|
Table of Content - Volume 17 Issue 1 - January 2021
Study of hypertension disorders in pregnancy and outcome of neonates in Telangana population
Associate Professor, Department of Obstetrics and Gynaecology, Mediciti Institute of Medical Sciences Ghanpur Medchal-501401 Telangana, INDIA. Email: drvijaylakshmi05@gmail.com
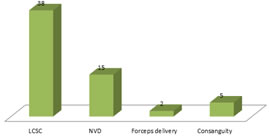
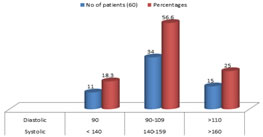
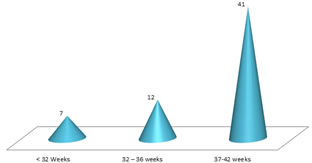
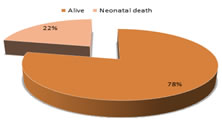
Abstract Background: Hypertensive disorders in pregnancy is a multi factorial disorder that, seriously endogenous the safety of the foetus during pregnancy and maternal morbidity and mortality. Method: Also 60 pregnant women selected for studies Blood examination CBC Blood culture, serum electrolyte CT, BT, was done. Foetal monitoring includes DFMC. FHR, NST umbilical and cerebral Doppler, USG to assess the foetal serial growth, AFI, BPP, placental location and maturity. Results: Types of delivery were 38 (63.3%) LCSC, 15 (25%) NVD 2 (3.3%) forceps delivery, 5 (8.3%) consanguity, 11 (18.3%) patients had < 140 systolic, 90 diastolic BP, 34 (56.6%) had 140-159 systolic 90-109 diastolic BP, 15 (25%) had > 160 systolic and > 110 diastolic BP. In the gestational age study 7 (11.6%) patients had 32 weeks, 12 (20%) had 32-36 weeks, 41 (68.3%) had 37-42 weeks of gestation, 27 (45%) were LBW, 10 (16.6%) were very low birth weight, 19 (31.6%) had normal birth weight, 18 (30%) were IUGR. The foetal outcome study had 47 (78.3%) were alive, 13 (21.6%) had neonatal death. Conclusion: Early detection and management death of pre clampsia, proper antenatal care, timely referral of high risk patient to higher centres where all facilities and specialities are available. Administration of MgSo4 in correct doses and proper timed caesarean will certainly reduce the incidence of eclampsia associated with incidences of maternal and perinatal morbidity and mortality. Keywords: HTN, NgSo4 IUGR, LBW, Gestational age, eclampsia.
INTRODUCTION Hypertension (HTN) disorder of pregnancy is the major cause of poor pregnancy outcome that encountered during pregnancy1. HTN in pregnancy defined as abnormal raising of blood pressure which diagnosis as chronic HTN, gestational HTN, mild pre-eclampsia, severe preeclampsia or/and eclampsia2. In India and abroad 10-15% of pregnant women affected with HTN which cause substantial maternal and infant morbidly and mortality3. About 70% maternal deaths were attributed to five major complications Haemorrhage, infections unsafe abortion, Hypertensive disorders in pregnancy and obstructed labour. HTN in pregnancy increases serious risk of maternal and new born baby such as premature delivery, IUGR prenatal mortality and morbidity, acute renal failure, acute hepatic failure, bleeding at the time of delivery and post partum bleeding. Maternal mortality and morbidity following harm, such as disseminated intravascular coagulation (DIC) and seizures4. Hence the magnitude of HTN in pregnancy is evaluated in detail.
MATERIAL AND METHOD Sixty (60) pregnant women regularly visiting obstetrics and Gynaecology department of Mediciti Institute of Medical Science HG Ghanpur Medchal-501401 Telangana were studied. Inclusive Criteria: Pregnant women having history of HTN, gestation HTN, preeclampsia, eclampsia, essential HTN were selected for study. Exclusion Criteria: Pregnant women have diabetes mellitus, gestation diabetes, Thyroid disorders; history of epilepsy was excluded from study. Method: Antenatal check up (ANC) gestational age determined by last menstrual period (or first trimester, USG) was recorded. HTN disorders, obstetric problems like preterm labour was recorded. In addition to this Neonatal parameters like gestational age, birth, weight, respiratory distress syndrome, congenital pneumonia, and convulsion were also recorded. Blood examination included – CBC (complete Blood count) blood culture serum electrolytic coagulation and bleeding time (CT, BT) was also noted. Foetal monitoring included – DFMC, FHR, NST, umbilical Doppler, USG was done to assess foetal serial growth, AFI, BPP placental location and maturity. Treatment included rest, control of blood pressure by using antihypertensive drugs Nefidepine, Methyldopa, Labetalol depending upon the severity of BP (Blood pressure) for control of seizure anticonvulsants, MgSo4, IV was given slowly over 5-10 minutes and 5 gm of 50% MgSo4 I M 4 hourly (in alternate gluteus region). In mild preeclampsia and gestational HTN termination of pregnancy was done by inducing labour at 37 weeks at this gestational age. In patients <37 weeks of gestation termination of pregnancy was warranted only if maternal condition detoraited or if there was foetal compromise. Pregnancy was terminated by LSCS for urgent termination a for maternal shake as in the acute fulminating preeclampsia and eclampsia when cervixes are not ripe and also for foetal sake when foetal was in jeopardy as indicated by de-arranged Doppler studies (reveres diastolic flow), severe IUGR, meconicum staining of liquor or foetal distress. The duration of study was three years (July-2017 to August-2020). Statistical analysis: Types of delivery, various HTN disorders, gestational ages, different body weight of Neonates, outcomes at birth, were classified with respective percentage. The statistical analysis was done in SPSS software. This research paper was approved by ethical committee Mediciti Institute of Medical Sciences Ghanpur – medchal – 501401. Telangana.
