location and extent of the tear. While many authors recommend subtotal or total hysterectomy as the choice of surgery, a few others advocate repair as a safer and more conservative approach12,13,14, in our study most of the women had to undergo hysterectomy.
CONCLUSION Increase in the scar rupture due to increasing rates of caesarean section. Therefore, all patients with previous caesarean scars should be made aware of the importance of proper antenatal visits in subsequent pregnancies, they also require careful prenatal supervision, proper selection of cases for vaginal delivery, early hospital admission and close supervision in labour. Good antenatal care at peripheral level, timely referral, admission and intervention, help in reducing maternal and fetal morbidity and mortality. Most cases are preventable with good antenatal and intrapartum care, and proper identification of high-risk cases.
REFERENCE
Policy for Articles with Open Access:
|
|
 Home
Home