|
Table of Content - Volume 19 Issue 1- July 2021
A study of correlation of C-reactive protein levels with anti-chlamydia pneumoniae antibodies in asthma patients
Vaishnavi Madavi1*, Renu Bharadwaj2
1Assistant Professor Department of Microbiology TNMCM & BYL Nair Ch. Hospital Mumbai, INDIA. 2Visiting Professor, Department of Microbiology, B.J. Government Medical College & Sassoon General Hospital Pune Maharashtra, INDIA. Email: devaki.vm@gmail.com
Abstract Background: Elevated level of C-reactive protein is a marker of systemic infection. These levels are also expected to increase in asthma. Aim and objective: To study the correlation of C-reactive protein levels with anti-chlamydia pneumoniae antibodies in asthma patients Methodology: Asthmatic patients (both adult and children) attending the chest and TB, pediatric OPD and IPD were selected. The presence of anti-Chlamydial IgM, IgG and IgA antibodies was detected using a species-specific ELISA. The clinical history, clinical findings and the presence of different antibodies were correlated together to stage the patient according to their status of asthma. These results were also correlated with the presence of CRP in blood which has been found to be commonly associated with asthmatic disease. Results and discussion: In pediatric patients (acute and chronic asthma), CRP was present in significant titers in 6/30 (20%) patients. The remaining 24/30 (80%) were negative for CRP. In the adult asthmatic patients, levels of CRP are increased in both acute and chronic patients. A total of 15/70 (21.4%) of adult asthmatics had significant titers of CRP in their blood. Increased titers of C-reactive proteins are observed in patients of acute asthma which have been found to be associated with high IgM titers or moderate titers of IgM and IgG together.
INTRODUCTION Chlamydia pneumoniae is an obligate intracellular bacterium commonly known as ‘energy parasite’. The diseases caused by C. pneumoniae are gradually rising in the industrialised world. More than 50% of adults in U.S and other countries show serologic evidences of past infection with C. Pneumoniae.1 This organism has a propensity to cause chronic infections and is often associated with ciliary dysfunction and epithelial damage in bronchial cells.2Different studies have suggested links between C. pneumoniae and respiratory tract infections like asthma, bronchitis and COPD. Nowadays, the organism is also said to be implicated in many more human pathologies like atherosclerosis3, Alzheimer’s disease4 and arthritis13. Amongst Asian countries, various studies from India, Korea and Japan have reported C. pneumoniae infection in people of all age groups particularly males.5,6,7,8 In India, Studies have been conducted in Madhya Pradesh, Punjab (Chandigarh), UP (Lucknow). The overall seroprevalence rate recorded is from 25-85%. (7, 60, 61) C. pneumoniae plays different roles in the causation or establishment of asthma. An acute C. pneumoniae infection can produce acute exacerbation in already established asthma. Due to its ability to produce a persistent infection, it may induce chronic asthma with ups and downs in the severity and also, primary or secondary C. pneumoniae infection may possibly induce asthma in previously non-asthmatic patients.9 C. pneumoniae infection in airways produces acute inflammation, thereby raising levels of IgM antibodies which appear first in the immune response against C. pneumoniae. This initial inflammation also increases the titers of CRP in the blood within a few weeks following the IgM antibodies. Present study was conducted to see the correlation of C-reactive protein levels with anti-chlamydia pneumoniae antibodies in asthma patients Aim and objective: To study the correlation of C-reactive protein levels with anti-chlamydia pneumoniae antibodies in asthma patients
MATERIAL AND METHODS Present study was a prospective laboratory based study. Study was carried out in department of chest and TB and department of paediatrics at tertiary health care centre during January 2012 to December 2012. Study population was patients presenting with characteristic symptoms of asthma or having medical history of asthma attending OPD and in patient department and 50 controls. Inclusion criteria:
Exclusion criteria:
Study was approved by ethical committee of the institute. A valid written consent was taken from the patients/ parents of ill children after explaining study to them. Total 100 patients were selected as cases. A total of 50 age and sex matched patients were included as controls. Data was collected with pre tested questionnaire. Data included sociodemographic data, clinical history, through clinical examination and investigations. 5cc of blood in adult and 3cc of blood in pediatric patients was collected in a sterile plain vacutainer. These vacutainers were kept at room temperature for 30 minutes allowing the blood to clot. Sera were separated by centrifugation at 1800rpm for 30 minutes. The separated sera were collected in Eppendorf vials and stored at -200C (in a deep freezer) until further testing. Haemolyzed samples were not processed and repeat blood samples were requested and collected. The sera were tested for presence of anti-Chlamydia pneumoniae IgM, anti-Chlamydia pneumoniae IgG and anti-Chlamydia pneumoniae IgA antibodies using commercially available kits (NovaTec Chlamydia pneumoniae ELISA). Presence of C-reactive protein was tested by commercially available latex agglutination test kit (RHELAX-CRP) Interpretation of test was done as follows. Semiquantitative test-(by dilution of serum) Table 1:
Data was entered in excel sheet. Comparison of C-reactive protein with asthma was done by applying Chi-square test and Fisher’s Z-test. p value < 0.05 is considered as statistically significant.
