|
Table of Content - Volume 20 Issue 1 - October 2021
Evaluation of the maternal and fetal outcome in multiple pregnancies in third trimester at tertiary care center
V Uma1*, S Nagamani2, B Aruna3
1Assistant Professor, 2Professor, 3Associate Professor, Department of Obstetrics & Gynaecology, MGMH Petlaburz Osmania Medical College, Koti, Hyderabad, INDIA. Email: veludandiuma11966@gmail.com
Abstract Background: The frequency of Multiple pregnancies varies among different regions, countries and populations mostly due to the variation in dizygotic twinning. Twin pregnancy is associated with adverse maternal and fetal outcomes. Dizygotic twinning is much more common than monozygous splitting of a single oocyte, and its incidence is influenced by race, hereditary, maternal age, parity and especially fertility treatment. By contrast, the frequency of monozygotic twin births is relatively constant worldwide-approximately one set per 250 births, and this incidence is generally independent of race, heredity, age and parity. One exception is that zygotic splitting is increased following ART. Aim: Early diagnosis and a good antenatal care to identify the high risk factors Timely intervention to prevent the maternal and fetal morbity and mortality The goal of this study is to evaluate the maternal and fetal outcome in twin pregnancies Materials and Methods: This retrospective observational study was carried out at MGMH petlaburz under Osmania Medical College and for a period of 4 years from January 2016 to December 2019 after obtaining IEC approval . During this period total deliveries -69,742 16,459 (2016);16,999 (2017) 18,063(2018) 18,221(2019) during the study period. Out of them, 1245 were twin deliveries during study period of 4 years with 311twin deliveries per year. Results: There were 69,742 deliveries during the study period. Out of them, with 311twin deliveries per year. The incidence of twin pregnancy was found to be 1 in 56 pregnancies or 1.7% or 17 per 1000 births. Maximum number of women belonged to age group of 21-25 years (57%). The mean maternal age was 26.1 years. 52% of women were multipara. The mean gestational age at delivery was found to be 35 weeks Pre-term labour resulting into preterm delivery was found to be the most common complication of twin pregnancy. 53.7% of women delivered before 37 completed weeks of gestation. Fetal malpresentation was found in 48.2%, maternal anaemia was the commonest medical complication (31.2%). Cephalic-cephalic was the commonest presentation (41.8%) followed by cephalic –breech and breech –cephalic (18% each). Transverse-cephalic was the least common presentation. (0.6%). Caesarean sections are more in present study with 56%. Most of the patients are with low birth weight(53%) followed by low APGAR score. Conclusion: More vigilance during the antenatal period and intra partum care is needed for proper selection of mother for mode of delivery. Active fetal surveillance and thorough maternal monitoring and timely intervention with appropriate neonatal care will improve maternal and fetal outcome Keywords: Twin pregnancy, Low birth weight, Maternal complications
INTRODUCTION The incidence of multiple pregnancies varies significantly among different regions, countries and populations. In several overview studies (since the early 1970) it was found that natural twinning rates were less than 8 twin births per 1000 births in East Asia and Oceania, 9-16 per 1000 births in Europe, USA and India and 17 and more per1000 births in African countries.1-5 Smith et al. reported that India has twining rates below 9 per 1000 births.1,2,3 Multiple pregnancy results in premature delivery, lower one-year survival in multiple infants compared to singletons. Common maternal complications reported in various studies are nutritional anaemia, pregnancy induced hypertension, antepartum haemorrhage, polyhydramnios, preterm labour and postpartum haemorrhage. Twins are more susceptible than singletons. They have lower birth weight and are often premature. They have higher risk of fetal and neonatal morbidity and mortality. The frequency of underweight new-borns and increased congenital anomalies. In India, up to 1% of the pregnancies are twin gestation and 10% of perinatal mortality can be attributed to twin pregnancies, a few studies conducted in India have reported a frequency of twin pregnancy.4,5 Inconsistency in reporting the frequency of multiple pregnancy could be due to structural differences in the populations studied and design effect and systematic errors, in addition to changes in the frequency of the interested outcome over time. In India, studies on the incidence of twin pregnancies and risk factors are very limited. Thus, conducting study to evaluate the maternal and fetal complications in twin pregnancies.
