|
Table of Content - Volume 21 Issue 1 - January 2022
The role of doppler study in evaluation of pregnancy induced hypertension (PIH) and intrauterine growth restriction (IUGR) in primigravida
Amod Mahajani1, Bhagyashree Badade2*
1Associate Professor, 2Junior Resident, Department of Obstetrics and Gynecology, ACPM Medical College, Dhule, Maharashtra, INDIA. Email: aam_111@yahoo.com
Abstract Background: Pregnancy induced hypertension (PIH) is the most significant and intriguing unsolved problem in obstetrics which remains as a great challenge to obstetricians particularly in developing countries. It denotes an underlying pathology that may be pre-existing or develop for the first-time during pregnancy. Aims And Objective: To screen and predict the development of Pregnancy induced hypertension (PIH) and intrauterine growth restriction (IUGR) using Doppler study in Primigravida patients. To evaluate usefulness of uterine, umbilical, middle cerebral artery Doppler screening in second and third trimester to predict the risk for PIH and IUGR. To correlate the finding of Doppler study with maternal and fetal outcome. Method: This Prospective observational study was carried out in the Department of Obstetrics and Gynaecology at our institution from December 2018 to October 2020 for a period of 1 year after obtaining approval from the Institutional Ethical Committee and getting informed and written consent from all the participants in a language best understood by them. In our study a total of 100 Primigravida patients between 18 to 35 years of age, attending antenatal outpatient department, were screened at 18 to 22 weeks of gestation with USG along with Doppler study. Result: Among 100 patients in our study group; 21 patients (21%) delivered preterm before 37 weeks of gestation, 7 out of 100 mothers (7%) in our study group developed pre-eclampsia and 8 mothers (8%) developed gestational hypertension. A total of 15 mothers (15%) developed pregnancy induced hypertension (PIH) at some point of time in their pregnancy. Pregnant mothers in our study group delivered 16 IUGR babies (16%), while 22 neonates (22%) delivered had their 1minute APGAR Score <7. 22 babies (22%) required NICU admission due to various reasons like fetal distress, low birth weight, prematurity etc. In our study, cesarean section (elective as well as emergency cesarean section) was done in 25 patients (25%) which included 17 patients with abnormal Doppler indices as well. Conclusion: Elevated uterine artery PI and presence of diastolic notch appears to be more significantly superior to other parameters in prediction of Preeclampsia. Umbilical artery Doppler findings are better predictor of perinatal outcome than abnormal MCA in early weeks of gestation whereas MCA PI Doppler is more useful than Umbilical PI or uterine artery in predicting the adverse perinatal outcome in later weeks. Keywords: Uterine Artery Doppler, Umbilical Artery Doppler, Middle Cerebral Artery Doppler, Pregnancy induced hypertension, Intrauterine growth restriction, Maternal Outcome, Neonatal Outcome
INTRODUCTION Every new born has the right to be born undamaged mentally and physically. The fulfilment of this goal plays an important role in materno-fetal medicine, whose sole objective is to culminate every pregnancy into a safe outcome both for the mother and the baby.1 Most pregnancies, labors and deliveries are normal biological processes that result in the healthy outcome for both, however those that are not normal can result in maternal and/or perinatal morbidity or substantial mortality.2 The main goal of antenatal care is to detect those pregnancies that are at risk for complications and manage them well in time.3 Pregnancy induced hypertension (PIH) is the most significant and intriguing unsolved problem in obstetrics which remains as a great challenge to obstetricians particularly in developing countries.4 It denotes an underlying pathology that may be pre-existing or develop for the first time during pregnancy. In developing countries, they rank second only to anemia complicating approximately 7 to 15 percent of all pregnancies.5 It is the world’s second most common cause of maternal death.6 Pre-eclampsia (PE) is principally disease of first term pregnancy and is thought to develop from inadequate trophoblast invasion of the maternal spiral arteries.7 It is a common condition that limits the availability of substrates required for growth and development of the fetus, resulting in intrauterine growth restriction (IUGR) and manifesting as birth weight below 10th centiles of average for the gestational age.8 The trophoblast begins to invade the decidual portion of the spiral arteries by the eighth week and is normally completed by the thirteenth week. After that, the second stage of spiral artery invasion begins, in which the myometrial portion of the spiral arteries are invaded. This is usually completed by 18-19 weeks.9 A low resistance, low pressure vascular bed with a high blood flow system is developed in this process.10 Physiological changes during pregnancy transform