|
Table of Content - Volume 20 Issue 1 - October 2021
Long term reversible contraceptive - postpartum IUCD in normal deliveries and cesarean section
Pramod Chaudhari1, Sonali Gaikwad2*, Dhanshri Patil3
1,2,3Consultant Obstetrician and Gynaecologist and Postgraduate Teaching Faculty, District Hospital Nashik, Maharashtra, INDIA. Email: sonalidrgaikwad@gmail.com
Abstract Background: The postpartum intrauterine contraceptive device (PPIUCD) is an effective, reliable, safe and recommended contraceptive method for the postpartum women. This study was conducted to evaluate the safety and efficacy of Immediate Postpartum Intra Uterine Contraceptive Device (PPIUCD) insertion in women delivering vaginally or by caesarean section. Material and Method: Two hundred postpartum subjects after contraceptive counselling included in the study. All eligible antenatal subjects hospitalized for delivery were counselled for PPIUCD. Consent was obtained from those who opted for insertion of PPIUCD. The study subjects were divided into two groups: Group A: Vaginal deliveries (100 cases). GroupB: Intra caesarean Section (100cases). Outcome measures were safety (perforation, irregular bleeding, unusual vaginal discharge, and infection), efficacy (pregnancy, expulsions, and discontinuations), and incidence of undescended IUCD strings, side effects and complications were noted. Results: Out of 200 cases, majority of patients belonged to 21-25 years age group (39%). Mean age of women accepting the PPIUCD was 25years. Majority of the patients opting for postpartum IUCD were primigravida and second gravida patients comprising of 36% primigravida and 32% of second gravida.Among 200 deliveries done around 62% were aware about PPIUCD while 38% were unaware. This can further suggest the awareness levels towards PPIUCD was quite low. Out of 200 cases maximum number of IUCD were inserted intracesarean 100 (50%) followed by 70(35%) post placental and 30 (15%) were inserted postpartum (≤48 hrs). Lower abdominal pain and menorrhagia were the common side effects in both vaginal and caesarean section group. Missing thread due to curling up was more common in caesarean section group while higher expulsion rate was seen in vaginal delivery group. No case of perforation or pregnancy was reported during the study. The reason for removal of IUCD were lower abdominal pain, menorrhagia, vaginal discharge, misplaced IUCD and in 5% cases removal of IUCD was for vague causes. Conclusion: Insertion of IUCD in immediate postpartum period is an effective, safe, and convenient contraceptive intervention in both caesarean and vaginal deliveries. Keywords-Postpartum IUCD, Long term Reversible contraception.
INTRODUCTION Immediate postpartum intrauterine contraceptive device (PPIUCD) is advantageous and cost effective postpartum contraceptive method which provides effective reversible contraception to women in the delivery settings. Most women do not desire a pregnancy immediately after a delivery but are unclear about contraceptive usage in postpartum period. This results in unplanned and undesired pregnancies, which in turn increases induced abortion rates and consequently maternal morbidity and mortality. Continuation of these pregnancies is also related with greater maternal complications and adverse perinatal outcomes.1 In India, 65% of women in the postpartum period have an unmet need of family planning.1 In India current usage of method of contraception is1 Female sterilization 34%2 Male sterilization. 1%3 Pills 4%4 IUD 2%5 Condom 6%6 any traditional method 7%5 Non user 46%. The modern IUCD is highly effective, safe, long acting, coitus independent and rapidly reversible method of contraception with few side effects. It is most cost effective method of contraception today. Many women also find the IUCD to be very convenient because it requires little action once it is in place.2 IUCD in the form of Lippes Loop was introduced in the National Family Welfare Program of the Government of India (GOI) in 1965. Based on the results of clinical trials conducted by the Indian Council of Medical Research (ICMR) in 1972, Copper T 200 B was introduced in the program in 1975. In 1997, ICMR conducted a comparative study between IUCD 200B and 380 A based on which Cu IUCD 380 A was introduced in 2002, replacing CuT 200B in the programme. In 2010, postpartum IUCD (PPIUCD) service was introduced in facilities with high case-load of deliveries. From 2010 till now, postpartum IUCD services are being scaled up in a phased manner throughout the country. In 2012, the Cu IUCD 375 was introduced so that women could choose between Cu IUCD 380 A with a lifetime of 10 years and Cu IUCD 375 with a lifetime