OBSERVATION AND RESULTS Table – 1: Study of types of delivery in HTN pregnancy – 38 (63.3%) LCSC, 15 (25%) by NVD, 2 (3.33%) forceps delivery, 05 (8.33%) consanguity. Table – 2: Study of parameters of HTN in pregnancy – 11 (18.3%) patients had <140 systolic and 90 mm Hg diastole, 34 (56.6%) patients had 140-159 mm/Hg systolic and 90-109 mm/Hg diastole, 15 (25%) had > 160 mm/Hg systole, > 110 diastole Table – 3: Study of gestational age in HTN pregnancy – 7 (11.6%) had > 32 weeks gestation, 12 (20%) had 32-36 weeks, 41 (68.3%) had 37-42 weeks. Table – 4: Study birth weight of Neonates in HTN pregnancies – 27 (45%) were LBW 10 (16.6%) very low birth weight, 19 (31.6%) had normal birth weight, 18 (30%) had IUGR. Table – 5: Outcomes of Neonates in HTN pregnancies – 47 (78.3%) alive, 13 (21.6%0 neonatal death.
Table 1: Types of delivery in HTN pregnant Women
(LCSC = Lower Uterine Caesarean Section) (NVD = Normal Vaginal Delivery)
Table 1: Types of delivery in HTN pregnant Women
Table 2: Study of HTN in pregnant Mother
Table 2: Study of HTN in pregnant Mother
Table 3: Study of gestational in HTN pregnancy
Table 3: Study of gestational in HTN pregnancy
Table 4: Study of Body weight of Neonates in HTN pregnancy
Table 4: Study of Body weight of Neonates in HTN pregnancy
Table 5: Study of foetal outcome in HTN in pregnancy
Table 5: Study of foetal outcome in HTN in pregnancy
DISCUSSION In the present study of HTN disorders in pregnancy and outcome of emanates in Telanganan Population. The types of deliveries were 38 (63.3%) LCSC, 15 (25%) NVD, 2 (3.33%) forceps delivery, 5 (8.33%) consanguity (Table-1). In the profile of HTN 11 (38%) had < 140 systolic, 90 mmHg diastolic BP, 34 (56.6%) had 140-159 systolic, 90-109 Diastolic BP, 15 (25%) had > 160 Systolic and > 110 diastolic BP (Table-2). The gestational age study shown 7 (11.6%) had <32 weeks, 12 (20%) had 32-36 weeks, 41 (68.3%) had 37-42 weeks of gestation (Table-3). 27 (45%) were LBW, 10 (16.6%) were very LBW, 19 (31.6) had normal birth weight, 18 (30%) had IUGR (Table-4). 47 (78.3%) were alive and 13 (21.6%) were neonatal death (Table-5). These findings were more or less in agreement with previous studies5,6,7. As majority of people are illiterate belonged to middle socio-economic status hence they come to hospital only when there is any serious problems hence eclampsia is often missed. More over pre eclampsia is asymptomatic and remits spontaneously. In addition to this, there are many predisposing factors related to preeclampsia, such as maternal age, familial aggregation, and race, smoking, socio-economic level, diet, and family history9. Apart from this It is established fact that, majority of Indian women are suffering with obsessive compulsive disorder (OCD). This internal agitation, non-compromising attitude elevates the hypertension even during pregnancy. It was also reported that, causes of maternal deaths were due to intra cerebral haemorrhage, aspiration pneumonia, and intractable congestive cardiac failure10. Multiple pregnancy and multiparty also significantly associated with HTN in pregnancy which included renal and cardiovascular diseases (11). Hence antenatal care is must to avoid preeclampsia and further complication
SUMMARY AND CONCLUSION The present of HTN disorders in pregnancy and its outcomes of neonates in Telangana population is quite useful to obstetric and gynaecologist, cardiologist to treat such patients efficiently because magnitude and pathogesis of eclampsia is still unclear.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home