|
Table of Content - Volume 20 Issue 3 - December 2021
Lichen planus- through a dermoscope
Atul Giri1*, Somshukla Ray2, Chitra Nayak3
1,2,3Department of Dermatology, IInd Floor, OPD Building, TNMC and BYL Nair Hospital, Mumbai, Maharashtra-400008, INDIA. Email: atulg100@gmail.com
Abstract Background: Lichen planus (LP) is an inflammatory dermatosis of skin and mucous membranes1 that has a variety of clinical manifestations. Dermatoscope is being increasingly used in dermatologic practice to study different skin conditions. However, knowledge of dermoscopic appearance of lichen planus is limited. Aims: To study the dermoscopic features of Lichen planus and its evolution. Methods: Fifty patients of active (acute and subacute) lichen planus were enrolled in the study. Biopsy was performed to confirm the diagnosis. Dermatoscopy was performed on each lesion before biopsy. Results: Wickham Striae (WS) was the most prominent feature noted in the lesions. The different patterns recognized were: - arboriform, reticular, globular, linear and annular with thin or broad spiky/comb like projections at the border. Different patterns of vasculature and pigment deposits were also studied. Conclusion: Dermoscopy is an effective and essential tool for diagnosing Lichen planus. It improves the recognition of pathognomonic feature- the Wickham striae which is often difficult to discern with naked eye. It also helps assessment of the disease activity and thereby the need for aggressive management, if any. Key Words: Lichen planus, Dermoscopy, Wickham’s striae.
INTRODUCTION Lichen planus (LP) is an inflammatory dermatosis of skin and mucous membranes1 with a variety of clinical manifestations. Dermatoscope, also known as epiluminence microscope, is being increasingly used to study different skin conditions. However, knowledge of dermoscopic appearance of lichen planus is lacking. Therefore, a detailed study may provide clues to the clinical behavior of this chronic condition.
METHODS Dermoscopic features of 50 patients of active (acute and subacute) lichen planus were studied. There were 23 males and 27 females in the study of age ranging from 4- 66 years. Seven of them were less than 20 years of age. Patients were selected consecutively as they presented to the hospital after obtaining informed consent. In case of children, parents/ guardians consent was obtained. Biopsy was performed to confirm diagnosis. A Canon Powershot A640 with an attachment was used with liquid paraffin as the linkage fluid for dermoscopy. The algorithm for dermoscopic diagnosis of non-pigmented disorders 1 – as suggested by Zalaudek et al. was followed. The different dermoscopic features observed were tabulated and analyzed.
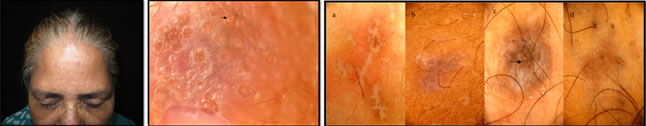
RESULTS Wickham’s striae (WS) was the most prominent feature (100%) noted in the initial papules and plaques (Figure 1, 2) of lichen planus (Table 1). The different patterns of Wickham’s striae recognized were: - reticular (Figure 1b, 3), globular (Figure 1b, 2b), linear (Figure 4), arboriform (Figure 4, 5) and annular with thin or broad spiky/comb like projections at the border (Figure 6). Some of the plaques also had central yellow-brown areas (Figure 1b, 4). Eighty four percent of the lesions showed an increased vascularity appearing as red globules (Figure 3) - 16 lesions (32%), diffuse erythema in 10 plaques, red dots- 10 lesions and red lines- 7 lesions (Figure 2b , 6). Some lesions had a combination of these features. Granular (Figure 3) and blotchy (Figure 1b, 4) pigmentation was observed in 36 patients (72%) along the borders of WS and also at the centre in mature LP lesions. Blotchy melanin deposits can be seen at areas where Wickham’s striae are slowly fading. Comedo like openings (9 lesions) and corn pearls (7 plaques) were observed in comparatively larger and long standing lesions (Figure 7, 8). Evolution of lichen planus can also be studied with a dermoscope. Early LP lesions (pink papules) show emergent Wickham Striae with background erythema (Figure 8a). In mature LP lesions (violaceous plaques - Figure 8b) WS become confluent in reticular networks and the central bluish- black pigment granules appear. In long-standing lesions (Figure 8c) WS appear to regress leaving behind dark blotchy pigment deposits with reduced vascularity. Comedo like openings can also be appreciated in older lesions. Fully subsided lichen planus shows irregular black slowly fading melanin granules (Figure 8d).
