|
Table of Content - Volume 19 Issue 3- September 2021
Second trimester uterine artery doppler analysis in the prediction of preeclampsia and fetal growth retardation: A prospective study
Simmi Salim1, Dev Ravishankar2*, Vinod Kumer VG3
{1Professor, Department of Obstetrics and Gynaecology} {2Associate Professor, Department of Radiodiagnosis} Sree Uthradom Thirunal Institute of Medical Science, Vattapara, Trivandrum, Kerala. INDIA. 3Scientist-B (Medical), ICMR, NIRT, INDIA. Email: simiaqib123@gmail.com
Abstract Background: The aim of the study was to find out the relation between Intra Uterine Growth Retardation in the second trimester with respect to uterine artery pulsatility index. Materials and Methods: The study was a longitudinal cross- sectional study, conducted in one Department of OBG, Sree Uthradom Thirunal Medical College, Thiruvanathapuram. The study started from January 2017 to January 2019. Conclusion: Preeclampsia could be avoided if the pregnant women get a timely intervention to detect that especially Doppler analysis of the UA early in the second trimester. Keywords: Doppler, Preeclampsia, Pregnancy, Ultrasound, Trimester, Maternal death.
INTRODUCTION Around one-tenth of maternal deaths in Asia are associated with hypertensive disorders, among them eclampsia and preeclampsia have the greatest impact on maternal and new born morbidity and mortality. Preeclampsia is considered as the onset of a new episode of hypertension during pregnancy, characterised by persistent hypertension (Diastolic blood pressure ≥ 90 mmHg) and substantial proteinuria (>0.3g/24 hours).1 Preeclampsia ranges from mild to severe as per the clinical characteristics and it is 5-8% in worldwide but it is one in every 10 pregnant women in India and it is varies from urban to rural, rural Indian women experiences higher incidences in getting preeclampsia than the urban Indian.2,3,4 By using Bayes’ theorem in the general accuracy we can assess the prior probabilities in the pregnancies through radiological investigations like Pulsatility Index (PI), calculating the levels of Placental Proteins (PAPPA-A and PIGF)5. By analysing the Uterine Artery Pulsatility Index (UAPI), Mean Arterial Blood Pressure (MAP), and maternal serum PAPP-A and PIGF at the first trimester of pregnancy we can calculate the risk factors for the PE in the pregnant women6. The risk factors for preeclampsia in that gestational diabetes, family history of diabetes or high BP, urinary tract infection, fibroids, and psychological stress during pregnancy are there7,8. Among them there are chances of developing left ventricular systolic and diastolic dysfunction are more9. The PE can cause severe defect in both mother and the foetus when its gets severe. To avoid this, we should do the early detection.
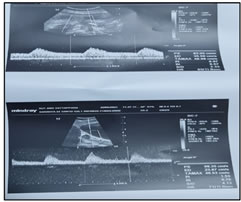
MATERIALS AND METHODS Study design and settings The study was a longitudinal cross- sectional study, conducted in one Department of OBG, Sree Uthradom Thirunal Medical College, Thiruvanathapuram. The study started from January 2017 to January 2019. Procedure Sample size for the present study was calculated by using OpenEpi, version 3.01. The sample size was 139 in 95% Confidence interval with 9.8 % prevalence of pre-eclampsia10. But we included 161 participants to the study after getting the informed consent because of the given time period, but 10 of them could not complete the study because of lost follow up (n=5), miscarriage (n=4) and one Intra Uterine Death (IUD). A total of 151 participants completed the study and the participants were from the gestational age of 11 weeks +0 days to 14 weeks + 0 days. The ultrasound scanning method was used for the study. A Mindray DC-7 ultra sound machine was used. The transducer is placed in the anterior vaginal fornix and a sagittal section of the cervix is obtained. The vaginal probe is then moved laterally until the paracervical vascular plexus is seen. Color flow Doppler is applied and the uterine artery is identified at the level of the cervicocorporeal junction. Measurements are taken at this point before the uterine artery branches into the arcuate arteries. The patients data including name, age, gravida, parity, live births, history of abortion, risk factors like previous LSCS, obesity, PCOD, thyroid problems, gestational diabetes, gestational hypertension, history of previous abortion and intra uterine insemination RAPI, LAPI and outcome of the pregnancy data were recorded. Statistical analysis The data was expressed in number, percentage, mean and standard deviation. Statistical Package for Social Sciences (20.0) version used for analysis.
