|
Table of Content - Volume 18 Issue 1 - April 2021
Study of neonatal outcome in relation to placental location in tertiary care centre
Alka Patil1, Bhagyashree Badade2*, Sayli Thavare3
1Professor and HOD, 2Junior Resident, Department of Obstetrics and Gynaecology, ACPM Medical College, Dhule, Maharashtra, INDIA. Email: sonu.badade07@gmail.com
Abstract Background: The human placenta is a complex organ and plays a key role during pregnancy. It serves as a medium by extracting nutrition from the mother and providing it to the growing fetus. As a largest fetal organ, it has indispensable functions in the development and protection of the fetus. The localization of the placenta determined by ultrasound in the second trimester has been hypothesized to have an impact on the pregnancy and therefore pregnancy success. Aims And Objective: To determine the neonatal outcome depending on second trimester placental location between 18-24 weeks and to determine whether it can be considered as a screening tool to predict these complications. Method: This retrospective study is conducted at ACPMMC Dhule. 200 pregnant women with singleton pregnancy, who delivered after 28 weeks of gestation during 1 year period, who had prior documentation of placental location on the basis of antenatal USG performed between 18-24 weeks were included. Placental position was then categorized as anterior, posterior, fundal, lateral and placenta previa. Association of placental location with neonatal outcome was then noted. Result: Out of 200 women, the frequency of central placentation was 166 (82.8%), lateral placentation 32 (16.2%) and placenta previa was 2 (1%). Central placentation had an abnormal outcome in 77(46.3%) and lateral placentas with abnormal outcome were 18(57.2%). Abnormal neonatal outcomes like Intrauterine Growth Restriction (IUGR) (16%), Preterm Birth (31%), and Intrauterine Death (3%) were more in lateral placentation. The number of central placentas having NICU admissions were (14.60%) and lateral placentas with NICU admissions were (29.30%). Additionally, we also found an association between unilateral implantation and low Apgar scores at 1 and 5 minutes in comparison with centrally located placenta. Conclusion: In our study, there is a significant association between lateral placentation and abnormal neonatal outcomes. Therefore, we believe our findings suggest that some aspect of placental implantation in the lateral uterus makes it less favourable for fetal growth than implantation in other sites. Therefore, placental location by Ultrasound examination done in second trimester is used as non-invasive predictor in determining adverse neonatal outcomes. Keywords: Placental location, Neonatal outcome, Lateral Placentation, APGAR score, NICU admissions
INTRODUCTION “Pregnancy and motherhood are the most beautiful and significantly life altering events that a women ever experiences. To be pregnant is to be vitally alive, thoroughly women and distressingly inhabited, making pregnancy a time of transition, growth and profound beginnings.” The human placenta is a complex organ and plays a key role during pregnancy5. It serves as a medium by extracting nutrition from the mother and providing it to the growing fetus. As a largest fetal organ, it has indispensable functions in the development and protection of the fetus. The site of implantation and resultant location of the placenta within the uterus are likely important determinants of placental blood flow and therefore pregnancy success.1 The blood supply of the uterus is not uniformly distributed.2 Centrally located placenta receives equitable distribution of blood flow from both the uterine arteries whereas in laterally located placenta, the uterine artery closer to the side of placenta has a low resistance and a good blood flow, which causes disparity in blood distribution. The other uterine artery supplying the placenta located laterally receives less contribution from the collateral circulation.3 As the anatomical conditions vary across different areas of uterus, both with respect to the shape of the cavity and the blood supply, other placental locations than the previa may also be associated with adverse pregnancy, delivery and infant outcomes. Despite the universal documentation of placental location at the time of the second trimester ultrasound evaluation of the fetal anatomy, a detailed appraisal of that location, with the exception of placenta previa, and its predictability of adverse perinatal and maternal outcomes in a large prospective study has not been undertaken.7Less is known about the possible association of placental location other than previa with pregnancy outcomes.5Unilateral placental implantations (placentas where the bulk of the placenta is implanted over the right or left lateral aspect of the uterus) have been linked with an increased incidence of preeclampsia, fetal distress in labour, abdominal deliveries and intrauterine growth retardation (IUGR). Cornual implantations have been linked with an increased risk of breech presentations, persistent placenta previa with fetal growth restriction, abruption placenta and third trimester bleeding.4 The aim of this study was to find out if the initial site of placental implantation, as determined by ultrasound between 18 and 24 weeks of gestation, is predictive of antepartum complications, intrapartum events, neonatal outcomes and to determine whether it can be considered as a screening tool to predict these complications.4
METHOD Present study was retrospectively conducted in the Department of Obstetrics and Gynecology at JMF’s ACPM Medical College, Dhule. 200 pregnant women with singleton pregnancy, who delivered after 28 weeks of gestation during 1 year period from August 2018 to August 2019, who had prior documentation of placental location on the basis of antenatal USG performed between 18-24 weeks were included. Approval from the Institutional Ethics Committee was obtained. INCLUSION CRITERIA All Primi or Multigravid women. Women with singleton pregnancy. Gestational age between 18-24 weeks. All Primi or Multigravid women coming to our OPD, willing for follow up and delivery at the hospital. EXCLUSION CRITERIA Patients attending OPD after 24 weeks of gestation. Women whose fetus had a structural abnormality. Multiple pregnancies. Rh incompatibility/fetal hydrops. Polyhydramnios/oligohydramnios. Females with unknown last menstrual period.