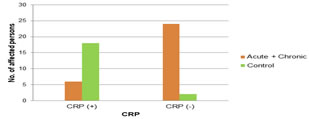
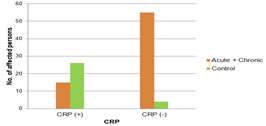
RESULTS In pediatric population majority of the patients (56.7%) were from 9-12 years. Males outnumbered the females (males-66.6% and females-33.4%). In adult population, majority of the patients (27.1%) were from age group of 51-60 years. Here also males outnumbered the females (males-57.1%, females-42.9%). Amongst asthmatic children (30/100), 12/30 (40%) suffered from acute asthma and the remaining 18/30 (60%) suffered from chronic asthma. In 70/100 adult asthmatics, 25/70 (35.7%) suffered from acute asthma and the remaining 45/70 (64.3%) suffered from chronic asthma. In 100 asthmatic patients, 70% patients had anti-Chlamydia pneumoniae antibodies while in 50 non asthmatic patients, 36% patients had anti-Chlamydia pneumoniae antibodies. In our study, we found that in pediatric patients CRP was present in significant titers in 6/30 (20%) patients. Of these five patients (41.7% i.e.5/12) were acute asthmatics and one (5.6% i.e.1/18) suffered from chronic asthma. This favours the relation between inflammatory condition and raised CRP. The remaining 7/12 (58.3%) in acute asthma and 17/18 (94.4%) in chronic asthma were negative for CRP. These values are statistically significant by applying Chi-square test (p-value 0.0154 i.e. < 0.05). (table 1) Considering the relation between CRP and clinical status of asthma, we found that in adult asthmatics, levels of CRP are increased in both acute and chronic patients. A total of 15/70 (21.4%) of adult asthmatics had significant titers of CRP in their blood. Out of the 15 patients who had significant titers of CRP 12 (48% i.e. 12/25) were suffering from acute asthma and 3 (6.7% i.e. 3/45) were from chronic asthma. The values are statistically significant by applying Chi-square test (p-value < 0.0001 i.e. < 0.05). (table 2) In pediatric patients (acute and chronic asthma), CRP was present in significant titers in 6/30 (20%) patients. The remaining 24/30 (80%) were negative for CRP. This favours the relation between inflammatory condition and raised CRP. Amongst controls all were positive for CRP except two.(fig 1) In the adult asthmatic patients, levels of CRP are increased in both acute and chronic patients. A total of 15/70 (21.4%) of adult asthmatics had significant titers of CRP in their blood. The remaining 55/70 (78.6%) patients were negative for CRP. Amongst controls 26/30 (86.7%) had significant levels of CRP while four (13.3%) were negative for CRP. (fig 2) In pediatric asthmatic patients, a total of six patients (6/30) had raised CRP. Five out of these had high IgM titers as the initial primary response against C. pneumoniae and one patient had IgM and IgG together as a late primary response. 14/30 pediatric asthmatic patients (7 acute and 7 chronic) none had anti-chlamydial antibodies and CRP in blood. (table 3) Table 4 shows the correlation between the anti-Chlamydia pneumoniae antibodies and CRP titers. Significant titers of CRP in adult asthmatic patients were found in 15/70 patients. Correlating these findings with anti-Chlamydia pneumoniae antibody, we found that majority of the patients (10/15) had IgM antibodies. The remaining five had IgM and IgG antibodies together in moderate to high titers.
