Official Journals By StatPerson Publication
|
Volume 10 Issue 2 - May 2019
Venous Doppler and 2D Echocardiography findings in pulmonary embolism cases
Rahul N Mastud1, Gurunath P Parale2*
1Assistant Professor, 2Associate Professor, Department of Medicine, Dr. Vaishampayan Memorial Government Medical College Opposite District and Sessions court, civil chowk, Solapur 413003, INDIA. Email: rahulmastud@gmail.com
Abstract Background: Pulmonary thromboembolic disease refers to the condition in which blood clot(s) (thrombus or multiple thrombi) migrate from the systemic circulation to the pulmonary vasculature. Amis and objective: To study the venous Doppler and 2D Echocardiography findings in pulmonary embolism cases. Material and Methods: In the present observational study patients with age 21 years and above with CT pulmonary angiography showing evidence of pulmonary embolism were enrolled in the study. Total 50 cases were selected in the two years of study duration. Results: Lobar and segmental location of thrombus (90%) was most common finding on CT Pulmonary angiography and was followed by thrombus at Right branch of main pulmonary artery (24%) and Main pulmonary artery (12%). 48% patients had a normal chest X ray while cardiomegaly on chest X ray (26%) was the second most common finding. Sinus tachycardia (88%) was the most common ECG abnormality followed by T wave inversion in V1 – V3 (72%). Tricuspid regurgitation (90%) was most common finding on 2D Echocardiography followed by RA and RV dilatation (84%) was reported. Severe and moderate pulmonary hypertension was diagnosed in 50% and 34% cases respectively. 44% cases showed normal venous Doppler. Left lower limb DVT was reported in 26% cases while right lower limb DVT was reported in 24% cases. Conclusion: In the end we conclude that sinus tachycardia followed by T wave inversion in V1 – V3 were the most common ECG abnormality. Tricuspid regurgitation followed by RA and RV dilatation were the most common finding on 2D Echocardiography. While abnormal Doppler findings were observed in 56% cases where Left lower limb DVT and right lower limb DVT was common diagnosis. Key Word: Pulmonary embolism, Venous Doppler, 2D Echocardiography
INTRODUCTION Pulmonary thromboembolic disease refers to the condition in which blood clot(s) (thrombus or multiple thrombi) migrate from the systemic circulation to the pulmonary vasculature. Most of these blood clots arise from the “deep veins” of the lower and upper extremities (deep venous thrombosis, DVT). From the clinical standpoint, DVT and pulmonary embolism can be considered a continuum of the same disease, and the two terms are often collectively referred to as venous thromboembolism (VTE). This is distinct from cases of in situ thrombus formation in the pulmonary vascular tree, which is often part of a more complex condition such as idiopathic pulmonary arterial hypertension (primary pulmonary hypertension).Whereas in situ thrombus formation is a slow process, with typically subtle onset and progressive symptoms over a period of weeks to months, thrombus migration often results in dramatic and acute clinical changes. In some cases, unresolved pulmonary emboli can lead to a condition called chronic thromboembolism, with associated secondary pulmonary hypertension (chronic thromboembolic pulmonary hypertension).Pulmonary embolism has earned the reputation of a silent killer because less than half of patients who die of pulmonary embolism are diagnosed with the problem prior to death.1 Long term effects of nonfatal VTE lower the quality of life. Chronic thromboembolic pulmonary hypertension and postphlebitic syndrome are especially debiliting conditions and amount to long term morbidity. Various diagnostic modalities has been advised to diagnosed PE, such as chest X- ray, Plasma D-dimer assay, Electrocardiography, Ultrasonography, MRI, CT phlebography, Chest computed tomography, Magnetic resonance imaging and Ventilation perfusion lung scan. The present study was conducted with the aim to study the Venous Doppler and 2D Echocardiography findings in pulmonary embolism cases.