the spiral arteries from small muscular arteries to distended, tortuous and funnel shaped uteroplacental vessels, allowing them to accommodate the hemodynamic forces of pregnancy.11 In the overwhelming majority of pre-eclamptics, this transformation does not occur in the spiral artery bed due to failure of second wave of endovascular trophoblast migration and leading to increased resistance to the flow into the intervillous space resulting in decreased blood supply to feto-placental unit.9 A low resistance, low pressure vascular bed with a high blood flow system is developed in this process.10 Physiological changes during pregnancy transform the spiral arteries from small muscular arteries to distended, tortuous and funnel shaped uteroplacental vessels, allowing them to accommodate the hemodynamic forces of pregnancy.11 In the initial stages, there is sparing of brain growth at the expense of compromise in fetal length. But if the insult continues, brain growth is also compromised. Initially Umbilical Artery (UA) Systolic-Diastolic (S/D) ratio increases and Middle Cerebral Artery (MCA) Systolic-Diastolic (S/D) decreases indicating placental resistance which is followed by reduced Middle Cerebral Artery (MCA) Systolic-Diastolic (S/D ) ratio than Umbilical Artery (UA) Systolic-Diastolic (S/D) ratio indicating centralization of flow. Finally, the Umbilical Artery (UA) Doppler shows absent and reversal of flow which is associated with adverse perinatal outcome.12 Direct assessment of trophoblastic invasion in human pregnancy is not possible, however with the introduction of Doppler ultrasound examination it became possible to assess the uteroplacental and feto-placental blood flow and the fetal blood circulation. The uteroplacental and feto-placental circulation gives information on the placental resistance whereas evaluating the fetal circulation could non-invasively assess the fetal response to hypoxia.13 This article titled “The role of Doppler study in evaluation of Pregnancy Induced Hypertension (PIH) and intrauterine growth restriction (IUGR) in Primigravida” helps to evaluate the usefulness of Uterine, Umbilical and Middle Cerebral Artery Doppler ultrasound, by documenting our experience in demonstrating their sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy (DA) in second and third trimester in Primigravida women. Aims and Objectives: Our primary aim to conduct this study is as follows: To screen and predict the development of Pregnancy induced hypertension (PIH) and intrauterine growth restriction (IUGR), using Doppler study in Primigravida patients. To evaluate usefulness of uterine, umbilical, middle cerebral artery Doppler screening in second and third trimester to predict the risk for PIH and IUGR. To correlate the finding of Doppler study with maternal and fetal outcome.
MATERIAL AND METHOD This Prospective observational study was carried out in the Department of Obstetrics and Gynaecology at our institution from December 2018 to October 2020 for a period of 1year after obtaining approval from the Institutional Ethical Committee and getting informed and written consent from all the participants in a language best understood by them. In our study a total of 100 Primigravida patients between 18 to 35 years of age, attending antenatal outpatient department, were screened at 18 to 22 weeks of gestation with USG along with Doppler study. Follow up Doppler studies were done after 30 weeks of gestation in the third trimester as per indicated to determine a favorable or worsening trend in Doppler indices. All the eligible candidates were included in the study depending on the following inclusion and exclusion criteria: Inclusion Criteria: All Primigravida coming to our OPD. All Primigravida with singleton pregnancy. Exclusion Criteria: Multiple gestations. Patients with history of medical disorders such as diabetes, hypertension, renal disease and cardiac disease. Unregistered Primigravida term gestation. All subjects with preterm labour and PROM. Congenital anomalies of uterus and fetus. Pregnant women of age less than 18 years and more than 35 years, or unknown last menstrual period. Intrauterine death at the time of first Doppler examination. Trophoblastic disease. The data was coded and entered into Microsoft Excel spreadsheet. Analysis was done using Statistical package for social sciences (SPSS) version 20 (IBM SPSS Statistics Inc., Chicago, Illinois, USA) Windows software program. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy was also calculated for all Doppler measurements. RESULT Table 1: Distribution of the patients in study according to age group
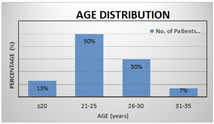
Table 1 showed the age distribution of 100 patients of my study group. All our patients’ age ranged from 18 years to 35 years. 13% were in the age group of ≤20 years, Majority of the patients (50%) were in the age group of 21-25 years, 30% were in the age group between 26-30 years, least number of patients (7%) were seen in the age group of 31-35 years. The mean maternal age was 24.68 years.
