|
Table of Content - Volume 20 Issue 1 - October 2021
Significance of maternal C-reactive protein in preterm prelabor rupture of membrane and its association with histopathological chorioamnionitis
Varsha Sinha1, Jyothi Harish Rao2*
1Postgraduate, 2Professor, Department of OBG, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, INDIA.
Abstract Background: Evaluate the diagnostic accuracy of C- reactive protein (CRP) in the association of chorioamnionitis following Prelabor Premature Rupture of Membrane (PPROM). Study maternal and fetal outcome. Material and Methodology: The study was conducted at Government Lady Goshen Hospital and KMC Attavar Mangalore associated with Kasturba Medical College, Mangalore. The study was a time bound observational study done over the period of September 2018 to August 2020. CRP was sent for all PPROM patient between 28 weeks to 36 weeks 6 days gestation and clinical signs of chorioamnionitis are noted. CRP levels above 8 mg/dl was considered positive. Placental membranes were sent for histopathological examination (HPE). Result and Conclusion: In this study of 100 cases, 47% of patient belong between the gestational age of 32 – 34 weeks. 56% of the study cases were CRP positive and 12% of CRP positive patient had clinical sign of chorioamnionitis. On HPE only 11% of the total CRP positive patient had HCA which was statistically insignificant. The incidence of HCA was found to be higher when the time of onset of PPROM was > 24 hours and is found to be statistically significant. Maternal pyrexia and foul-smelling vaginal discharge are found to be a specific clinical sign. HCA does not correlate to the CRP value in this study and found to be statistically insignificant. Keywords: PPROM, CRP, histopathological chorioamnionitis (HCA), Histopathological examination (HPE), Preterm, Prelabor
INTRODUCTION Preterm prelabor rupture of membranes (PPROM) is defined as the leakage of amniotic fluid<37 gestational weeks, which precedes the onset of regular uterine contraction.1 The incidence of PPROM is 5-10% of all deliveries.2 It is one of the important causes of preterm delivery and perinatal mortality. Preterm prelabour rupture of membrane has been strongly associated with histopathological chorioamnionitis. Chorioamnionitis (CAM) is also known as intra amniotic infection is an inflammation of the fetal membrane due to bacterial contamination.3 Chorioamnionitis affects many pregnancies complicated by preterm prelabour rupture of membranes (PPROM).4 Intrauterine infection and inflammation are mostly associated with preterm labor and delivery, and at least 40% (positive amniotic fluid and chorioamniotic space culture) of preterm births have been estimated to occur with mothers who have an intrauterine infection, which is subclinical.5 The lower the gestational age at delivery, the greater the frequency of infections. As the clinical signs of chorioamnionitis like uterine tenderness, fever, fowl smelling vaginal discharge, maternal and fetal tachycardia is late to appear, CRP being the marker for inflammation, could be used as a non-invasive test to detect early chorioamnionitis, hence avoiding several complications associated with invasive test. In preterm patient who are being evaluated for the tocolysis or corticosteroids, laboratory assessment is of great value.6,7 OBJECTIVE: To determine the diagnostic accuracy of CRP in the association of chorioamnionitis following PPROM. Study maternal and fetal outcome.
MATERIALS AND METHODS This study was conducted at Government Lady Goshen Hospital and KMC Attavar Mangalore associated with Kasturba Medical College, Mangalore. The study was a time bound observational study done over the period of September2018 to August 2020. With the anticipated incidence of 5-10% (Lenihan et al.) the sample size was taken to 100 pregnant women with period of gestation between 28 weeks to 36weeks + 6 days. Patient with conditions such as preeclampsia, Antepartum haemorrhage, Polyhydramnios, Uterine anomalies, Chronic hypertension, Diabetes, Hepatitis, SLE, Rheumatoid Arthritis, Rheumatic fever, Viral Infection were excluded. A detailed history was taken, general, systemic and local examination was done and signs of chorioamnionitis were noted and documented in Proforma. Blood is withdrawn at the time of admission, routine investigations with CRP for all patient with PPROM sent and collected, and patient’s antepartum and intrapartum events observed. Patient was managed as per hospital protocol. For CRP estimation 2ml blood is withdrawn and collected in red vacutainer. CRP levels are estimated by immunoturbidimetric method that gives a quick result. The normal level of CRP is 6-8mg/dl. After delivery, placental membranes were cut into 1-2mm pieces and placed in 10% formalin is sent to pathology department for HPE and HCA was identified as intracytoplasmic neutrophilic infiltration at two or more sites in the chorionic plates, using a standardized protocol. Placental membranes in normal saline were also sent for culture sensitivity to watch for any growth of organism. The study participants were observed while they were in hospital. The mother was looked for the signs of abdominal pain, fever, foul smelling vaginal discharge, hemorrhage, wound discharge, post- partum hemorrhage, sepsis and length of hospital stay. Neonates were observed in NICU. The symptoms sought for included excessive crying, poor sucking effort, neonatal jaundice, discharge from eyes or umbilicus. Collected data will be coded and entered. Statistical package for social science (SPSS) 11.5. For comparison of values student t- test would be used. P value <0.005 will be considered as statistically significant.
