|
Table of Content - Volume 18 Issue 3- June 2021
Study of different modes of presentation, diagnosis and management of ectopic pregnancy in tertiary care hospital
Shruti Manchanda
Assistant Professor, Department of OBG, Surat Municipal Institute of Medical Education and Research, Surat-395010, Gujarat, INDIA.
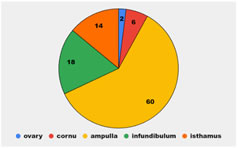
Abstract Background: Diagnosis of ectopic pregnancy was frequently missed and rising trend in incidence of ectopic pregnancies necessitates awareness about risk factors, resultant morbidity and mortality. Aim: To understand the modes of presentation, diagnosis and surgical management of ectopic pregnancy. Methods: This prospective study included 100 patients detected to have ectopic pregnancy in a Municipal Hospital of Mumbai from April 1998 to May 1999. Results: The patients presented with pain in abdomen (88%), Amenorrhoea ( 64 % )and bleeding per vaginum (58%), Abdominal tenderness (66%), tenderness in fornix (60%) and mass in the fornix ( 56 %). Laparoscopy was the most helpful diagnostic method and was positive in all the patients (100%). Abdominal ultrasonography was Positive in 83.37% cases. The commonest site for ectopic pregnancy is ampullary 60% followed by infundibular (18%) and isthmic (14%). Two ectopic pregnancies occurred in the ovary. In the present study, tubal rupture was 72%, unruptured ectopic constituted 18 % and tubal abortion in 10%. Salpingectomy (82%) was performed in the majority of cases. Salpingo- oophorectomy in 16% and conservative surgery was performed in 2% of the cases. Conclusion: To prevent morbidity and mortality the emphasis should be on early diagnosis. With regularly increasing availability of sonography, laparoscopy and blood transfusion facilities, conservative preferably laparoscopy surgery should be performed in patients and future fertility in patients who desire to have a child could be preserved. Key words: ectopic pregnancy, incidence, risk factors, laparoscopy
INTRODUCTION "Ectopic pregnancy" is like a fire alarm to the gynecologist and remains a dramatic gynecologic emergency and a persistent diagnostic challenge. The term "Ectopic Pregnancy" is derived from "NK-TOPUS" i.e. out of place. Thus it embraces all varieties of gestation- outside the uterine cavity.4 Although the incidence of ectopic pregnancy is rising, the complications, morbidity and mortality associated with it have been decreasing. This decline may be related to improved diagnostic techniques and improved management and care. Today Laparoscopy has opened up a new field of accurate diagnosis as well as surgery in these cases. More often the Management approach is shifting from radical to conservative with the help of electro cauterization, laparoscopic surgery and chemotherapy. But in a developing country like ours when ignorance, illiteracy and poverty are at its peak, ectopic pregnancy remains a serious threat, because of late patient arrival, difficulty in management of blood and lack of timely transport and operative facility.5-10 Because of the above reason maternal morbidity and mortality still remain high in our country. This study was undertaken so as to understand modes of presentation, diagnosis and surgical management of this condition. MATERIALS AND METHODS This study included 100 patients detected to have ectopic pregnancy in a Municipal Hospital of Mumbai from January 1998 to April 1999. Approval of the Institutional ethics committee was obtained before the start of the study After the diagnosis of ectopic pregnancy was established, the following patient data were recorded. Data was entered in MS excel spreadsheet and analyzed using SPSS software version 19.0. Data was compiled as frequency and percent
OBSERVATIONS
TABLE 1
Above table 1, In present study the most common presentation is pain in the abdomen, 44% of the cases. Next common presentation is amenorrhea and bleeding per vaginal constitutes 64% and 58% incidence respectively. 22% of cases have vomiting while syncope is present in 4% of the cases.
TABLE 2
Clinical signs elicited by abdominal examination Above table 2 shows that, out of 100 cases the commonest abdominal finding is abdominal tenderness, present in 66% of cases. In 32% of the cases, no positive signs on abdominal examination were elicited.
TABLE 3
Total 60% of the cases had hemoglobin levels less than 8 gm%. Out of which 10 cases are severely anemic with hemoglobin in level less than 6 gm %. High number of anemic cases is because of:
-Poor dietary intake of iron. Poor health education and illiteracy.
Table 4: Specific investigations for ectopic pregnancy
It is clear that laparoscopy is good when diagnosis is doubtful. Laparoscopy is performed in 6 cases, and it is positive in every case (100%). Out of 78cases of urine pregnancy test by pregcolor, it is positive in 68 cases (87.18%) Ultrasonography was done in 60 cases and is positive in 50 cases (83.33%). In 38 cases culdocentesis is performed and it is positive, in 68% of the cases, Abdominal paracentesis was done in 20 cases and was positive is 80% of the cases. Figure 1 The most common is ampulla of Fallopian tube, 60% common site of ectopic pregnancy thereafter, infundibular (18%) and isthmic (14%). Two cases were of ovarian ectopic pregnancy (figure 1).
