|
Table of Content - Volume 17 Issue 2 - February 2021
The effect of mifepristone in induction of labour at term
Priyanka1, Shukla S Shetty2*
1Assistant Professor, Department of Obstetrics and Gynaecology, Gulbarga Institute of Medical Sciences, Kalaburgi, INDIA. 2Professor & HOD, Department of Obstetrics and Gynaecology, JJM Medical Collage, Davangere. INDIA. Abstract Background: One of the most common indication for labor induction is prolonged pregnancy, which is associated with many of the fetal complications. Present study evaluated effect of Mifepristone. Aim and objective: To study the effect of Mifepristone in induction of labour at term Methodology: This was a prospective study involving 110 women with gestational age 41 weeks. Tab Mifepristone 200mg single dose was given to study subjects after written informed consent after assessing the bishop score at admission. Bishop's score was reassessed at the end of 24 hours, if the score was <6, other methods of induction was given. If the bishop score was >6 ARM was done. Effect of Mifepristone was assessed by BISHOP score and IDI (Induction Delivery Interval). Results: There was significant change in mean bishop score from 3.25 to 8.35 . Induction delivery interval was 47.7 hours. In our study 73.6% women delivered without the need of any other methods of induction other than Mifepristone. Key Word: mifepristone.
INTRODUCTION The ability to induce labour has been of interest to many societies from the primitive to the ancient to the modern. For the majority of women, labour starts spontaneously and results in vaginal delivery at or near term.1 Cervix plays essentially a passive role as an innocent obstruction and is acted upon by all the forces of labour. A ripe or favorable cervix is a prerequisite for successful vaginal birth.2 The cervical dilatation during labour is strongly influenced by the cervical ripening which is done prior to induction of labour. Bishop score is the most prevalent scoring system for preinduction cervical assessment. This system and its many modifications take into account the cervical dilatation, effacement, consistency and position and the station of the presenting part. Cervical dilatation is the factor with the strongest association with successful induction.3 One of the most common indications for labour induction is prolonged pregnancy as it is associated with increased risk to the fetus including Fetal distress, Low APGAR score at 5-minute, Meconium aspiration syndrome, Non-reassuring fetal heart rate, Increased risk of death within the first year of life, Placental dysfunction and Oligohydramnios. Recently, the most fascinating synthetic mifepristone (RU-486) has been the focus of attention in the arena of various labour inducing agents. Mifepristone is a steroidal compound that has antiglucocorticoid and antiprogesterone properties. It increases uterine activity and causes cervical effacement and dilatation for pregnancy termination. Mifepristone has an established role in termination of pregnancy during the early first, and the second trimester.4 The first trial, performed in Geneva in 1982, 5 indicated the actual antiprogesterone activity of RU486 in human beings, and it was followed by many clinical studies mostly in the gynecologic and obstetrical fields. Animal studies have suggested that mifepristone also has a role in inducing labour in late pregnancy. There is insufficient information available from the clinical trials to support the use of mifepristone to induce labour. Keeping this in mind, the present study is undertaken to find out the safety and efficacy of mifepristone for preinduction cervical ripening and labour induction in women with prolonged pregnancy Aim and objective: To study the effect of Mifepristone in induction of labour at term
MATERIAL AND METHODS Present study was a Prospective study carried out in Chigateri General Hospital, Bapuji Hospital and Women and Children Hospital, Davangere during the period of November 2016 –October 2018. Study population was 110 cases with gestational age sbetween 41-42 weeks including cases with previous LSCS willing for normal vaginal delivery. Inclusion Criteria:
Exclusion Criteria:
Indications For Induction In Our Study was Post dated pregnancy. Sample size is calculated using the formula : n= {Z1-α/2}2× S2 _________ d2 Z1-α/2 = 1.96 S = Standard deviation of Bishop's score based on previous literature70 d = 7% of mean Bishop's score = 7.1 (2.02) = 0.1414 Sample size = (1.96)2× (0.749)2/ ( 0.1414)2 = 108 Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pre tested questionnaire. Data included demographic data like age and sex, detailed clinical history and through clinical examination. Per abdominal examination was done. Gentle pelvic examination was done to assess the status of cervix by modified bishops score. All patients underwent complete blood count, urine examination, Ultrasonography. Tab mifepristone 200mg single dose was given after examination was complete. Bishop score was assessed on admission. Repeat bishop score was assessed at the end of 24 hours. If it was <6, labour was induced using other inducing agents like tablet misoprostol 25micrograms 4th hourly, cerviprime gel instillation till the bishop score became >6 or the women entered active labour, no other method of induction was used. If the bishop score was >6 at the end of 24 hours, ARM was done and if required oxytocin was started for augmentation of labour. After induction patients were monitored for signs of labour, when labour ensued, they were closely monitored for maternal vital signs, progress of labour, and fetal heart rate which was monitored by intermittent auscultation. If fetal heart rate remained normal with satisfactory progress of labour, those women were kept for vaginal delivery. If the progress was unsatisfactory or variable fetal heart rate pattern, those women were taken for caesarean section. The effectiveness of Mifepristone was assessed on the basis of improvement in bishop score, and duration of induction to active phase of labour. Successful induction was considered when women entered into active labour within 24 to 48 hours after administration of mifepristone. Failed induction was considered when women failed to enter into active labour at the end of 48 hours of administration of tab Mifepristone. Data was entered in excel sheet and analysed with SPSS version 22.