of 5 years. In India only 2% of married women of reproductive age use IUCDs, though the last DLHS-3 survey (2007-2008) has shown an increase in the contraceptive use to 54%. Despite the fact that the government offers IUCD services free of cost and IUCD is one of the most effective reversible and safe contraceptive methods, it still remains largely underutilized The postpartum period is a crucial time when the women is highly motivated for accepting a long term, reliable, safe and reversible contraception. At this time, the woman is in hospital for the childbirth and if provide with PPIUCD, she leaves the hospital with an efficient contraceptive in place. PPIUCD insertion is an exceptional opportunity to offer postpartum contraception to rural women having marginal access to medical care and infrequent and inaccurate postpartum visit because of socioeconomic reasons.3 Immediate PPIUCD insertion is labelled when intra uterine device is inserted within 10 minutes to 48 hours of expulsion of placenta and during caesarean section. Moreover, PPIUCD is an ideal contraceptive method advised during this period as there is no interference with breastfeeding and allows women to obtain safe, long acting, highly effective contraception while women is already under medical specialist observation.1,4 Further, in developing countries like India, delivery might be the only time when a healthy woman is in contact with the health care provider and her chances of returning for contraceptive advice are uncertain. Moreover, there are studies that show that in India, 65% of women in postpartum period have an unmet need for contraception.1 In another study, it was shown that IUCD insertion rate was as high as 95% in patients willing for immediate postpartum insertion, whereas this rate decreased to only 45% in those consenting for a later insertion.5 Thus contraceptive counselling measures should included in ante partum period and immediate PPIUCD insertion for those who are willing. This study was conducted to evaluate the safety and efficacy of Immediate Postpartum Intra Uterine Contraceptive Device (PPIUCD) insertion in women delivering vaginally or by caesarean section.
MATERIAL AND METHODS This study is conducted at District Hospital Nashik between August 2019 to April 2021 in Department of Obstetrics and Gynaecology. Two hundred postpartum subjects after contraceptive counselling included in the study. All eligible antenatal subjects hospitalized for delivery were counselled for PPIUCD. Consent was obtained from those who opted for insertion of PPIUCD. The study subjects were divided into two groups: Group A: Vaginal deliveries (100 cases). Group B: Intra caesarean Section (100cases). Inclusion criteria All antenatal patients admitted for delivery to our hospital were counselled for PPIUCD. Consent was obtained from those, who opted for insertion; among those who fulfilled the following criteria were considered for inclusion.
Exclusion criteria
Counselling was done during antenatal visits or during early labour and a written informed consent was taken prior to insertion. This was placed in uterine fundus with the help of long and curved forceps without lock (Kelly’s Forceps) for vaginal insertions, within 10 minutes to 48 hours of removal of placenta. During caesarean section the IUCD was placed at fundus of uterus through the lower segment incision which was closed subsequently as routine. The IUCD strings were not trimmed in both types of insertions and left in uterine cavity. Active management of third stage of labour was performed as routine. All PPIUCD insertions were done by doctors who had been trained for this purpose. Postinsertion counselling was done and women were advised to follow-up for examination at our centre after 6 weeks. Subsequent visits after 3 months and 6 months. Follow up schedule was done at 6 weeks after insertion and the following things were assessed:
Outcome measures were safety (perforation, irregular bleeding, unusual vaginal discharge, and infection), efficacy (pregnancy, expulsions, and discontinuations), and incidence of undescended IUCD strings, side effects and complications were noted.
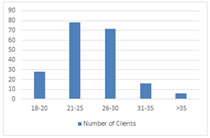
RESULTS Out of 200 cases, majority of patients belonged to 21-25 years age group (39%). Mean age of women accepting the PPIUCD was 25years.Table 1 shows age wise distribution of patients. Table 1: Age wise Distribution (N-200)
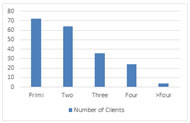
Majority of the patients opting for postpartum IUCD were primigravida and second gravida patients comprising of 36% primigravida and 32% of second gravida. Table 2 summarises the distribution of patients according to parity.
