|
Table of Content - Volume 19 Issue 3 - September 2021
Comparative study of dinoprostone pessary and misoprostol for induction of labour
Pramod Chaudhari1, Sonali Gaikwad2*, Dhanshri Patil3
1,2,3Consultant Obstetrician and Gynaecologist and Postgraduate Teaching Faculty, District Hospital Nashik, INDIA. Email: sonalidrgaikwad@gmail.com
Abstract Background: Induction of labour by use of different drugs is done in indicated cases. Misoprostol and Dinoprostone vaginal Pessary are commonly used for inducing labour to achieve normal delivery.The current study compares the safety and effectiveness of tablet misoprostol and dinoprostone vaginal pessary in induction of labour. Materials and methods: 100 Patients who required labour induction were included in this study. 50 of them received Dinoprostone Pessary (PGE2) and 50 patients received 25mcg of sublingual Misoprostol tablet and dose was repeated every 6 hours for up to maximum of 4 doses. Factors such as induction to delivery time, indications for induction, need of Oxytocin, Mean Bishop’s Score prior to induction, mode of delivery, need for C- section, side effects were studied in detail. Results: The baseline characteristics were similar amongst both groups including mean maternal age, mean BMI, mean gestational age at induction of labour, and the mean Bishop’s score at the commencement of induction of labour. The patients with indication of post-term pregnancy were found to be highest in number with total of 40, of which 42% received tablet misoprostol and 38% in Dinoprostone Pessary group. Followed by Pregnancy induced hypertension with 20% in misoprostol group and 24% in Dinoprostone Pessary group and Preeclampsia with 16% % in misoprostol group and 18% in Dinoprostone Pessary group. Mean Bishop Score on Admission was 3. Mean change in the Bishop’s score after Misoprostol was used for cervical ripening was 6.8. Mean change in the Bishop’s score after Dinoprostone Pessary was used for cervical ripening was 8. Mean change in the Bishop’s score was highly significant. The induction to delivery interval was calculated for both the groups. In Misoprostol group 36 patients had delivery with in 12 hours that is 72% while in Dinoprostone pessary group 39 patients had delivery within 12 hours that is 78%. Delivery with in 24 hours was achieved in 14 patients (28%) in misoprostol group while 11 Patients (22%) in Dinoprostone pessary group.The Common side effects were nausea, vomiting and chills. Hyperstimulation was seen in 6% cases in Misoprostol group while in 2% cases in Dinoprostone Pessary Group. Neonatal outcome was good in all cases. No maternal complications were observed. Vaginal Propess was an effective and safe approach to promote cervical ripening and it was successfully used in induction of labour. Conclusion: Our study results revealed that, dinoprosrone pessary is better inducing agent as compared to the Misoprostol because it has short induction to delivery intervals and thus short duration of labour and advantage of rapid labour as required in cases where quick delivery is comtemplated. The need of Oxytocin augmentation was less with dinoprosrone pessary as compared to Misoprostol. Misoprostol is cost-effective when compared to Dinoprostone Pessary. Misoprostol is stable at room temperature and does not need refrigeration whereas Dinoprostone Pessary requires refrigeration. To conclude Misoprostol and Dinoprostone Pessary both are safe and effective for cervical ripening and labour induction. Keywords: Dinoprostone Pessary, Misoprostol, Induction of labour
INTRODUCTION Induction of labour is defined as the process of artificially stimulating the uterus to start labour. It is usually performed by administering oxytocin or prostaglandins to the pregnant woman or by manually rupturing the amniotic membranes. Over the past several decades, the incidence of labour induction for shortening the duration of pregnancy has continued to rise. It is estimated that in the developed world, at least 19.8% of all labours are induced.1 Methods for labour induction include both mechanical and pharmacological options. Pharmacological interventions to ripen the cervix as part of labour induction include administration of oxytocin, and prostaglandins delivered orally or vaginally. Various preparations of prostaglandin are available differing in their effectiveness, side effects and price.2,3 The preparation most commonly used for IOL is the shorter acting Dinoprostone vaginal gel. Recently longer-acting Dinoprostone preparations (Cervidil and Propess) with retrieval system have become available which have been successfully used for induction of labour. Misoprostol is a synthetic analogue of PGE1. Misoprostol (Cytotec) has been extensively investigated in the past few years for use in cervical ripening and labour induction. the drug is an effective, safe and inexpensive agent for cervical ripening and labour induction. Misoprostol has relative selectivity for the EP3 receptor but also binds to EP2 and stimulates the release of endogenous PGE2, resulting in cervical ripening and increasing uterine contractility. Dinoprostone targets all four EP receptors, activating EP1 and EP3 to increase intra cellular calcium, while EP2 and EP4 stimulate cyclic adenosine monophosphate (cAMP) production. Cervical ripening with Dinoprostone is therefore theoretically similar to endogenous cervical ripening prior to spontaneous labor.4,5 Bishop's score, also known as cervix score is a pre-labor scoring system to assist in predicting whether induction of labor will be required. The total score is calculated by assessing the following five components on manual vaginal examination by a trained professional: Cervical dilation in centimeters ,cervical effacement as a percentage, cervical consistency by provider assessment/judgement, cervical position and fetal station, the position of the fetal head in relation to the pelvic bones Bishop score with less than 6 points indicates that the cervix is unfavorable for induction and probability for vaginal delivery is very low.6 All the selected patients who were given tablet Misoprostol or Dinoprostone vaginal insert had a Bishop score of less than 6 at the time of initiation. The purpose of current study was to determine the effectivity and efficacy of Misoprostol in induction of labour compared to dinoprostone vaginal insert delivery system (brand: PROPRESS) which contains 10 mg of dinoprostone spread on a non-biodegradable polymeric drug matrix.