MATERIALS AND METHODS This retrospective observational study was carried out at Osmania Medical College and Hospital for a period of 3 years from January 2016 to December 2019 after obtaining IEC approval. During this period total 8764 deliveries during the study period. Out of them, 311 were twin deliveries. Inclusion Criteria: Pregnant Women who delivered twins at or after 28 weeks of gestation at our institute, during the stipulated study period. Exclusion Criteria: Women with twin pregnancy, delivering at gestational age < 28 weeks. The hospital medical records of the stipulated study period were analysed to collect data of the study subjects. A predesigned format was used to record data pertaining to maternal characteristics, such as maternal age, parity (primiparous vs. multiparous), registration status (booked/un booked) nature of conception (natural/induced) and family history of twins, gestational age at the time of delivery (weeks), fetal presentation(cephalic/Other than cephalic), mode of delivery (vaginal vs. caesarean), maternal medical complications, which included anaemia, preeclampsia, eclampsia, obstetrical complications such as antepartum haemorrhage, premature rupture of membranes, pre term delivery, fetal distress, cord prolapsed, retention of second twin , post-partum haemorrhage, nature of birth (live birth/ still birth), sex, APGAR score at birth and birth weight of neonates. Before conduct of the study, ethical clearance was obtained from the College. Written informed consent was obtained from every study participant before the interview by explaining the objective of the research. All the information collected from the study participants were handled confidentially through omitting their personal identification, conducting the interview in private place and using the data for the research purpose only. Statistical analysis was carried out using SPSS 11.0 for Windows (SPSS Inc., Chicago, IL, USA) statistical software. Categorical variables were described using frequency distribution and compared by chi-square and Fisher’s exact test. For continuous variables, descriptive statistics were calculated and reported as Mean±Standard Deviation. Student-t was used to compare mean scores of continuous variables between two groups. A p value of less than 0.05 was considered statistically significant.
During this period total deliveries -69,742 16,459 (2016); 16,999 (2017) 18,063(2018) 18,221(2019) during the study period. Out of them, 1245 were twin deliveries during study period of 4 years in which we have considered 311 twin deliveries. The incidence of twin pregnancy was found to be 1 in 56 pregnancies or 1.7% or 17 per 1000 births.
Table 1: Distribution of pregnant mothers with variable
Maximum number of women belonged to age group of 21-25 years (57%). The mean maternal age was 26.1 years. 52% of women were multipara. Family history of twins was found in 10% of women. The mean gestational age at delivery was found to be 35 weeks Table 2: Pregnancy complications in present study
Pre-term labour resulting into preterm delivery was found to be the most common complication of twin pregnancy. 53.7% of women delivered before 37 completed weeks of gestation. Fetal malpresentation was found in 48.2%, maternal anaemia was the commonest medical complication (31.2%) in present study.
Table 3: Fetal presentations in present study
In present study, Cephalic-cephalic was the commonest presentation (41.8%) followed by cephalic –breech and breech –cephalic (18% each). Transverse-cephalic was the least common presentation. (0.6%).
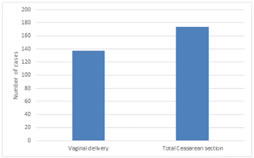
Figure 1: Mode of delivery in present study Caesarean sections are more in present study with 56%.