Informed written consent of all pregnant women was taken. The records of 200 subjects were ascertained. All sonographic examinations were performed in the Radiology Department of same institute, in supine position using Toshiba nemio ultrasound machine attached to a 3.5 MHz curvilinear transducer by the radiologist between 18-24 weeks on same USG machine. It is our departmental policy to offer a routine scan at 18-24 weeks or later if the booking is late, where the details of placental location are recorded apart from other parameters. Trans-abdominal scan were performed in maternal supine position using Toshiba nemio ultrasound machine attached to a 3.5 MHz curvilinear transducer. Maternal demographic information including hospital number, age, parity, LMP, EDD, period of gestation at the time of scan and placental location on second trimester scan were collected. Pregnancy complications and neonatal outcomes were obtained from our hospital records during their routine follow up as per indications and labour room registers. Based on the placental location in the scan, we categorized each placenta into 6 groups as anterior, posterior, fundal, left lateral, right lateral and placenta previa. For the ease of understanding it was simplified into following categories namely central, lateral location and low lying. Central placental location means those which are uniformly distributed, and it includes anterior, fundal or posterior locations. When the greater portions of placenta are confined to one side it is termed as lateral location which may be on left lateral location or on the right lateral location. The following neonatal outcomes were studied: Neonatal Outcomes: IUGR. IUD/ Stillbirth. Preterm delivery. APGAR score.
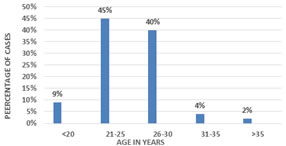
RESULT The study was conducted retrospectively on 200 pregnant women on the basis of placental location. In the present study 85% of the patients were in the age group of 21 to 30 years, 9% were below the age group of 20 years, whereas only 6% were more than 31years of age.
Table 1: Distribution of cases according to Age
Graph 1: Distribution of cases according to Age
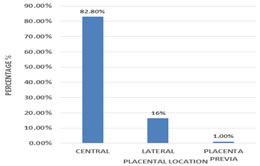
Out of 200 women, the frequency of central placentation was 166(82.8%), that of lateral placentation was 32(16.2%) and 2(1%) were placenta previa.
Table 2: Frequency of Placental Location
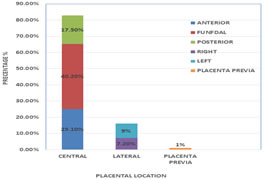
Graph 2: Frequency of Placental Location Further, the study showed that, amongst 166(82.8%) of central placentas: 50(25.1%) had anterior placenta, 35(17.5%) had posterior placenta and major part 81(40.2%) was fundal, whereas amongst 32(16.2%) of the lateral placentation: 7.2% were right lateral and 9% belonged to left lateral group. The frequency of placenta previa was 2(1%).
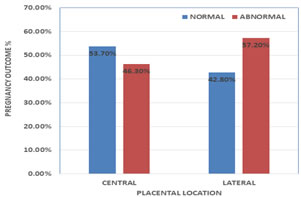
Graph 3: Frequency of Placental Location Out of total cases, 89(53.7%) cases with central placentation had normal outcome and 77(46.3%) had an abnormal outcome, whereas lateral placentas with normal outcome were 14(42.8%) and abnormal outcome was seen in 18(57.2%) cases.