Graph 1: Distribution of the patients in study according to age group
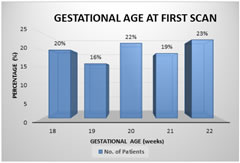
Table 2: Distribution of patients according to gestational age at 1st scan (18-22 weeks)
The study group included patients whose gestational age ranged from 18-22 weeks of gestation. Mean gestational age at the time of 1st scan was 20.10 weeks. Graph 2: Distribution of patients according to gestational age at 1st scan (18-22 weeks)
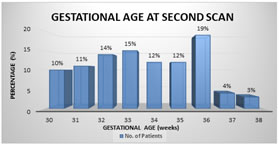
Table 3: Distribution of patients according to gestational age at 2nd scan (After 30 weeks)
The study group included patients whose gestational age ranged from 30-38 weeks of gestation. Mean gestational age at the time of 2st scan was 33.58 weeks.
Graph 3: Distribution of patients according to gestational age at 2nd scan (after 30 weeks)
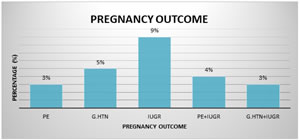
Table 4: Distribution of cases of pre-eclampsia (pe), gestational hypertension (gh) and intrauterine growth restriction (iugr) in study population
Of the 100 cases included in the study, 8 patients developed only PIH (3 PE + 5 GH); 9 patients had only IUGR and 7 patients were complicated by both PIH and IUGR. Incidence of PIH was 15% and IUGR was 16%
Graph 4: Distribution of cases of pre-eclampsia, gestational hypertension and intrauterine growth restriction in study population Table 5: Adverse pregnancy outcome in study population
Mean gestational age at time of delivery - 37.68 weeks. Preterm delivery – 21%. Term delivery – 79%. Minimum Birth weight - 1.40 kilograms. Maximum Birth weight -3.24 kilograms. Mean Birth weight at time of delivery - 2.7023 kilograms. Stay in NICU – 22%. Minimum stay in NICU – 3 days. Maximum stay in NICU – 14 days. IUGR – 16%
Table 6: Mode of delivery
Amongst 24 patients with abnormal Doppler: 7 patients delivered vaginally (29.17%). 17 patients underwent LSCS (70.83%) Amongst 76 patients with normal Doppler: 68 patients delivered vaginally (89.47%). 8 patients underwent LSCS (10.53%) In 100 patients: 75% had Vaginal delivery. 21% had Emergency LSCS. 4% had Elective LSCS
Table 7: Test performance values for uterine artery, umbilical artery and middle cerebral artery for PIH at 18-22 weeks
Table 8: Test performance values for uterine artery, umbilical artery and middle cerebral artery for IUGR at 18-22 weeks
Table 9: Test performance values for uterine artery, umbilical artery and middle cerebral artery for PIH after 30 weeks
Table 10: test performance values for uterine artery, umbilical artery and middle cerebral artery for IUGR after 30 weeks
DISCUSSION This study was primarily done to evaluate whether abnormal Doppler findings at 18 – 22 weeks and after 30 weeks of gestational period is useful in predicting the development of PIH and IUGR. In this study, 100 pregnant Primigravida women with singleton pregnancy attending our OPD between 18-22 weeks of gestation were selected. They were assessed with Doppler velocimetry, follow up of all the patients was done. The period between 18 -22 weeks was chosen to perform the Doppler because a routine anomaly scan was done regularly in all pregnant mothers during that period. Coming to age distribution of the patient, all our patients age ranged from 18 years to 35 years. Majority of the patients (50%) were in