Most of the patients are with low birth weight (53%) followed by low APGAR score. DISCUSSION Multiple pregnancies are associated with significantly higher maternal and neonatal morbidity and mortality. Women pregnant with multiples are nearly six times more likely to be hospitalized during pregnancy, more than twice as likely to be admitted to the adult intensive care unit and to die compared with women with singleton pregnancies. Incidence in our study was be 1 in 56 pregnancies or 1.7% or 17 per 1000 births. Kamlesh Kumari et al.6 study twin pregnancies over 4 years shows the twinning rate to be 16.5/1000 deliveries. There is a wide variation in incidence rates among the world countries and the Indian subcontinent depending on the racial and geographical factors ranging from 6 to 18 per thousand .7,8,9 This study incidence rate matches with the literature, though it is on the higher side of the range. This could be because the study represents a cross-section of high-risk pregnancies referred to this tertiary center with anticipated complications to mother and foetus. In our study Maximum number of women belonged to age group of 21-25 years (57%). The mean maternal age was 26.1 years. 52% of women were multipara. Family history of twins was found in 10% of women. The mean gestational age at delivery was found to be 35 weeks kamlesh Kumari et al. study majority were in the age between 21-30 years, with a mean age of 28.11±4.68 years. Almost similar mean maternal age of 28.3±4.05 years (range 20- 40 years) was observed from the study done by Jhaveri RR and Nadkarni TK at Nowrosjee Wadia Maternity Hospital .10 Lee YJ et al., in their analysis from Seoul, Korea showed the increased average age of twinning in mothers who had assisted contraception with average age of 32.0±1.4.11 There is no difference seen in distribution of twin pregnancy cases according to primigravida and multigravida group. In our study Pre-term labour resulting into preterm delivery was found to be the most common complication of twin pregnancy which is nearer to that reported by other studies 62.5% by Pandey M.R.et al. and 53.8% by Ri-Na Su et al.12,13 It is higher than reported (44%) by Sultana H. and Chowdhury S. et al. and quite lower than reported (84%) by Bangal et al.14,15,16 In present study 53.7% of women delivered before 37 completed weeks of gestation which is similar to the mean gestational age reported by Muzhar et al. from Pakistan.17 There was no maternal mortality in this study. This was achieved by MULTIDISCPLINARY APPROACH- active management of 3rd stage of labor, round the clock availability of blood products, anaesthetist and Maternal Intensive Care Unit. Present finding is consistent with the studies conducted by Masuda S and Sultana H who did not report any maternal mortality.14,18In present study, Cephalic-cephalic was the commonest presentation (41.8%) followed by cephalic –breech and breech –cephalic (18% each). Upreti P.study showed 43.8% of twin pairs had cephalic-cephalic presentation, 19.3% cephalic-non- cephalic and 36.9% non-cephalic presentation of first twin. The corresponding figures by Masuda S et al. were 48% cephalic-cephalic presentation, 16% cephalic-non- cephalic and 36% non-cephalic first twin.18 In our study Casarean sections are more in present study with 56%. The corresponding figures reported by Pandey MR et al.12 were 48% for the second twin.11 Present finding is comparable to the results reported by other studies such as 56% (Sultana H), 42% (Obiechina NJ et al.).21,22 The higher caesarean section rate in present study was due to malpresentation of first twin, Preterm premature rupture of membranes, fetal distress and previous caesarean section. Most of the patients are with low birth weight (53%) Incidence of low birth weight was same as in present study similar to Ri-Na Su et al. from Bejing. (46.6%) 19 The low birth weight in twin deliveries is due to prematurity and intrauterine growth restriction caused by the pregnancy complications associated with twin pregnancy such as hypertension and anemia. Other fetal complications that were seen included neonatal asphyxia (low APGAR score), IUGR and birth weight discordance (4-5%). Perinatal mortality at 9.5% in present series, Kamlesh Kumari et al., study showed Perinatal mortality at 12.9% was less compared to other Indian studies.6 All cases were of early neonatal death. Variable rates of perinatal mortality (0.8- 2.6/1000 births) have been described in the literature.18 Fewer complications are seen in dichorionic than monochorionic twins. Good neonatal facilities(NICU) probably helped us to attain this good result.
CONCLUSION Management of twin pregnancies is a challenging task for obstetricians. Twin pregnancy rates were more in the younger age group. Maternal complications during twin pregnancy were mainly preterm labour, diabetes, hypertension and anaemia. Caesarean section was the main mode of delivery in indicated cases in this study. Dichorionic gestations had less fetal complications and low perinatal mortality probably due to better biology. Fetal complications were in the majority related to intrauterine growth restriction. More vigilance during the antenatal period and labour is needed for proper selection of mode of delivery. Active fetal surveillance and intervention with appropriate neonatal care can improve fetomaternal outcome.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home