Table 3: Placental Location and Pregnancy Outcome
Graph 4: Placental Location and Pregnancy Outcome
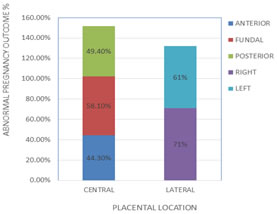
The number of anterior placenta with abnormal outcome was 22(44.3%) and with normal outcome was 28(55.7%). The number of fundal placentae with abnormal outcome was 47 (58.1%) and with normal outcome was 34(41.9%). The number of posterior placentae with abnormal outcome was 17 (49.4%) and with normal outcome was 18 (50.6%). The number of right lateral placenta with abnormal outcome was 10(71%) and with normal outcome was 4(29%). The number of left lateral placenta with abnormal outcome was 11(61%) and with normal outcome was 7(39%).
Graph 5: Placental Location and Abnormal Pregnancy Outcome
Lateral placental location was associated with majority of abnormal outcomes. It was observed that lateral placenta had major NICU admissions maximum of which belong to the high risk group of IUGR and Low APGAR score. Three cases of lateral placental location were associated with 16% risk of IUGR, 7 cases were associated with 31% risk of preterm birth and one case was associated with IUFD/Still birth (3%).
Table 4: Neonatal Outcomes associated with Placental Location
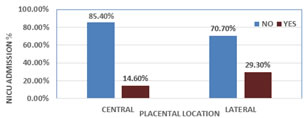
The number of central placentas having NICU admissions were 24(14.6%) and without NICU admissions were 142(85.4%). The number of lateral placentae with NICU admissions were 9(29.3%) and without NICU admissions were 23(70.7%). Table 5: Placental Location and NICU Admissions
Graph 6: Placental locatin and NICU Admissions
DISCUSSION Uteroplacental circulation and studies examining the association between placental location and uterine artery Doppler velocimetry suggest that site of placental attachment in the uterus may be an important determinant of placental blood flow. Abnormal uterine artery blood flow is more likely to occur in pregnancies with unilaterally located placentas. This suggests the possibility that placental location might affect fetal growth.2 Various factors associated with IUGR are maternal malnutrition, infectious agents, maternal vascular disease which have been hypothesized to exert their effects on foetal growth by constraining foetal resources by restricting metabolic substrates, limiting oxygen availability, or curbing foetal blood supply. Given the placenta’s role in fetal blood supply, nutrient and oxygen delivery, it comes as little surprise that placental location itself elevates the risk of IUGR.2 The maternal blood supply to the placenta derives mainly from the uterine arteries, with additional supply from the ovarian arteries.6 In pregnancies with unilateral placentas, uterine artery resistance is lower in the ipsilateral vs. contralateral uterine artery, while in pregnancies with centrally located placentas resistance is similar between the two uterine arteries.2 Ito et al., interpreted this finding in the context of an electrical equivalent circuit model of uteroplacental circulation and suggested that the decreased placental-side uterine artery resistance may reflect decreased uteroplacental blood flow volume in unilaterally situated placentas.7 Kofinas (64), further suggested an anatomic mechanism by which decreased blood flow to a unilaterally located placenta could occur. Perhaps centrally located placentas receive adequate blood flow from both uterine arteries by virtue of their position. Therefore, any deficiency in circulation could lead to decreased blood flow, and, therefore, a higher risk of growth restriction in pregnancies with unilateral placentas.8 In our study we found that, out of 200 women, the frequency of central placentation was 166(82.8%), that of lateral placentation was 32(16.2%) and 2(1%) of placenta previa, which was comparable with the study done by Vidhu Nair et al.,3 Jaiswal et al.,9 Singh et al..10
Table 6:
In the study conducted by Vidhu Nair et al.,3 out of 450 singleton pregnancies, central placentation with abnormal outcome was 182(48.3%) and normal outcome was 195(51.7%). The number of lateral placentas with abnormal outcome was 44(60.3%) and with normal pregnancy outcome was 29 (39.7%). In their study, Lateral placentas had the major abnormal outcomes which was comparable to our study, where out of total cases, 89(53.7%) cases with central placentation had normal outcome and 77(46.3%) had abnormal outcome, whereas lateral placentas with normal outcome were 14(42.8%) and abnormal outcome was seen in 18(57.2%)cases. Similarly, Singh et al.10 also concluded that lateral placenta was associated with more abnormal outcomes, compared to centrally located placentas. Table 7.