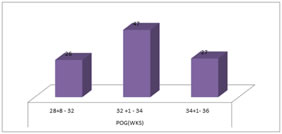
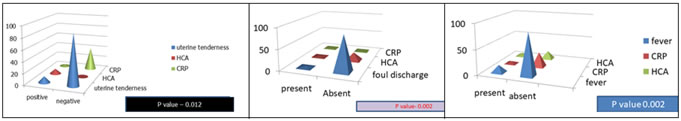
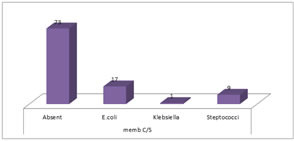
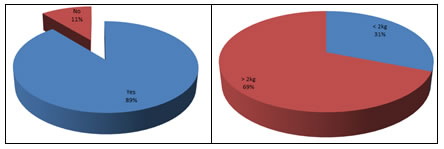
RESULTS In the present study Out of 121 subjects selected, 10 subjects had Gestational HTN, 4 subjects had Polyhydramnios and 3 subjects had malpresentation and were excluded from the study. Hence A total of 100 pregnant women were included in the study in accordance with the inclusion criteria in a time bound study. The maternal and foetal outcome were observed. The Period of Gestation when the PPROM is noted commonly is between 32–34-week POG making up to 47% of the study population and was found to be statistically insignificant (graph 1). Of the total study participant, the case of HCA is noted to be higher when the time interval between the onset of PPROM and the delivery of the baby is more than 24 hrs. and is found to be statistically significant. The relation with of CRP with lag of time is found to be statistically insignificant, as the patient having HCA on HPE were found to have negative CRP values (table 1). Out of the total 100 study participant, uterine tenderness was found in 11% of the cases and was not statistically significant for the development of HCA. The CRP levels were found to be low, hence implying that the levels of CRP were not statistically significant for the diagnosis of HCA (graph 2). Out of the total 100 study cases, 4 cases had foul smelling vaginal discharge, and all 4 cases were found to have HCA, which is found to be statistically significant. Meanwhile the value of CRP was not found to be statistically significant (graph 3). Out of the total 100 cases, maternal pyrexia was found in 15% of the cases and of those 15% cases HCA was found to be positive in 46% of cases which was found to be statistically significant. Although, the CRP levels were found to be raised in only 5% of cases, which was found to be statistically insignificant (graph 4). Out of the total study population, 48% of the cases had the total counts of more than 16700, and there was no significant association noted between elevated total counts and HCA (table 2). In our study out of 100 cases, 56% cases were CRP positive, out of which only 4 HCA positive cases had a CRP level cutoff of 40 mg/dl (table 3). 11% was found to have HCA on histopathological examination, out of which only 4 cases were CRP positive and hence there was no statistically significant correlation between CRP levels and HCA (table 4). In the study 27% cases were membrane culture positive with no significant correlation to HCA. The most common organism isolated from the placental membrane was E. coli and 2ndcommon being Streptococci. E. coli was the most common organism isolate from the placental membrane culture sensitivity in patient having pyuria (table 5, graph 5). In this study, the PPROM was most seen in-patient showing bacteria positive in URE (table 6). 56% cases underwent C-section and 44% of cases were delivered vaginally. Out of 56% cases which was C-section, 12% of the cases had HCA and 30% were CRP positive which was not found to be statistically significant (table 7). The patient undergoing caesarean delivery because of CRP positive status were 56% and the number of patients who had HCA were 6, which was found to be insignificant. The rate of caesarean delivery was found to be increased in our study (table 8). The study reveals a positive correlation with P value of 0.002 between HCA positive cases and post-partum hemorrhage (PPH). While the pelvic abscess, wound infection and maternal sepsis remains insignificant outcome (table 9). 89% babies were admitted in NICU for preterm care and monitoring (graph 6). The mean POG observed in our study was between 32-34 weeks, and the neonatal birth weight were in correlation to the POG i.e., 69% of the neonates had birth weight above 2 kegs. However, there was no evidence to show a positive association between HCA and birth weight. The neonates born > 2kgs had a better survival rate and less of neonatal complication (graph 7). In this study, out of 89% NICU admission, Necrotizing Enterocolitis and Early onset sepsis was found to be statistically significant in PPROM delivered babies. The neonates delivered to HCA positive mother was found to be more at risk of developing Early onset sepsis. A total of 11 neonates developed Necrotizing enterocolitis and 23 neonates developed Early onset neonatal sepsis (table 10).
Graph 1: gestational age at the time of PPROM
Table 1: Time interval between PPROM and delivery of the baby
Graph 2 Graph 3 Graph 4 Graph 2: Uterine tenderness and its relation to HCA Graph 3: Foul smelling discharge and its relation to HCA Graph 4: Maternal Pyrexia and its relation with HCA. Table 2: Total counts and its relation to HCA
Table 3: CRP positive cases.