Table 2: Distribution by Parity (N-200)
Figure 2: Distribution by Parity
As per table 3 among 200 deliveries done around 62% were aware about PPIUCD while 38% were unaware. This can further suggest the awareness levels towards PPIUCD was quite low. Table 3: Distribution of Cases according to type of delivery and Awareness (N=200)
Out of 200 cases maximum number of IUCD were inserted intra caesarean 100 (50%) followed by 70(35%) post placental and 30 (15%) were inserted postpartum (≤48 hrs) as shown in table 4. Table 4: Timing of Insertion (N-200)
In this study mothers who were counselled during antenatal care (62%) were more willing to utilize PPIUCD than those who were counselled during early labour (26%) and after delivery (12%). This finding is similar to studies conducted in different regions of India.6,7 This might be that mothers undergoing labour are much more concerned about the birth outcome than contraception. In addition, at this time mothers do not have the time to discuss with their partner. However, antenatal care counselling can solve such constraints. The mothers have the time to discuss their fears about postpartum IUCD and discuss their reproductive health plan with their partners. In follow up cases side effects like pain, menorrhagia, vaginal discharge, missing thread and expulsion were seen as shown in Table 5. Lower abdominal pain and menorrhagia were the common side effects in both vaginal and caesarean section group. Missing thread due to curling up was more common in caesarean section group while higher expulsion rate was seen in vaginal delivery group. No case of perforation or pregnancy was reported during the study.
Table 5: Side effects and complications of PPIUCD
The reason for removal of IUCD were lower abdominal pain, menorrhagia, vaginal discharge, misplaced IUCD and in 5% cases removal of IUCD was for vague causes. The detailed summary of reasons for removal of IUCD are shown in Table 6.
Table 6: Reasons for Removal of PPIUCD
DISCUSSION The average age of the patients accepting PPIUCD was 25 years close to those found in the literature as in Morison et al. study.8 This may be because the fertility is higher in this age and majority of women admitted with full-term pregnancy were from the same age group. Studies by Usha Ram et al., Halder et al. and Kanwat B et al. also observed the same findings.9,10 Acceptance of IUCD was the most common among primigravida clients (36%). In case of multiparous, it was 32% for second gravida,18% for third gravida 12 %for fourth gravida; thus, this finding is consistent to that of the study by Grimes et al. where they found higher acceptance in multiparous clients (65.1%).4 Lower abdominal pain and menorrhagia were the common side effects in both vaginal and caesarean section group. Missing thread due to curling up was more common in caesarean section group while higher expulsion rate was seen in vaginal delivery group. Different studies report different rate of bleeding PV after PPIUCD insertions varying from 23.5% as reported by Mishra S et al. to as low as 5.5% by Kumar S et al.,11,12 and Halder et al.10 found 30% of missing tails in caesarean group and 17.7% in vaginal group, whereas Hooda R et al. found a rate of missing tails of 55.1% in caesarean group and 22.1% in vaginal group.13 In the present study, one of the main observations at follow-up was that of undescended IUCD strings, the incident of missing strings is found in 10% in vaginal group and 16% in caesarean group The practice of leaving the full length of IUCD string in uterine cavity during caesarean section and not passing it through the cervix, unlike study by Celen et al., may have had a role in the significant difference in the incidence of undescended strings in intracaesarean insertions. Our technique might also be the reason for lower expulsion rates as compared to study by Celen et al. (5.3%) for intracaesarean IUCD insertions at 6 weeks of follow-up.15 Counselling the women and confirmation of IUCD in uterine cavity by ultrasound are important to reassure the women and encourage them to continue with the device. Expulsion of Cu T is 8% in vaginal group as compared to 5% in caesarean group. Low expulsion in caesarean group may be because of the better fundal placement of Cu T under visualisation. Gupta et al. also reported low expulsion after caesarean expulsion than vaginal delivery. In the present study, even if we combine the discontinuations (removal of IUCD for different medical or personal reasons) and spontaneous expulsions we still have a commendable IUCD continuation rate of 77.5%. In the absence of PPIUCD insertions, these women would have left the hospital premises without effective postpartum contraception. Similar rates of removal of PPIUCD have been reported in recent studies (12, 13,15).
CONCLUSION Immediate postpartum intrauterine contraceptive device (PPIUCD) is advantageous and cost effective postpartum contraceptive method which provides effective reversible contraception to women in the delivery settings. Postpartum period is the period when patient is highly motivated for contraception and can be easily counselled. PPIUCD has a huge potentiality and abundant scope in India and if widely used it will have a strong impact on population control and will prevent unplanned pregnancy and its sequelae. Follow-up examinations are important to identify spontaneous expulsions and provide alternative contraceptives or IUCD reinsertions. Insertion of IUCD in immediate postpartum period is an effective, safe, and convenient contraceptive intervention in both caesarean and vaginal deliveries.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home