In anteriorly located placentas, the incidence of IUGR is found to be 3.3%, preterm birth 10%, and 5% were IUFD. Similar observations were made by Fung et al.,11 where 13 cases of anterior placenta were associated with 7.3% risk of IUD/still birth. Shakluntala Chhabra et al.,12 in their study reported that with anterior placenta, 10 (5%) women had spontaneous preterm labor. Shumaila Zia et al.13 conducted a retrospective study on 474 patients and found that anterior placental location was associated with IUD with an outcome of 1.5%. The study also showed statistically significant association of anterior placenta with IUGR and IUFD. With Fundal location, the incidence of IUGR is found to be 15%, preterm birth 16%, and that of IUFD is 5.1% which is comparable to study done by Shakluntala Chhabra et al.,12 where out of 322 women with fundal placenta, 28 (42.4%) had FGR, 34 (10.6%) had preterm births. Hadley et al.14 reported that a placenta located in the fundus carries a significantly higher risk of premature rupture of the membrane. Shumaila Zia et al.13 revealed a significant association of fundal placentas with IUGR. In our study, with posterior placental location, the incidence of IUGR is found to be 7.4%, preterm birth 14%, and that of IUFD is 4%. This result was correlating with the study done by Singh et al.,10 which concluded that posterior placental location was associated with 62.26% risk of IUGR. Similarly, in the study done by Shakluntala Chhabra et al.,12 (4 of 12) had FGR, 18 (14.6%) women had spontaneous preterm labor. Similar observations were made by Fung et al.,11 Shumaila Zia et al.,13 in their study concluded that preterm labour was associated with posterior placenta with an outcome of 3.7%. Singh et al. 10 concluded that posterior placental location had 50% risk of still birth. In present study with lateral placental location, we found the incidence of IUGR was 16%, preterm birth was seen in 31%, and 3% were IUFD. These results were in accordance with the study conducted by Vidhu Nair et al.,3 where five cases of left lateral placenta were associated with IUGR and abnormal dopplers (10.2%) and Eight cases of left lateral placenta were associated with 16.3% risk of preterm birth. Similarly, Singh et al.10 conducted a prospective study on 592 patients and concluded that lateral placental location was associated with 62.26% risk of IUGR. Seadati et al.,15 showed lateral placentation had 2.7 times risk of developing IUGR. A retrospective study conducted by Jackson et al.16 showed lateral placenta was associated with preterm birth. Kofinas et al.8 used a case-control design to compare placental location in pregnancies with IUGR and/or preeclampsia to placental location in normal pregnancies. They found that in the presence of preeclampsia and/or IUGR, up to 75% of pregnancies had unilaterally located placentas and 25% central placentas, whereas in the absence of these two conditions, 51% of the patients had unilateral and 49% central placentas. Additionally, in the assessment of laterally implanted placenta, Vaillant et al.17 discovered an increased risk of fetal distress, caesarean deliveries, and IUGR compared with centrally implanted placentas. A more recent study by Magann et al.,18 however, examined second trimester placental location and a variety of adverse pregnancy outcomes. This group found an association between unilateral implantation and low Apgar scores (<7) at 1 and 5 minutes 30, which was consistent with our study, where it was observed that lateral placenta had Low APGAR score at 1minute and 5minute. Table 8:
The current study showed, lateral placenta had major NICU admissions. The number of central placentas having NICU admissions were 24(14.6%) and without NICU admissions were 142(85.4%). The number of lateral placentae with NICU admissions were 9(29.3%) and without NICU admissions were 23(70.7%), these results were consistent to the study done by Vidhu Nair et al.,3 where the number of central placentae having NICU admissions were 62 (16.4%) and the number of lateral placentae with NICU admissions were 19 (26%), the number of central placentae without NICU admission were 315 (83.6%) and lateral placenta without NICU admission were 54 (74%). Singh et al.10 concluded that 16% of NICU admissions belong to the high-risk group of IUGR.
CONCLUSION In our study, there is a significant association between lateral placentation and abnormal neonatal outcomes. Therefore, our findings suggest that some aspect of placental implantation in the lateral uterus makes it less favourable for fetal growth than implantation in other sites. Therefore, placental location by Ultrasound examination done in second trimester is used as non-invasive predictor in determining adverse neonatal outcomes.
REFRENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home