|
Table of Content - Volume 18 Issue 1 - April 2021
Study of correlation of umbilical cord abnormalities with neonatal outcome
Alka B Patil1, Sayli Thavare2*, Bhagyashree Badade3
1Professor & HOD, 3Junior Resident, Department of Obstetrics and Gynecology, ACPM Medical College, Dhule, Maharashtra, INDIA. Email: saylithavare0693@gmail.com
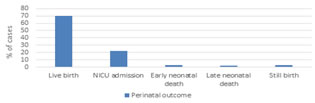
Abstract Background: Umbilical cord abnormalities usually describe situations where fetal blood flow is reduced or interrupted due to altered structure or function of umbilical cord. Defects or disease of cord may seriously affect the health and even life of the fetus. Aims and Objectives: The aim of this study is to assess the impact of umbilical cord abnormalities on neonatal outcome. Method: This retrospective study was conducted in ACPMMC Dhule. 100 pregnant women with singleton pregnancy who delivered after 28 weeks of gestation and who were diagnosed and documented as having umbilical cord abnormalities either antenatally or during and after delivery were included. Neonatal outcome was assessed based on APGAR score, NICU admissions, still birth. Results: 64% of the total study patients delivered Vaginally whereas 36% underwent caesarean section either elective or emergency. 70% fetus had live birth without any complication and did not require NICU admission. 22% required NICU admission. 3% had early neonatal death, 2% late neonatal death whereas 3% was still birth. Conclusion: Umbilical cord abnormalities is a stress factor for fetus, where stillbirth can occur due to combination of risk factors. This is especially important because most of these still births occur relatively late in pregnancy in a setting of otherwise normal foetuses and pregnancies. Therefore early detection and continued surveillance will help to prevent such sudden fetal loss. Keywords: Umbilical cord abnormalities, Nuchal cord, Cord knots, Cord prolapse, Still birth.
INTRODUCTION The umbilical cord is a conduit between developing embryo or fetus and placenta.1 Baden in 1955 wrote: “intrauterine life , which is sustained only by two small arteries and a tortuous vein coursing through a long flexible cord, hangs by a very delicate thread.”2 Umbilical cord abnormalities usually describe situations where fetal blood flow is reduced or interrupted due to altered structure or function of umbilical cord. Defects or disease of cord, if of enough degree may seriously affect the health and even life of the fetus. Umbilical cord abnormalities may be acute or chronic and they may be intermittent or persistent. Abnormal cord parameters are associated with:
A considerable number of stillbirths which are thought to be unexplained may be because of cord abnormalities. Of the possible Umbilical cord abnormalities, nuchal cord has been studied the most and its incidence increases throughout gestation, peaking at birth.3,4 While there are some reports of nuchal cord in individual cases of still birth, others report no effect of nuchal cord on still birth. Umbilical cord abnormalities including true knots and cord prolapse are rarer but are also linked to adverse outcomes like perinatal death and low APGAR scores. Umbilical cord abnormalities can present in combination. For example true knots may occur in long cords which are also more prone to entanglement thereby complicating the appreciation of significance of individual abnormalities.5,6 In spite of improvement in antenatal care and use of modern monitoring techniques such as ultrasonography, Doppler and intrapartum fetal monitoring, cord complications remain one of the major unavoidable cause of fetal death compromising umbilical blood flow to a degree sufficient enough to prejudice their life. The aim of this study is to assess the impact of umbilical cord abnormalities on neonatal outcomes.
MATERIAL AND METHODS A retrospective study was conducted in Department of Obstetrics and Gynecology, ACPM Medical college, Dhule from AUGUST 2018 to August 2019. 100 pregnant women with singleton pregnancy who delivered after 28 weeks of gestation during 1 year period from August 2018 to August 2019, who were diagnosed and documented as having umbilical cord abnormalities either antenatally or during and after delivery were included in the study after taking informed and written consent. Mode of delivery noted: Vaginal or Caesarean. Recorded post-delivery neonatal outcome on basis of: APGAR score at 1 and 5 minutes. NICU admission. Perinatal mortality Inclusion Criteria: Maternal age between 18-35 years. Primigravida or multigravida. Singleton pregnancy. Pregnancy of 28 weeks onwards. Antenatal diagnosis of umbilical cord abnormalities by USG and/or Doppler. Women delivered by vaginal route or c section with gross umbilical cord abnormalities. Exclusion Criteria: Pregnancy complicated by obstetrical, medical and surgical disorders. Fetal congenital anomalies detected at prenatal ultrasonography. Oligohydramnios/ polyhydramnios. Multiple gestation. Rh incompatibility/ fetal hydrops. Diagnosed intrauterine fetal death at time of first ultrasonographic examination.