the age group of 21-25 years, 30% were in the age group between 26-30 years, 13% were in the age group of ≤20 years and least number of patients (7%) were seen in the age group of 31-35 years. The mean maternal age was 24.68 years. Before going in deep about Doppler findings let’s see prevalence of adverse outcomes in our study group. Among 100 patients in our study group; 21 patients (21%) delivered preterm before 37 weeks of gestation, 7 out of 100 mothers (7%) in our study group developed pre-eclampsia and 8 mothers (8%) developed gestational hypertension. A total of 15 mothers (15%) developed pregnancy induced hypertension (PIH) at some point of time in their pregnancy. Pregnant mothers in our study group delivered 16 IUGR babies (16%), while 22 neonates (22%) delivered had their 1minute APGAR Score <7. 22 babies (22%) required NICU admission due to various reasons like fetal distress, low birth weight, prematurity etc. In our study, cesarean section (elective as well as emergency cesarean section) was done in 25 patients (25%) which included 17 patients with abnormal Doppler indices as well. Dildy et al.14 have reported the rate of cesarean delivery in patients of hypertension in the range of 11-57%. UTERINE, UMBLICAL AND MIDDLE CEREBRAL ARTERY DOPPLER INDICES IN PIH AND IUGR: The Doppler findings in our study group was as follows. To start with evaluation of uterine artery. Among the 100 patients studied there were 21 patients with abnormal uterine artery Doppler when 95th percentile was taken as cut off. Among them 15 Patients had abnormal SD ratio, 13 patients had abnormal RI, 19 patients had abnormal PI and 21 patients had early diastolic notch during their first scan which was done between 18-22 weeks of gestation. On follow up scan, done after 30 weeks of gestation, there were 15 patients with abnormal uterine artery Doppler when 95th percentile was taken as cut off. Among them 10 Patients had abnormal SD ratio, 9 patients had abnormal RI, 15 patients had abnormal PI and 13 patients had persistence of diastolic notch. Coming to the evaluation of umbilical artery, there were 22 patients with abnormal umbilical artery Doppler when 95th percentile was taken as cut off. Among them 22 Patients had abnormal SD ratio, 19 patients had abnormal RI and 16 patients had abnormal PI during their first scan done between 18-22 weeks of gestation. On follow up scan, done after 30 weeks of gestation, there were 17 patients with abnormal umbilical artery Doppler when 95th percentile was taken as cut off. Among them 16 Patients had abnormal SD ratio, 17 patients had abnormal RI and 14 patients had abnormal PI. None of them had reversal or absent diastolic flow in the umbilical artery. In the middle cerebral artery, there were 14 patients with abnormal Doppler indices when 95th percentile was taken as cut off. Among them 14 Patients had abnormal SD ratio, 11 patients had abnormal RI and 12 patients had abnormal PI during their first scan done between 18-22 weeks of gestation. On follow up scan, done after 30 weeks of gestation, there were 21 patients with abnormal middle cerebral artery Doppler when 95th percentile was taken as cut off. Among them 18 Patients had abnormal SD ratio, 17 patients had abnormal RI and 21 patients had abnormal PI.