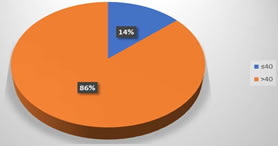
RESULTS Total 110 patients were included in our study. In our study 65 women (59.1%) were primigravidae, 28 women (25.5%) multigravidae, and 17 women (15.5%) were with previous 1 LSCS. (table 1) Out of total 110, 95 (86.4%)women involved in the study were with gestational age 41 weeks and beyond and 15 women (13.6%) of women were with gestational age less than 40 weeks. (fig 1) In our study, pre induction BISHOP score was 3.24±0.9. Post induction (the end of 24 hours after the administration of tab Mifepristone) score was 8.36± 1.8. Statistically significant change in the bishop’s score was observed at the end of 24 hours. (p<0.001) After 24 hours of administration of tab Mifepristone, if the bishop score remains <6, patients were induced with other methods of induction. The above table shows 11 patients among 110 were induced with 1 dose of cerviprime gel, 10 patients were induced with tab misoprostol 25 micrograms and 70 (63.64%) patients required no other methods of induction where in the bishop score at the end of 24-36 hours was >8. Out of 110 patients induced, 99 delivered vaginally, 11 patients underwent caesarean section. Table 4 shows mean induction delivery interval in primigravidae was 47.77 hours and in multigravidae was 37.56 hours. IDI in muligravidae patients was significantly lower than primigravidae patients (P<0.001).
Table 1: Distribution of patients according to parity
Figure 1: Distribution of patients according to gestational age
Table 2: Pre and post induction of BISHOP score
Table 3: Distribution of patients according to mode of delivery
Table 4: Induction Delivery Interval according to parity
DISCUSSION In our study we intended to assess the efficacy of tab Mifepristone for preinduction cervical ripening and induction of labour at term. This study was restricted to the patients who were admitted to the Chigateri hospital, Women and Children hospital, and Bapuji hospital, Davangere , who fulfilled inclusion and exclusion criteria. Ours is a prospective study involving 110 patients. In the present study 90% patients were delivered vaginally, 10% underwent emergency LSCS. There was significant change in the Bishop score at the end of 24 hours after the mifepristone administration.63.64% patients delivered vaginally without any other method of induction followed by mifepristone. 10% patients were induced with single dose of cerviprime gel at the end of 24 hours where the Bishop's score was <6. The average induction delivery interval was 47.57 hours in primigravidae. Similar results were reported by Wing et al.. 6 More spontaneous vaginal deliveries and less incidence of LSCS and less instrumental deliveries were noted by Fathima et al..7 Byrne and Wing 6 demonstrated that Mifepristone exposure and induced labour were associated with increase in cortisol levels, which was observed within 18 hours. Li L, Gao W, 8 Chen S did a study at Beijing Tian Tan Hospital, Capital University of Medicine on Labour induction in women at term with mifepristone and misoprostol. Results of their study, women who were given mifepristone: the cervical length was 1-3 cm shorter and Bishop score was 4-5 higher than those before treatment. In our study statistically significant improvement was observed in mean Bishop’s score at the end of 24 hours. This improvement in score indirectly indicates withdrawl of progesterone. Wing et al.. 9 demonstrated favorable Bishop score after 24 hours of mifepristone. Atwale et al.. 10 and Fathima et al..7 also noted the significant change in Bishop score with the use of oral Mifepristone. Our results were consistent with the literature that showed decreased prostaglandin requirements for term induction. Hapangama and Neilson 11 reported that mifepristone -treated women were less likely to undergo caesarean section as a result of failure to induce labour (RR 1.43, 95 % CI 0.20–0, 80) and they were less likely to need the augmentation with oxytocin (RR 0.80, 95 % CI 0.66–0.97) . The rate of successful induction in our study was comparable with Wing et al.. 9 Yelikar Kanan et al. 12 conducted a study on 100 subjects with late term pregnancy beyond 40 weeks and bishop score <6. Concluded that MIFEPRISTONE is an effective inducing agent for cervical ripening and initiation of labour when given 24 hours prior to induction in late term pregnancy. In a previous scarred uterus when other drugs can not be used to induce labour, Mifepristone is a wonder drug for induction of labour in a case of previous LSCS willing for trial of labour. However more studies are required on larger population to prove it to be an ideal agent for cervical ripening. Therefore, this may justify future trials comparing mifepristone with the routine cervical ripening agents currently in use.
CONCLUSION Mifepristone is an effective inducting agent for cervical ripening which can be used in prolonged pregnancy.
REFERENCES
Kanan Y, Deshapande S, Deshapande R, Lone D. Safety and Efficacy of Oral Mifepristone in Pre-induction Cervical Ripening and Induction of Labor in Prolonged Pregnancy.The Journal of Obstetrics and Gynecology of India. July-August 2015;65(4):221-5.
Policy for Articles with Open Access
|
|
 Home
Home