DISCUSSION The present study is carried out to make a detailed analysis of 100 cases of ectopic pregnancy admitted in a Municipal Hospital in Mumbai in the period of January 1998 to April 1999. The results and other clinical aspects of ectopic pregnancy are compared with other studies. Incidence of ectopic pregnancy varies widely with different studies. The highest incidence amongst other studies is seen.11 Bleeding per vaginum and amenorrhea is seen in 58 and 64 % cases respectively, Uterine bleeding, dark brown, scanty and irregular, is due to decline of hormonal levels after the death of embryo, Amenorrhea is usually of early weeks and sometimes may not be present where scanty last period is present due to hormonal disturbances,12 Sometimes conception occurs in the lactation period, There was one such case in present study. In the present study 64% of the cases had amenorrhea In 8% of the cases, there was scanty last menstrual period, Other symptoms mainly included vomiting, nausea, giddiness, Syncope due to reflex vasomotor disturbances following Peritoneal irritation and hypovolemia is also present. Robins has explained that as associated shoulder pain is due to diaphragmatic irritation. In the present study it is seen in 4% of the cases and all are acute ones.13 Increasing pallor, tachycardia followed by shock are the main clinical signs. It is due to intraperitoneal hemorrhage and it suggests ruptured tubal pregnancy,14 Various authors have shown the incidence of shock from 13.1% to 22.2%. In present study the incidence of shock is 26% which was comparable to previous studies. As reported by many authors the most common abdominal finding is abdominal tenderness present in 70% to 98% of the cases. In the present study it is 66% and comparable with others.15 Tenderness and mass in the fornix were usually present in 60% and 56% of the cases respectively. Uterine size reported to be enlarged in 8.5% to 60.7% of the case in the various studies.15 The wide variation is due to an ill defined uterus due to tenderness. The enlargement is in the response to increased hormonal level. In the present study it is enlarged in 42% of the cases and 50% had a normal size uterus. With facilities of urinary pregnancy tests and high resolution ultrasound examinations, the diagnosis of ectopic pregnancy is easier. Early detection has now become possible before rupture and subsequent complications. The Combined use of both beta hCG estimation and ultrasonography has increased the diagnostic accuracy. I.Stable and J.B. Brudzinskas et al. studied the diagnostic efficacy of abdominal and vaginal ultrasound and serum hCG used alone and in combination with abdominal ultrasound in the diagnosis of ectopic Pregnancy. They have reported combined use of beta hCG and vaginal Sonography is the most important method.16 In the present study abdominal ultrasound was performed in 60 cases out of which it was positive in 50cases 83.33%. In 10 cases (16.66%) it was misleading. Out of these 10, in 4 cases adnexal mass was thought to be of ovarian origin. In one case a patient had Koch’s in which adnexal mass was thought to be tuberculos tubo ovarian mass. In another 4 cases ultrasonography findings were reported as completely normal. Urine pregnancy test was performed in 78 cases, which was positive in 68 cases with positive predictive value in 87.18 of cases and negative in 10 cases. These negative results may be due to: Chronic ectopic pregnancy in which due to necrosis of the chorionic tissue or due to death of embryo the functional trophoblastic mass was greatly reduced. Very low levels of hCG may be detected depending upon the sensitivity of the test used preg-color in this study.17 Out of 100 cases of ectopic pregnancy laparoscopy was performed in 6 cases and positive in all the cases, (100%) in the present study. Although we had 6 cases it is clear that laparoscopy 1s the most important diagnostic aid in ectopic pregnancy. Use of laparoscopy has reduced the error in diagnosis of ectopic pregnancy from 20% to 4%. Most of investigators have found that laparoscopy provides positive diagnosis in more that 90% of the cases.18 Missed diagnosis in 3 to 4% of the cases and is limited to very early ectopic pregnancy Salpingectomy is the treatment of choice in most of the cases when the tube is badly damaged or obstetric career is completed. In the present study it was performed in 82 % of cases Salpingo-oophorectomy is also a radical Surgery performed in (16%) of cases. previous study has explained that after Salpingo-oophorectomy chances of recurrent ectopic Pregnancy is reduced by abolishing the transmigration of ova,19 But in modern times, ovary should be preserved unless the blood supply to ovary is impaired or presence of adhesions or in a case of ovarian pregnancy. Moreover, increasing the facility of fertility by IVF-ET, GIFT etc. In the present study it is performed in 16% of the cases 14% due to adherent ovary 7% and 2% due to ovarian cyst. Conservative surgery is performed in the selected cases by keeping in the mind the age, parity, conditions of the patient. In the present series conservative surgery was performed in 4 of the cases. In the present series,there were 2 cases of ovarian pregnancies in which resection at the hemorrhagic portion of the ovary was done followed by anastomosis at the resected margins.20 Hysterectomy was performed in 6.3% of the cases in Morton and 7.3% of cases in Thomas series. Hysterectomy is indicated in cornual and cervical ectopic pregnancy. In the present study no case of ectopic pregnancy required hysterectomy.
CONCLUSION In Spite of its rising incidence, ectopic pregnancy has become much less dangerous than it used to be, thanks to the availability of highly sensitive pregnancy tests, abdominal and particularly vaginal sonography and above all high degree of suspicion among doctors in the diagnosis of ectopic pregnancy. To prevent this kind of morbidity and mortality the emphasis should be on early diagnosis i.e. in the unruptured stage. For that a very high degree of suspicion amongst the doctors is required. In fact, every patient with a missed period should be seen as a potential ectopic pregnancy case. With gradually increasing availability of sonography, laparoscopy and blood transfusion facilities, conservative preferably laparoscopy surgery should be possible in almost all patients and future fertility in patients who desire to have a child can be conserved.
Acknowledgement I would like to acknowledge Dr. N.M Mayadeo, Prof and HOD, Dept of OBG, Seth GS medical College And KEM hospital, Mumbai and Dr. Vandana Walvekar, Ex Dean, Nowrosjee Wadia Maternity Hospital, Mumbai for their support and guidance
REFERENCES
Tahmina S, Mary Daniel, and Preethy Solomon. Clinical Analysis of Ectopic Pregnancies in a Tertiary Care Centre in Southern India: A Six-Year Retrospective Study. J Clin Diagn Res. 2016 ; 10(10): 13–16.
Policy for Articles with Open Access
|
|
 Home
Home `
`