MATERIAL AND METHODS The present observational study was conducted with the aim to study the clinical profile and risk factors of CT pulmonary angiographically confirmed cases of pulmonary embolism. Patients with age 21 years and above with CT pulmonary angiography showing evidence of pulmonary embolism were enrolled in the study. Total 50 cases were selected in the two years of study duration. A detailed history of each patient was taken. Presenting symptoms were enquired in their chronological order of appearance, onset, and progression. Significant past medical history was noted in details. Family history, drug history and personal history were noted. History was followed by a detailed clinical examination of all the patients. General examination was done with special emphasis on Level of consciousness, Pulse, Blood pressure, Respiratory rate, Pallor, Cyanosis, Clubbing, Icterus, Jugular venous pressure, Edema and Body mass index. Detailed systemic examination was done in all patients. All the patients in the study were subjected to the following investigations Complete hemogram, blood sugar level, serum electrolytes, lipid profile, renal function tests, liver function tests, arterial blood gas analysis (ABG), electrocardiography (ECG), 2 D echocardiography with Doppler, chest X Ray, venous Doppler of lower limbs, CT pulmonary angiography.
RESULTS Table 1: Distribution according to Age and sex of patients with pulmonary embolism
Out of fifty patients 07 (14%) were of age group 21 to 30 years. 10 (20%) were in 31- 40 years age group, 13 patients (26%) were in 41 – 50 years age group, 07 patients (14%) were in 51 – 60 years age group, 09 patients (18%) were in 61 -70 years age group, 04 patients (08%) were in 71 – 80 years age group.
Table 2: Distribution according to location of thrombus on CT Pulmonary Angiography and Chest X ray findings
It was observed that lobar and segmental location of thrombus (90%) was most common finding on CT Pulmonary angiography and was followed by thrombus at Right branch of main pulmonary artery (24%) and Main pulmonary artery (12%) In present study 48% patients had a normal chest X ray while cardiomegaly on chest X ray (26%) was the second most common finding. Table 3: Distribution according to Electrocardiographic changes
In present study sinus tachycardia (88%) was the most common ECG abnormality followed by T wave inversion in V1 – V3 (72%).
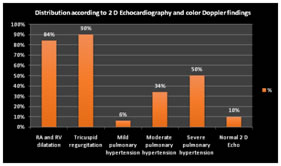
Table 4: Distribution according to 2 D Echocardiography
It was observed that tricuspid regurgitation (90%) was most common finding on 2D Echocardiography followed by RA and RV dilatation (84%) was reported. Severe and moderate pulmonary hypertension was diagnosed in 50% and 34% cases respectively.
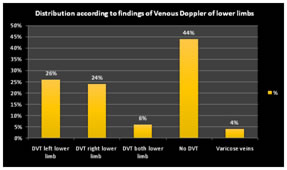
Table 5: Distribution according to findings of Venous Doppler of lower limbs
In the present study 44% cases showed normal venous Doppler. Left lower limb DVT was reported in 26% cases while right lower limb DVT was reported in 24% cases. DISCUSSION The present study was conducted to study the Venous Doppler and 2D Echocardiography findings in pulmonary embolism cases reported in tertiary care institute. Pulmonary embolism was observed in all age groups with a tendency to increased occurrence after the age of forty years. The mean age observed in thepresent study was 48 years which was lower than those reported by ICOPER2 (62.3 years), MAPPET3 (63.5 years) and JASPER4(60 years) in their studies. Most studies show a tendency towards even distribution by gender. In our study we observed a higher prevalence of the male gender (66%), which was also reported in the MAPPET3study (59%). It was observed that lobar and segmental location of thrombus (90%) was most common finding on CT Pulmonary angiography and was followed by thrombus at Right branch of main pulmonary artery (24%) and Main pulmonary artery (12%) In the present study we found cardiomegaly as one of the more common findings on chest X-ray observed in 26% of our patients whereas prominent central pulmonary artery was observed in 12%of our patients. In present study we found chest radiographic changes in 52% of patients. The ICOPER2analyzed chest X-rays of 2322 patients and found abnormal in 78% of patients. The ICOPER2 showed that pleural effusion was present in 23%, and areas of pulmonary infiltrates in 17%. Our findings identified pleural effusion in 14%, and pulmonary infiltrates in 14% of patients. Given the possibility of inter-observer variability and subjective analysis of changes, difference between the observations is acceptable. With the increasing accuracy of the different tools called on to diagnose PE (echocardiography, ventilation-perfusion scan, pulmonary angiography), the use of, and the interest in, the ECG as a diagnostic tool for PE has declined in most centers. In the present study out of 50 patients with PE hospitalized in a cardiology unit, the ECG changes were present in 92% of cases. This marked prevalence of ECG changes should be attributed to the fact that the patients were admitted in a cardiology unit that habitually receives cases of submassive and massive PE. Sinus tachycardia was the most prevalent (88%) ECG abnormality in the present study and was comparable to study by Lenegre et al5 who reported a prevalence of 90%. T wave inversion in V1 to V3 (anterior subepicardial ischemic pattern) was the next most common abnormality observed in 72% patientswhich was in agreement with a study by Ferrari et al6 who report a prevalence of 68% in their study and Lenegre et al5 who report a prevalence of 89%. Echocardiography may serve a valuable role in the diagnostic approach to pulmonary embolism. Under appropriate clinical circumstances, the detection of unexplained right ventricular volume or pressure overload should suggest the possibility of embolism and lead to confirmatory testing. Tricuspid regurgitation was the most common finding observed in 90% patients in the present study. The percentage of patients with RV dysfunction on echocardiography was 84%, which is higher than results found in the study by Ribeiro et al7 who reported it to be 70%. Severe pulmonary hypertension (SPAP >60 mm of Hg) was found in 50% of patients. 2 D Echocardiography was normal in 10% of our patients corroborating the fact that normal 2 D Echo does not exclude the diagnosis of pulmonary embolism. A distinct echocardiographic pattern involving akinesia of the mid-free right ventricular wall with apical sparing has been described8 (Mc Connells sign). The overall sensitivity of transthoracic echocardiography in pulmonary embolism approximates 50%.9 There fore, it cannot be considered a primary diagnostic technique. Consideration can be given to its use in the subset of patients with suspected massive pulmonary embolism who are too ill for transportation or who have an absolute contraindication to the administration of a contrast agent for CT pulmonary angiography. More recently, echocardiography has been investigated along with other techniques as a means of stratifying risk in patients with embolism. Transthoracic echocardiography and biochemical markers such as serum troponin or serum brain natriuretic hormone levels have been investigated as a means of evaluating right ventricular function in patients with embolism.10,11,12 Duplex ultrasonography, which refers to the combination of Doppler venous flow detection and real-time B-mode imaging, has assumed a central role in the noninvasive diagnosis of symptomatic lower extremity deep venous thrombosis.13 A number of criteria are used to diagnose venous thrombosis, the most reliable of which is non-compressibility of a venous segment. Other, less reliable criteria include the presence of echogenic material within the venous lumen, venous distention, and loss of phasicity, response to Valsalva's maneuver, and augmentation of spontaneous flow. The absence of an echogenic luminal mass cannot be considered useful in excluding the diagnosis of venous thrombosis because acute thrombus may not demonstrate echogenicity. Since the origin of the thrombus is mostly from deep veins of the legs, compression ultrasound of lower limb veins is a useful investigation in the diagnosis of PE. It is, however, reported to be positive only in 10-20% of patients without leg symptoms or signs who undergo evaluation and in approximately 50% of patients with proven PE14. Thus, PE cannot be ruled out on the basis of negative results on ultrasound. Compression ultrasound has its value in situations where there is a high clinical probability of PE and the patient has no past history of VTE14. In the present study, 56% of patients had an ultrasonographic evidence of DVT. And 6% of our patients had evidence of bilateral DVT. Which was comparable to the study by Agrawal et al15 who reported DVT in 66% of patients in their study. Thus, compression ultrasound is a useful investigation in patients with symptomatic PE.
CONCLUSION In the end we conclude that sinus tachycardia followed by T wave inversion in V1 – V3 were the most common ECG abnormality. Tricuspid regurgitation followed by RA and RV dilatation were the most common finding on 2D Echocardiography. While abnormal Doppler findings were observed in 56% cases where Left lower limb DVT and right lower limb DVT was common diagnosis.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home