|
Table of Content - Volume 17 Issue 2 - February 2021
Study of post-partum haemorrhage in Telangana population
Vijaylakshmi Chirumamilla
Associate Professor, Department of Obstetrics and Gynaecology, Mediciti Institute of Medical Sciences Ghanpur Medchal-501401 Telangana, INDIA. Email: drvijaylakshmi05@gmail.com
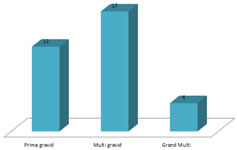
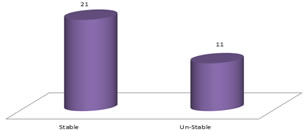
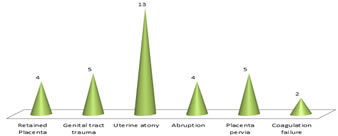
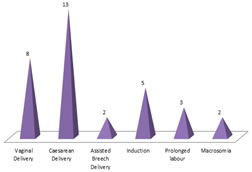
Abstract Background: Post partum haemorrhage (PPH) is the major cause of maternal morbidity and mortality in middle socio-economic status women. Method: Apart from Biochemical and haematological study. I.V. fluid infusion use of oxytocin, prostaglandins Blood transfusion, manual removal of placenta, other appropriate surgical intervention were tried and noted. Results: The parity study was – 12 (36.3%) were prima gravida, 17 (51.5%) multigravida, 4 (12.1%) were grand multi. The hemodynamic status was 21 (63.6%) were stable, 11 (33.3%) were unstable. The clinical manifestations was 4 (12.1) had retained placenta, 5 (15.1%) had trauma in genital tract, 13 (39.3%) had uterine atony, 4 (12.1) had abruption, 5 (15.1) had placenta pervia, 2 (6%) had failure of coagulation. The types of labours were 8 (24.2%) had vaginal delivery, 13 (39.2) had caesarean delivery, 2 (6%) had assisted Breach delivery, 5 (15.1) had induction, 3 (9%) had prolonged labour of morbidity were 9 (27.2%) had NICU admission, 12 (36.3%) had prematurity, 5 (15.1%) had jaundice, 4 (12.1%) had septicaemia, 3 (9%) were quite normal (No morbidity). Conclusion: As PPH is life threatening which causes maternal morbidity and mortality. Hence prevention at the earliest with proper approach will save the life of mother. Availability of blood and blood product plays key role in PPH. Keywords: PPH, Placenta pervia, haemodynamicity, uterine atony, morbidity.
INTRODUCTION Obstetric haemorrhage is often severe and is the most feared obstetric emergency that can occur to any women at child birth. If unattended, the haemorrhage can cause fatal to healthy women1. The maternal mortality due to post-partum haemorrhage is estimated 127,000 deaths every year globally2,3. As PPH occurs within 24 hours and 6 weeks post-partum, most likely due to infection secondary to retained placental products4. Multiple pregnancies, macrosomia, induction of labour, operative vaginal deliveries and caesarean section. Hence WHO define PPH if the blood loss is 500 ml in the first 24 hours of post partum5. Hence attempt was made to evaluate the risk factors, types of PPH in the present study.
MATERIAL AND METHOD 33 (thirty-three) full term pregnant women regularly visiting to obstetric and Gynaecology department. Mediciti Institute of Medical Sciences hospital Ghanpur Medchal-501401. Telangana were studied. Inclusive Criteria: Patients having primary and secondary PPH and who had loss of Blood >1500 ml and haemo-dynamically unstable were also included in the study. Exclusion Criteria: Cardiac patients, patients having H/O epilepsy, on antidepressant treatment and HIV positive patients were excluded from the study. Method: Detail history of each patients, age, social-economic status was noted. The obstetric history included, time of onset of pain and duration of pain history of vaginal leak or bleeding, medicines use like IV fluids, Oxytocin ergometrine, prostaglandins, per vaginal examination, ARM, episitomy given any instrumental use, manual removal of placenta and blood transfusion if any noted. The duration study was about 2 years (July 1918 to August 2020). Statistical analysis: Various parameters like parity, conditions causing haemorrhage, pregnancy related variables, types of labour, perimorbidal conditions were classified with percentage. The statistical analysis was carried out in SPSS software. This research paper was approved by Ethical committee of Mediciti Institute of Medical Science Ghanpur Madchal-501401 (Telangana).
