|
Table of Content - Volume 21 Issue 2 - February 2022
A study on partogram in management of labor in patients with previous LSCS
Rupali Lalasaheb Ghatage1, Smita Krishnarao Bhat2*
1Junior Resident IIIrd Year, 2Professor, Department of Obstetrics and Gynaecology, Bharati Vidyapeeth (Deemed to Be University) Medical College and Hospital, Sangli, INDIA. Email: bhatsmita2@gmail.com
Abstract Background: Partogram is a very useful document to study the progression of labor. In patients who undergo trial of labor after cesarean section, partogram can help in intrapartum monitoring and identify any abnormal labor patterns. Thus it can ensure good feto-maternal outcome. Aim: To study the progress of labor in all ANCs with previous LSCS consenting for vaginal delivery using partogram and to note the feto-maternal outcome. Methods: A retrospective observational study was conducted for a duration of 6 months in 25 patients with previous LSCS for trial of labor who fulfilled the inclusion criteria. Detailed history regarding age, parity, duration of pregnancy and labour pain was taken from every patient. Examination was done including general physical examination, abdominal examination for fundal height, lie, presentation, engagement, amount of liquor, palpable uterine contraction and fetal heart rate. Pelvic examination was done for pelvic assessment and Bishop score. All the data were entered in a predesigned proforma. The course of labour in all the patients were recorded on WHO modified partograph. Statistical analysis was done using SPSS software. Result: Out of 25 patients, 10 (40%) delivered vaginally while 15 (60%) underwent repeat LSCS. 2 of 10 vaginal deliveries were instrumental deliveries. 3 patients (12%) crossed the action line, 13 (52%) were between action and alert line and 9 patients (36%) did not cross the alert line. From among 15 patients who had to be taken for CS, fetal distress was seen in 10 patients (66.66%), 2 patients (13.33%) had scar dehiscence and 3 patients (20%) were taken for CS due to non-progression of labor. APGAR score was less than 7 in 5 neonates and more than 7 in 20 neonates at 1 minute. While APGAR score was less than 7 in 3 neonates and more than 7 in 22 neonates at 5 minutes.
INTRODUCTION ‘A picture is worth a thousand words’. Partograph is a Latin/Greek hybrid word, synonymous with Parturition recorded in a graphic form. Partograph is a composite graphical record of key data (maternal and fetal) during labor, entered against time on a single sheet of paper.1 Partograph is a simple inexpensive predictive tool which is useful for analyzing progress of labor but is underutilized due to lack of knowledge.2 As part of the Safe Motherhood initiative, launched in 1987, the World Health Organization have produced and promoted a partograph with a view to improve labour management and reducing maternal and fetal morbidity and mortality. The programme described that WHO -modified partogram is an excellent tool in reducing obstructed labour and its consequences.1 Although the maternal mortality ratio (MMR) has dropped by approximately 45% in the last two decades, around 300,000 women continue to die each year globally due to avoidable pregnancy related complications. Obstructed labour is a leading cause of maternal and neonatal mortality, especially in developing countries.3 The present study was carried out for giving trial of labor using WHO recommended partograms to evaluate the effectivity of partogram in patients in labor with a previous LSCS and the predictability of the progress and outcome of labor.1 AIM: To study the progress of labor in all ANCs with previous LSCS consenting for vaginal delivery using partogram and to note the feto-maternal outcome. OBJECTIVES: To study the progress of labor using partogram. To identify abnormal labor patterns. To prevent prolonged labor and its complications. To study maternal and fetal outcome
MATERIAL AND METHODS MATERIAL: Patients with previous LSCS (previous LSCS due to non-recurrent indications like Breech, fetal compromise, abruptio placenta, cord prolapse etc.), adequate pelvis and cephalic presentation in whom the consultant decided to give normal trial of labor attending Bharati Vidyapeeth (Deemed to be) University Medical college and Hospital Sangli were selected for the study and explained pros and cons of vaginal birth after cesarean section (VBAC). Informed written consent was taken from all consenting patients. Patients with malpresentation, CPD, contracted pelvis, more than previous LSCS, Previous classical CS, previous CS due to prolonged labor or obstructed labor, previous inverted T incision, pregnancy occurring too soon after cesarean section, Pre-term labor, PPROM, placenta previa and Pre-eclampsia/ Eclampsia were excluded from the study. METHOD: A retrospective observational study was conducted for a duration of 6 months in 25 patients with previous LSCS for trial of labor who fulfilled the inclusion criteria. Detailed history regarding age, parity, duration of pregnancy and labour pain was taken from every patient. Examination was done including general physical examination, abdominal examination for fundal height, lie, presentation, engagement, amount of liquor, palpable uterine contraction and fetal heart rate. Pelvic examination was done for pelvic assessment and Bishop score. All the data were entered in a predesigned proforma. The course of labour in all the patients were recorded on WHO modified partograph. Individual partograph was studied to know the various aspects related to the course of labour and the role of partograph in influencing decision making in abnormal progress of labour was assessed.9 OBSERVATIONS Our study included a total of 25 patients with average age 24.04 years with minimum age of a patient being 19 years while the maximum age was 33 years. Table 1
In present study 21 out of 25 patients delivered at the gestational age of 37-40 weeks (84%). Out of these the patients who underwent repeat LSCS were 13 (52%) and those who delivered vaginally were 8 (32%). Table 2
Table 3
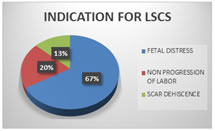
4 patients delivered at gestational age of more than 40 weeks (16%). Out of which 2 patients undergone LSCS (8%) and 2 delivered vaginally (8%). There was no statistically significant association between gestational age and mode of delivery. Out of 15 patients who undergone repeat LSCS, 2 patients had scar dehiscence (13.33%), 3 patients were taken for LSCS due to non-progression of labor (20%) and 10 patients had fetal distress (66.66%). Out of 10 patients who delivered vaginally, 2 underwent instrumental delivery (20%). Table 4
Figure 1
COMPLICATIONS Maternal complications: From among 10 vaginal deliveries, 1 patient had cervical tear and 1 had vaginal lacerations due to instrumental delivery. There was incidence of PPH in 2 cases. Neonatal complications: There were no neonatal complications like birth asphyxia or meconium aspiration.
DISCUSSION Ever since 1920 when lower segment transverse caesarean section came into favor, trials on vaginal delivery after a prior caesarean section have flooded the world’s obstetric literature convincing that vaginal delivery is the optimal mode of delivery in subsequent pregnancy unless contraindicated. In this study there were 25 patients selected for a trial of labour. Of these 25 patients 10 delivered vaginally yielding an overall incidence of 40% in patients with previous LSCS undergoing trial of labor. This result was quite similar to study done by Sharma R. K. No mentionable incidence of maternal morbidity was found to be in the study group. No maternal mortality took place in our study. PPH was seen in 2 cases (8%) whereas in the study done by Sowmya K. et al. there was incidence of PPH in 4% cases. No stillbirth or perinatal mortality took place in our study and there were no other neonatal complications whereas in a study done by Sowmya K. et al. there was 2% incidence of birth asphyxia and 2% incidence of meconium aspiration. In our study there was no case of scar rupture but there were 2 cases (8%) in whom scar dehiscence was diagnosed and hence they underwent repeat LSCS. In the study done by Sharma R. K. there was incidence of scar dehiscence in 1.2% cases.
CONCLUSION The partogram was able to reduce feto-maternal complications and help in early detection of deviation from normal labor thus guiding in timely intervention. The subjects who crossed alert line in partogram were taken for LSCS thus indicating higher efficacy of partogram. With the use of partogram maternal complications in patients with previous LSCS like obstructed labor, prolonged labor, scar dehiscence and scar rupture and other complications like PPH, cervical tears/vaginal lacerations etc. can be prevented. The neonatal morbidity increases as the labour curve moves to the right of the alert line and it is significantly increased as the labour curve crosses the action line. Thus the alert line on the partograph indicates a high risk for the fetus to develop respiratory distress. Use of partograph reduces the incidence of fresh still birth and perinatal mortality. Thus with a careful selection of cases for trial of labour in patients with previous LSCS it resulted in successful vaginal delivery. And with the better infrastructure and antenatal and postnatal care of these patients, the chances of maternal and perinatal morbidity and mortality can also be reduced successfully.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home