MATERIAL AND METHODS This comparative study was carried out at Department of Obstetrics and Gynecology at tertiary care center District Hospital Nashik between August 2019 to June 2021. Induction of labour was done in 50 clients with tablet Misoprostol 25ug sublingually and 50 clients with dinoprostone vaginal insert delivery system (brand: PROPRESS). All the selected patients who were given misoprostol tablet or vaginal insert had a Bishop score of less than 6 at the time of initiation. For patients who were given tablet misoprostol for induction of labour was re-examined after every 6 h. If the response of cervix as calculated by Bishop score was found to be less than 6, another dose of tablet was given to the patient. The process was repeated until the initiation of normal contractions keeping in mind that a maximum of four tablets could be given to a single patient. For all those patients who were given dinoprostone vaginal insert, the insert was placed in situ for 24 h initially but was removed if patients started to experience painful contractions or if the patient passed into labour or 30 min before initiation of oxytocin intravenous infusion. Inclusion criteria: Pregnant women with single live fetus and cephalic presentation, Pregnant women with reactive fetal heart rate, post maturity [41 weeks – 42 weeks], Pregnant women with hypertension (pre-eclampsia), Pregnant women with eclampsia and Pregnant women with gestational diabetes. Exclusion criteria: Pregnant women with multiple pregnancies, Pregnant women with abnormal presentations, Pregnant women with previous uterine bleeding, malpresentation, Pregnant women with previous LSCS, Pregnant women with history of surgery on uterus.
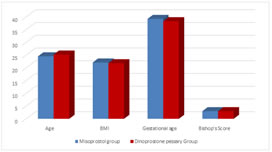
RESULTS During the study period, a total of 100 patients were enrolled whose induction of labour was carried out. Induction of labour was done in 50 clients with tablet Misoprostol 25ug sublingually and 50 clients with dinoprostone vaginal insert delivery system (brand: PROPRESS). The baseline characteristics were similar amongst both groups as shown in Table 1 including mean maternal age, mean BMI, mean gestational age at induction of labour, and the mean Bishop’s score at the commencement of induction of labour.
Table 1: Baseline characteristics
Figure 1: The baseline characteristics
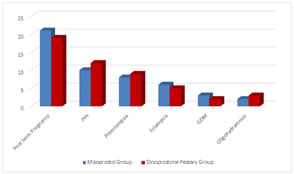
The patients with indication of post-term pregnancy were found to be highest in number with total of 40, of which 42% received tablet misoprostol and 38% in Dinoprostone Pessary group. Followed by Pregnancy induced hypertension with 20% in misoprostol group and 24% in Dinoprostone Pessary group and Preeclampsia with 16% % in misoprostol group and 18% in Dinoprostone Pessary group. The indication of patients for which they were opted for induction labour is summarized in Table 2.
Table 2: Indications of Induction of Labour
Figure 2: Indications of Induction of Labour
Mean Bishop Score on Admission was 3. Mean change in the Bishop’s score after Misoprostol was used for cervical ripening was 6.8. Mean change in the Bishop’s score after Dinoprostone Pessary was used for cervical ripening was 8. Mean change in the Bishop’s score was highly significant. Table 3 shows Bishop’s score on admission and after induction.