Table 1: Relation showing presence of CRP with clinical state of asthma in pediatric patients
Table 2: Relation showing presence of CRP with clinical state of asthma in adult patients
Figure 1: Relation showing presence of CRP with asthmatic and control pediatric patients
Figure 2: Relation showing presence of CRP with asthmatic and control adult patients Table 3: Correlation between the presence of antibodies with CRP in pediatric asthmatic patients
Table 4: Correlation between the presence of antibodies with CRP in adult asthmatic patients
DISCUSSION Considering the relation between CRP and clinical status of asthma, we found that in pediatric patients CRP was present in significant titers in 6/30 (20%) patients. Of these five patients (41.7% i.e.5/12) were acute asthmatics and one (5.6% i.e.1/18) suffered from chronic asthma. This favours the relation between inflammatory condition and raised CRP. Levels of CRP are increased in both acute and chronic patients in adults. A total of 15/70 (21.4%) of adult asthmatics had significant titers of CRP in their blood. Out of the 15 patients who had significant titers of CRP 12 (48% i.e. 12/25) were suffering from acute asthma and 3 (6.7% i.e. 3/45) were from chronic asthma. This clearly shows that inflammatory disease caused by C. pneumoniae was responsible for increase in CRP titers. Jovonen et al.12 and Sävykoski et al.13 have also reported similar finding regarding C. pneumoniae and CRP in asthmatics. The remaining 13/25 (52%) in acute asthma and 42/45 (93.3%) in chronic asthma were negative for CRP. From all this findings it can be concluded that in acute asthma and also in the stages of early chronic asthma, there is excessive inflammation of respiratory tract as well as airways remodeling due to C. pneumoniae infection and this leads to high CRP titers in such patients. Considering the relation between CRP and clinical status of asthma, we found that in pediatric patients (acute and chronic asthma), CRP was present in significant titers in 6/30 (20%) patients. The remaining 24/30 (80%) were negative for CRP. This favours the relation between inflammatory condition and raised CRP. Amongst controls all were positive for CRP except two. This was due to the inflammatory condition associated with the disease or operative state of the control patients. The two patients with negative CRP levels suffered from undescended testis and phimosis (non-operated). These values are statistically significant by applying Chi-square test (p-value < 0.0001 i.e. < 0.05). Considering the relation between the CRP and clinical status of asthma, we found that in the adult asthmatic patients, levels of CRP are increased in both acute and chronic patients. A total of 15/70 (21.4%) of adult asthmatics had significant titers of CRP in their blood. The remaining 55/70 (78.6%) patients were negative for CRP. Amongst controls 26/30 (86.7%) had significant levels of CRP while four (13.3%) were negative for CRP. The reason behind is that the most of the cases that we selected for controls were inflammatory surgical cases and in these CRP was positive due to inflammation. The four control in which CRP was negative suffered from non-operated lipoma (3) and diabetes mellitus (1). These values are statistically significant by applying Chi-square test (p-value < 0.0001 i.e. < 0.05). In pediatric asthmatic patients, a total of six patients (6/30) had raised CRP. Five out of these had high IgM titers as the initial primary response against C. pneumoniae and one patient had IgM and IgG together as a late primary response. This signifies that C. pneumoniae infection in airways produces acute inflammation, thereby raising levels of IgM antibodies which appear first in the immune response against C. pneumoniae. This initial inflammation also increases the titers of CRP in the blood within a few weeks following the IgM antibodies. IgG antibodies appear and increase up to a moderate titer which is a normal immune response after infection. 14/30 pediatric asthmatic patients (7 acute and 7 chronic) none had anti-chlamydial antibodies and CRP in blood. This indirectly supports the hypothesis of C. pneumoniae infection-inflammation-antibodies and CRP. From all these things it is quite evident that C. pneumoniae infection in the airways leads to inflammation. Thereby producing antibodies and CRP. Significant titers of CRP in adult asthmatic patients were found in 15/70 patients. Correlating these findings with anti-Chlamydia pneumoniae antibody, we found that majority of the patients (10/15) had IgM antibodies. The remaining five had IgM and IgG antibodies together in moderate to high titers. This signifies that C. pneumoniae infection in airways produces acute inflammation, thereby raising levels of IgM antibodies which appear first in the immune response against C. pneumoniae. This initial inflammation also increases the titers of CRP in the blood within a few weeks following the IgM antibodies. IgG antibodies appear and increase up to a moderate titer which is a normal immune response after infection. In sixteen adult asthmatic patients (9 acute and 7 chronic), none had antibodies or CRP in their blood. This also indirectly supports the hypothesis of C. pneumoniae infection-inflammation-antibodies and CRP. Sävykoski et al.13 correlated the levels of IgA and IgG antibodies in patients of asthma. They reported that elevated levels of serum IgA antibodies are associated with raised levels of CRP in asthmatic patients. And they have also concluded that at least in some asthmatic patients antibodies produced against specific chlamydial antigen might be associated with C. pneumoniae mediated airway inflammation which leads to raised CRP levels in these patients.
CONCLUSION C. pneumoniae produces airway inflammation, there by leading to asthmatic disease, production of anti-Chlamydia antibodies as well as raises CRP titers in such patients.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home