P value: 0.016 (Significant) Table 4: CRP levels and its relation to HCA
Table 5: Placental membrane culture and sensitivity.
Graph 5: Growth on membrane culture sensitivity.
Table 6: Urine examination and relations with HCA
Table 7: Mode of delivery
Table 8: Indication for caesarean delivery in PPROM cases
P value- 0.098
Table 9: Maternal outcome
Graph 6: NICU admission Graph 7: Birth Weight
Table 10: Neonatal outcome
DISCUSSION The overall incidence of the Histopathological Chorioamnionitis is this study is found to be 11% and was not significantly related to CRP positive status, which is comparable to the study done by Martinez and colleagues (2007),8 Rebecca et al. (2012),9 Angela Koech Etyang and colleagues (2020),10 although had a contrasting results with the study done by Su Ah Kim, et al.11 Sung Youn Lee et al. (2011),12 Naskar et al. (2019).13The Period of Gestation where the maximum PPROM was noted in our study was between 32-34 weeks POG, which was comparable to Kayam et al.14, Asadi, et al.15 Park et al.16. Although Farb et al.17 showed a contrasting results, which showed lower the gestational age higher is the chances for chorioamnionitis, which also could be due to small sample size.The POG was not significantly related to HCA or CRP levels in our study. The time noted from the onset of PPROM, and delivery is crucial to the neonatal outcome as well as maternal outcome. This study has found a positive correlation between the duration of PPROM and risk of developing HCA, the longer the duration of PPROM more the risk of HCA. Cases delivering after 24 hrs.was significantly related to the development of HCA which was comparable to the study done by Gopalani, et al.18 Miyazaki. et al.19 The invasion of the decidua by microbes and its migration to fetus increases leads to poor neonatal outcome. Uterine tenderness as a clinical sign for HCA is not statistically significant in relation to development of HCA. Uterine tenderness can also be masked by the effect of epidural analgesia, if used, hence making it not a very reliable sign for suspecting HCA. The results obtained in this study is comparable to the study done by Alan and colleague.20 Curtin. et al.21 Foul smelling discharge is listed as the clinical sign for suspecting Chorioamnionitis. In this study, the foul-smelling discharge is found to be statistically insignificant in relation to developing HCA, which is comparable to the study done by Alan T and colleague20 and Gulin. et al.22 The foul discharge of vaginal fluid may be missed clinically and hence should be very carefully assessed. The “Maternal Pyrexia is the most important clinical sign of Chorioamnionitis”. The temperature cut-off noted in our study was 38 degrees Celsius, which was comparable to the study done by Drucilla, et al.23 Curtin, et al.21 and was statistically significant and was the clinical sign associated with the HCA. While it had no positive correlation with CRP levels. Of all the clinical signs to detect chorioamnionitis, maternal pyrexia is found to be most reliable. CRP being the nonspecific marker of inflammation is widely used in deciding the management of the PPROM cases, has found to be statistically insignificant for suspecting HCA, which is comparable to the study done by Gulin, et al.22 Park, et al.16 Kim, et al.24 Angela and colleague,10 Su Ah Kim. et al.11 CRP is found to be inadequate in the diagnosis of HCA. CRP has been used traditionally to guide the management of cases of PPROM, this study has put forward the need to use other marker for the management of PPROM. In the present study11% of the cases were HCA positive with no correlation to CRP levels significantly. The definitive diagnosis of HCA is always established by histopathological examination, which remains the gold standard. Our study is comparable to Jeong and colleague25 which proves that CRP played no role in the diagnosis of HCA and only HPE is the diagnostic tool for establishing the diagnosis of HCA. In our study, adverse maternal outcome was noted in terms of PPH seen in patient with HCA positive status which was found to be statistically significant and comparable to the study done by Ovalle and colleagues.27 Ocheke et al.26 showed contrasting results and showed no association between the maternal outcome and HCA positive status, which can be due to the small sample size of the study. The NICU admission is our study was 89%, of which 11% of the neonate had necrotising enterocolitis and 23% of the neonates had early onset sepsis. While 60% neonates had developed respiratory distress, there was no correlation found with the HCA positive status. 8% of the neonates had developed IVH which was found to be insignificant. In our study the risk of Necrotising Enterocolitis and Early onset sepsis was found be to significant with P value of 0.001 for both, which was comparable to the study done by Liran, et al.28 Matsuda, et al.29 Kenyon et al.30 while other study showed contrasting results like keuchkerian, et al.31 The birth weight of the neonate had no correlation to the HCA in our study which is comparable to the study done by Ocheke, et al.26 whereas a study done by Cutin and co-workers21 has a contrasting finding, where babies born to HCA positive mother weighted significantly less than those born to HCA negative mother.
LIMITATION The sample size of the study was relatively small. The other inflammatory markers and amniotic fluid was not studied.
CONCLUSION Histopathological chorioamnionitis does not correlates to the CRP values in this study. In this study, maternal pyrexia and foul-smelling vaginal discharge is found to be a more specific clinical sign. The rate of caesarean section was increased, considering the CRP positive status.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home