RESULTS As expected, age of majority of patients was in the range of 21-28 years as this group is most fertile. Primigravida comprised of 38% whereas 62% were multigravida.
Table 1: UMBILICAL CORD ABNORMALITIES:
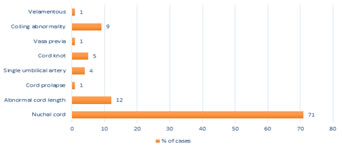
Graph 1: TYPE OF ABNORMALITIES AND PERCENTAGE OF CASES
Of all the abnormalities of umbilical cord, the most common abnormality encountered is Nuchal cord (cord around the neck) with 71 % cases in our study. Abnormal cord length i.e. Long (>100cm) and short (<40cm) was seen in 12% cases. Rare abnormalities like vasa previa, velamentous insertion and cord prolapse was seen in 1% cases each. Single umbilical artery was seen in 4% cases. Cord knot which includes true as well as false knots was seen in 5% cases of which only 1 case had true knot. Coiling abnormality which includes hyper as well as hypo coiled cord was seen in 9% cases.
Graph 2: MODE OF DELIVERY 64% patients had normal vaginal delivery whereas 36% patients required Caesarean section
Table 2: NEONATAL OUTCOME
Table 3: PERINATAL OUTCOME
Graph 3: PERINATAL OUTCOME
Table 4: ABNORMALITY AND OUTCOME
Graph 4: ABNORMALITY AND OUTCOME
DISCUSSION Among all the cord abnormalities, the commonest was nuchal cord. Single loop of cord around neck did not significantly affect the mode of delivery or neonatal outcome whereas more than 2 loops of cord around neck were associated with APGAR score less than 7.Our findings are similar to the study done by Dexter Hayes and associates in which they discovered that single loop of nuchal cord was only associated with 1 minute APGAR score <7 whereas multiple loops were associated with increased likelihood of Caesarean section and APGAR score <7 at 1 and 5 minutes. Tight loops of Nuchal cord but not loose were associated with low APGAR score. Among cord knots, adverse neonatal outcome in the form of still birth was associated with true knot. True knots occur due to active fetal movements and cause still birth due to venous stasis causing thrombosis, fetal hypoxia, fetal neurological morbidity and death.7 Although the incidence of cord prolapse in our study was only 1% it was associated with adverse fetal outcome due to delayed referral to our centre. A study by Aarti Jeenwal stated that newborns delivered after umbilical cord prolapse graded lower APGAR scores, less than 7, at 5 minutes and higher rate of perinatal mortality was noted in cord prolapse group. Abnormal cord length was seen in 12% of cases where long cords (more than 100 cm) were found to be associated with nuchal cord and true knot. Single umbilical artery was found in 4% cases of which 1 fetus had associated renal anomaly. In the study by Aarti Jeenwal similar incidence of single umbilical artery was seen of which 20% cases(fetus) had associated cardiovascular anomalies, gastrointestinal defects, renal defects. Vasa Previa was also found in 1 patient where there was still birth due to excessive bleeding before the patient reached our facility. Coiling abnormality includes hyper as well as hypocoiled cords where IUGR was seen in 22% cases and APGAR score less than 7 at 1 min was seen in 22% cases whereas less than 4 at 1 in was seen in 11% cases. The study by Umamaheshwari Guruswamy showed IUGR in 43% cases of hypercoiled cords whereas 29% cases of hypocoiled cords. Velamentous cord insertion was found only in 1 patient which reported to our centre with heavy bleeding per vaginum for which emergency caesarean section was performed and baby had poor APGAR score requiring NICU admission.
Table 5: COMPARISON WITH OTHER STUDIES
CONCLUSION Umbilical cord abnormalities is a stress factor for fetus, where stillbirth can occur due to combination of risk factors.8 The reported rates of umbilical cord abnormalities associated with still birth is reported to be 2.5-30%.9-12 This is especially important because most of these still births occur relatively late in pregnancy in a setting of otherwise normal foetuses and pregnancies. Due to lack of clear knowledge about risk factors, strategies should target entire population. Investigations in the form of biomarkers which will indicate intermittent hypoxia may also be of great value in identifying pregnancies with occult but clinically relevant umbilical cord abnormalities.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home