Table 3: Bishop’s score on admission and after Induction
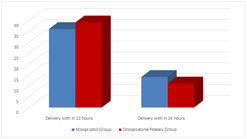
The induction to delivery interval was calculated for both the groups. In Misoprostol group 36 patients had delivery with in 12 hours that is 72% while in Dinoprostone pessary group 39 patients had delivery within 12 hours that is 78%. Delivery with in 24 hours was achieved in 14 patients (28%) in misoprostol group while 11 Patients (22%) in Dinoprostone pessary group. Induction to delivery interval is shown in Table 4. Table 4: Induction to delivery interval
Figure 3: Induction to delivery Interval
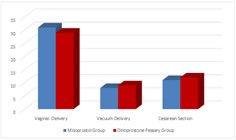
Mode of delivery were Vaginal delivery, Vacuum delivery and Cesarean section. In Misoprostol group 62% had vaginal delivery and 16% required vacuum delivery totalling to 78% by vaginal route while 22% required caesarean section as a route of delivery. In Dinoprostone pessary group 58% had vaginal delivery and 18% required vacuum delivery totalling to 76% by vaginal route while 24% required caesarean section as a route of delivery. Table 5: Mode of Delivery
Figure 4: Mode of Delivery
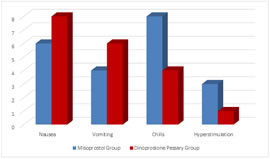
Side effects in both groups are shown in Table 6. The Common side effects were nausea, vomiting and chills. Hyperstimulation was seen in 6% cases in Misoprostol group while in 2% cases in Dinoprostone Pessary Group. Table 6: Side effects
Figure 5: Side Effects
Oxytocin augmentation was required in 14 cases (28%) in misoprostol group and 10 cases (21%) in dinoprostone pessary group. Neonatal outcome in all cases were good and no maternal complications were observed. DISCUSSION Induction of labour is common in obstetric practice. Non pharmacological approaches to cervical ripening and labour induction have included herbal compounds, castor oil, hot baths, enemas, breast stimulation, acupuncture, acupressure, transcutaneous nerve stimulation, and mechanical and surgical modalities. Of these nonpharmacological methods, only the mechanical and surgical methods have proven efficacy for cervical ripening or induction of labour. Pharmacologic agents available for cervical ripening and labour induction include oxytocin and prostaglandins like Misoprostol and Dinoprostone. When the Bishop score is favorable, the preferred pharmacologic agent is oxytocin.7 Propess vaginal delivery system is a pessary containing the active ingredient dinoprostone, which is a naturally occuring female hormone also known as prostaglandin E2. The Propess pessary is inserted high up into the vagina to induce labour. It releases dinoprostone continuously next to the cervix until it is removed (for up to 24 hours). The pessary has a special retrieval tape that allows it to be removed quickly and easily once labour has started, or if there are any problems during the induction. Misoprostol, the synthetic analogue of PGE1, commonly used as a gastric cytoprotective agent.It has several potential advantages, it is stable at room temperature, it is relatively inexpensive and it has been shown to be effective and safe in stimulating uterine contractions.Prostaglandins have been used for induction of labour via cervical ripening for decades.8,9 Prostaglandin E2 insert is considered to be more effective than oxytocin infusion for successful induction of labour. The present study was undertaken to assess the efficacy and safety of misoprostol as compared to the dinoprostone for induction of labour and to assess maternal and foetal outcome. The present study, we observed that the mean time period between application of drug and establishment of regular uterine contractions in misoprostol group and dinoprostone pessary group. The present study, we observed that, the mean time period between application of drug and establishment of satisfactory and regular uterine contractions in misoprostol group was 4.3, dinoprostone pessary group was 6.1. In this study the mean induction to delivery interval was less dinoprostone pessary in the group. Similar results were seen in study in 2013 by Dr Patil P et al.10 In the present study we observed that there was significant improvement in the Bishop’s score after induction with Propess pessary. Mean induction to delivery interval was less in dinoprostone pessary in the group. Rate of vaginal delivery was 76% and rate of caesarean section was 24 %. Fetal outcome was good in all cases. No maternal complications were observed. Chen W et al.11 investigated the efficiency and safety of vaginal Propess as a methodology for cervical ripening and labour induction in full-term pregnant patients with similar results. In our study Oxytocin augmentation was needed in 14 (28%) cases in the misoprostol group whereas in Dinoprostone group 10 (21%) patients required it as compared to study by Neiger R. Greaves.12 Maternal side effects were minimal in both the groups. In Dinoprostone pessary group, 8% patients had chills, 16 % had nausea and 12% had vomiting and 2% had hyperstimulation In Misoprost group, 16% patients had chills, 12% had nausea and 8% had vomiting and 6% had hyperstimulation. Although hyperstimulation was more in Misoprost group but it did not had any effect on the neonatal outcome.13-14
CONCLUSION Tablet Misoprostol and Dinoprostone Pessary both are safe and effective for cervical ripening and labour induction. Misoprostol is cost-effective when compared to Dinoprostone Pessary. Misoprostol is stable at room temperature and does not need refrigeration whereas Dinoprostone Pessary requires refrigeration. Induction to delivery time was slightly shorter in dinoprosrone pessary group when compared to Misoprostone group. One disadvantage with Misoprostol is uterine tachysystole and hyperstimulation with further fetal distress. Although hyperstimulation and meconiumn stained liquor was more in Misoprost group but it did not had any effect on the neonatal outcome. Misoprostol also does not need cold chain storage and is cheaper. Thus Misoprostol can be considered as safe, efficacious and cheap drug for the induction of labour. Our study results revealed that, dinoprosrone pessary is better inducing agent as compared to the Misoprostol because it has short induction to delivery intervals and thus short duration of labour and advantage of rapid labour as required in cases where quick delivery is comtemplated. The need of Oxytocin augmentation was less with dinoprosrone pessary as compared to Misoprostol. To conclude Misoprostol and Dinoprostone Pessary both are safe and effective for cervical ripening and labour induction.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home