OBSERVATION AND RESULTS Table-1: Study of parity in patients of PPH 12 (36.3%) were prima gravid, 17 (51.5%) multigravida, 4 (12.1%) were Grand multi. Table-2: Hemodynamic status was – 21 (63.6%) were stable, 11 (33.3%) were unstable. Table-3: Clinical manifestations of PPH, 4 (12.1%) had retained placenta, 5 (15.1%) had genital tract trauma, 13 (39.3%) had uterine atony, 4 (12.1%) had Abruption, 5 (15.1%) placenta pervia, 2 (6%) failure of coagulation. Table-4: Types of labours in PPH patients 8 (24.2$) had vaginal delivery, 13 (39.2%) had caesarean Delivery, 2 (6%) had assisted Breech delivery, 5 (15.1%) had induction, 3 (9%) had prolonged labour, 2 (6%) had macrosomia. Table-5: Causes if prenatal morbidity in PPH patients – 9 (27.2%) had NICU admission, 12 (36.3%) had prematurity, 5 (15.1%) had jaundice, 4 (12.1%) had septicaemia, 3 (9%) were quite normal (hence no morbidity).
Table 1: No. of patients: 33 Study of Parity in patients if PPH
Table 1: Study of Parity in patients if PPH Table 2: No. of patients: 33 Hemodynamic status of PPH Patients
Table 2: Hemodynamic status of PPH Patients
Table 3: Clinical Manifestations of PPH (Post-Partum Haemorrhage (No. of Patients: 33)
Table 3: Clinical Manifestations of PPH (Post-Partum Haemorrhage
Table 4: No. of patients: 33 Types of Labours in PPH patients
Table 4: Types of Labours in PPH patients
Table 5: No. of patients: 33 Causes of prenatal Morbidity in PPH patients
Table 5: Causes of prenatal Morbidity in PPH patients
DISCUSSION In the present of PPH in Telangana Population – 12 (36.3%) were prima gravida, 17 (15.5%) were multigravida, 4 (12.1%) were grand multi (Table-1). Hemodynamic status was 32 (63.6%) were stables, 11 (33.3%) were unstable (Table-2). In the clinical manifestations – 4(12%) had retained placenta, 5 (15.1%) had trauma on genital tract, 13 (39.3%) had uterine atony, 4 (12.1%) had abruption, 5 (15.1%) had placenta pervia, 2 (6%) had failure of co-ogulation (Table-3). The types of labours were – 8 (24.2%) had vaginal delivery, 13 (39.2%) had caesarean delivery, 2 (6%) had assisted breech delivery, 5 (15.1%) had induction, 3 (9%) had prolonged labour, 2 (6%) had macrosomia (Table-4). The causes of prenatal morbidity were 9 (27.2%) had NICU admission, 12 (36.3%) had prematurity, 5 (15%) had jaundice, 4 (12.1%) had septicaemia, 3 (9%) were normal (Table-5). These findings were more or less in agreement with previous studies6,7,8. PPH is the one of the third stage complications which every obstetrician faces and is very challenging most of the times. Despite of improvement in management, early PPH still remain a significant cause of maternal morbidity and mortality in developing countries9. It is reported that, longer-acting oxytocin derivative, carbetocin (single dose) specifically indicated for prevention of PPH in context of caesarean delivery is at least as effective as oxytocin by infusion10. Moreover poverty middle socio-economic status affects the maternal health during pregnancy which may lead to PPH11 may end in maternal morbidity and mortality. There may be one of the cause which is related to PPH is Tone, Tissue, trauma, Thrombin (four Ts). The most common is PPH uterine atony. Clinical examination to find out the above mentioned cause, if the pharmacological (drugs) treatment fails to control bleeding in case of atonic PPH and mechanical method of control by balloon catheter temponade is instituted before considering the surgical procedure12. In majority of cases Hysterectomy was avoided in PPH by arterial embolism. There are multiple surgical options available including uterine compression sutures, vascular ligations and peri partum Hysterectomy.
SUMMARY AND CONCLUSION Globally PPH is the leading cause of maternal mortality and morbidity. Prevention plays very important role by identifying high risk factors and active management of labour management requires multidisciplinary approach is essential in severe haemorrhage. Prediction and assessment of blood loss remains the corner stone for prompt and effective management of PPH. But still it requires genetic, nutritional and angiological study because exact pathogenesis of PPH is still unclear.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home