RESULT Table-1: Distribution of patients based on the demographic and clinical data
Table 2: Distribution of patients based on the previous history and clinical data
Table 3: Distribution of patients based on the pregnancy and out come
Figure 1: Uterine artery Pulsatility index in women according to pregnancy outcomes (N=151)
Description of the Study sample A total of 151 participants 78.0% of them were belong to the age group of 21 years to 30 years (n=118, Range=18-37 years) and the mean age of the participants were 24.74 (SD±3.9). The participants were from the gestational age 11 week+0 days to 14 weeks +0 days and 48.0% participants were from 12 weeks of pregnancy at the first scan (n=72). More than half of the participants were primigravida (53.0%) and 6.60% (n=10) of them had parity of 2. It was found that 83.0% (n=125) of the participants were not have history of abortion (Table-1, 2). More than half of them had several risk factors during their first trimester; they were risk of abortion (19.0%), Hypothyroidism (11.30%), previous history of Caesarean (8.0%), pregnancy induced Hypertension (7.30%), 4% risk for Obesity and PCOD. The mean left uterine artery pulsatility index (LAPI) was 1.27(SD±0.052) and mean right uterine artery pulsatility index was 1.18 (SD± 0.055) about 1.30% developed notch and 11.30% of the patients shown high uterine artery resistance. Around 33.0% of the women took Ecospirin during their pregnancy. Pregnancy and neonatal outcomes It was found that 8.0% of the patients gave birth below 36weeks of their pregnancy about 47.0% of them gave birth at 38th weeks of their pregnancy. More than half of them (52.0%) of them had Full Term Normal Delivery (FTND), among the 26.0% LSCS 17.20% was elective and it was found that 6.0% of them were due to IUGR. Among all Hypertension 17.20% and gestational diabetes 5.0% were prevalent (Table-3). Dopler analysis and maternal and fetal outcomes It was found that patients with Hypertension had an increased chance of getting IUGR (p<0.000) and they have the higher chance for LSCS (p<0.001). When there is an increase in HTN the chances of increased LAPI (p<0.000), RAPI (p<0.000) and Uterine artery resistance (p<0.000) also seen. It had been found that 3.80% of the hypertensive patients had elective LSCS where as 7.70% of the diabetic patients had elective LSCS. And only 1.30% if the diabetic patients were able to complete the full term normal delivery but around 13.0% of the hypertensive patients were able to complete it. When there are patients with HTN they also shown increase in UA resistance (p<0.000) especially they had increased PI(p<0.000). The patients with pre-eclampsia had an increased incidence of IUGR (p<0.000), LSCS (p<0.017) and when there was an increase in gestational age the UA resistance decreased (p<0.000). The intra Uterine Growth retardation increased with mean pulsatility index (p<0.035) especially it had a high significance with right uterine artery pulsatility index (p<0.000) also they had high incidence of LSCS (p<0.004) (Table-3).
DISCUSSION The normal delivery is most common in India11,12. The study shows that there is no significant relation between age and Pre-eclampsia (p>0.89) since majority of the participants were from the same age group of 21-30 years (78.0%)13. Even though the pregnancy associated risk factors can influence the pregnancy out comes14. The lower maternal cardiac output high peripheral vascular resistance is associated with increasing in resistance in the maternal uterine artery and fetal umbilical arteries, Pre-eclampsia are associated with high and low cardiac output of the mother. Especially the increase in the systolic blood pressure (SBP<100 mmHg) is one of the main risk factor for Pre-echlampsia also the diastolic blood pressure, if it goes above 74 mmHg also increase the chance of preeclampsia15. If the percentage of desired body weight in accordance with height increases the chances of pre eclampsia increases 20.0% also the previous history of abortion can influence the worse pregnancy outcomes in accordance with increasing the numbers of abortion16-18. The uterine artery pulsatility index was significantly higher in the women with Intra Uterine Growth Retardation (IUGR) and PE19. The increasing maternal age and parity like maternal factors can increase the incidence of PE20.
CONCLUSIONS Majority of the morbidity and mortality related to Preeclampsia could be avoided if the pregnant women get a timely intervention to detect that especially Doppler analysis of the UA early in the second trimester. Then we can intervene there with effective evidence based clinical management.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home `
`