Table 11: comparison of study at our institution with previous studies on uterine artery doppler for prediction of PIH
Tis indicates that elevated uterine artery PI and presence of notch appears to be more significantly superior to other parameters in prediction of Preeclampsia. This is similar to opinions by Sieroszewski; et al.15 Barati M; et al.19 Saptarshi Chakraborty, et al.16 Jeltsje S Cnossen et al.17 and Samir hazra et al.4 where they concluded that an abnormal uterine artery Doppler result had an high specificity and negative predictive value for predicting preeclampsia. Table 12: comparison of study at our institution with previous studies on uterine artery doppler for prediction of IUGR
According to Ochi, et al.24 increased PI and the presence of diastolic notch in the uterine artery flow velocity, indicate increased uterine arterial resistance and impaired uterine circulation. The findings in the present study suggest that the increased Doppler indices in uterine artery with associated diastolic notch and persistence of diastolic notch after 30 weeks of gestation constitute an ominous sign and indicate the requirement for timely and intense fetal surveillance and intervention. The present study concludes that elevated uterine artery PI and presence of diastolic notch at early weeks of gestation appears to be a better predictor and more significant than uterine artery S/D in assessment of intrauterine fetal growth and in predicting perinatal outcome. Table 13: Comparison of study at our institution with previous studies on umbilical artery doppler for prediction of PIH
Table 14: Comparison of study at our institution with previous studies on umbilical artery doppler for prediction of IUGR
The present study concludes that Umbilical artery PI is relatively a more specific criterion than a sensitive criterion. In the present study, umbilical RI was also seen to have a good discriminant value but with relatively lower sensitivity as compared to PI. In different studies too umbilical artery RI has been reported to have low sensitivity and high specificity. A systematic review and bivariate meta-analysis has concluded that, in cases of IUGR, presence of abnormal fetal umbilical artery Doppler is the best predictor of adverse perinatal outcome. Table 15: Comparison of study at our institution with previous studies on middle cerebral artery doppler for prediction of IUGR
While studying the usefulness of MCA parameters, we observed an increasing trend of sensitivity for MCA PI and MCA RI with increasing gestational age. This outstanding performance of the middle cerebral artery PI and MCA RI in between 31-36 weeks of pregnancy is because changes of IUGR in the artery become prevalent in later weeks of pregnancy, as in earlier weeks there is brain sparing effect which protects the fetal brain from the profound effects of hypoxia. The MCA pulsatility index had a higher sensitivity and positive predictive value for predicting the adverse perinatal outcome than the Umbilical Artery pulsatility indices and uterine artery PI while using Doppler ultrasound results for interpretation. Our findings agree with the results of the studies that have shown MCA PI Doppler to be more useful than Umbilical PI or uterine artery in predicting the adverse outcome in later weeks whereas Umbilical artery Doppler findings are better predictor of perinatal outcome than abnormal MCA in early weeks of gestation. Hence we are of the opinion that, Doppler data containing both umbilical and cerebral velocimetry provide additional information on fetal consequences of the placental abnormality.
CONCLUSION After analyzing results of our study, we are of the conclusion that Pregnancy induced hypertension is associated with a higher rate of fetal morbidity and mortality. Doppler velocimetry can be used as routine check-up during follow up in high-risk pregnancies suspected of PIH and IUGR. Early recognition of women of PIH will help in identifying high risk women who may benefit from early prophylaxis and enhanced surveillance. Increased pulsatility index with notching in second trimester predicted overall preeclampsia in high risk and low risk patients. Diastolic notch in the uterine artery as a single parameter is better than the individual Doppler indices in uterine artery. Doppler patterns follow a longitudinal trend with early changes in the umbilical artery followed by middle cerebral artery. Combined uterine artery, umbilical artery and middle cerebral artery Doppler is the best predictor for PIH and IUGR. Doppler serves as an important yardstick for the obstetricians when dealing with pregnancies complicated with PIH and growth restriction. Uterine, umbilical and middle cerebral artery Doppler velocimetry may be included in hospitals with facilities and infra-structure to identify a group of patients at a risk of developing PIH or fetal growth restriction. It is safe, non-invasive technique, easy to perform, easy to interpret, and hence most valuable tool in the management of high-risk pregnancy. The limitation of our study is sample size, hence it would be better to do further studies by having a large sample and further modalities, and also combining all Doppler indices with other tests that are related to PIH and IUGR used in clinical care. This may improve the predictive accuracy and the clinical important value of the tests. The research for ideal predictive test and preventive measure still remains challenging.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home