Table 1: Major Dermoscopic Features Of Lichen Planus (50 patients)
Figure 1a Figure 1b Figure 2a Figure 2b Figure 3 Figure 4 Figure 5 Figure 6 Figure 7a Figure 7b Figure 8a Figure 8b Figure 8c Figure 8d Figure 1a: Tiny erythematous papules and violaceous plaques on upper chest of a 33 year old female with eruptive lichen planus; Figure 1b: Dermoscopy showed reticular Wickham’s Striae with broad ramifications and comb like peripheral projections with central yellow-brown areas; bluish black granules of melanin are more prominent within the lesion than periphery. Also, adjacent lesion has globular Wickham’s striae; Figure 2a: A case of widespread lichen planus in a 22 year old female; Figure 2b: New lesions on leg was examined with a dermoscope which revealed globular pearly white WS with peripheral comb like projections intermingled with linear tortuous hairpin blood vessels at the periphery and very faint central erythema; Figure 3: A background of diffuse erythema with reticular Wickham’s Striae. Irregular granular pigmentation (broken arrow) and red globules (five point star) are seen bordering WS in the upper part whereas tiny red dots are visible along with faint white lines at the lower part of the lesion (arrow); Figure 4: Another lesion showing linear and arboriform WS with blotchy pigmentation; Figure 5: Arboriform WS in an early papule showing pigment granules along the margin; Figure 6: Annular WS, comb-like radial extensions at the periphery intermingled with capillaries; Figure 7a: Solitary papule of lichen planus on the forehead of a 55 year old lady. Figure 7b: dermoscopy shows multiple comedo like openings with developing corn pearls(); Figure 8: Evolution of Lichen Planus: Comedo like openings appear in later stages (8c, 8d) DISCUSSION Dermatoscope has been widely used to study pigmented lesions like melanoma but studies on non- pigmented benign conditions like lichen planus are limited. In 2006 Zalaudek et al.1 had suggested the following algorithm for diagnosis of non pigmented skin disorders. Step 1: Evaluation of lesion number: LP lesions are usually multiple. Step 2: Evaluation of vascular morphology: red globules (round dilated red structures), red lines (linear fine red structures) and red dots (punctate red structures) were observed. Step 3: Evaluation of architectural pattern of vessels, eg. a radial arrangement was noted in early lesions. Step 4: Evaluation of additional dermoscopic criteria (non-vascular features). In case of lichen planus they are2: - Wickham’s Striae (WS) and its patterns Central yellow-brown areas. The pattern of pigment deposits- fine grey-blue dots (punctate spots) and/or blotches (coarse localized pigmentation with irregular margin) Comedo- like openings- dilated pores, may be filled with yellow plugs Corn pearls- rounded solid corned structures over the surface of lesions. Milium like cysts- intra epidermal yellow round globules The last three are comparatively common features of hypertrophic LP. Step 5: Diagnosis: The first step is crucial in differentiating between skin tumors (usually single lesions) and inflammatory conditions (eg. lichen planus, psoriasis, eczema) that are usually multiple. Further differentiations among the inflammatory disorders are based upon the patterns of their vascular and non-vascular findings. The latter are more common and varied in lichen planus than other inflammatory dermatoses. Dermoscopic literature1 so far has identified different vascular patterns like arborizing vessels, comma vessels, crown vessels, erythema, glomerular structures, hairpin vessels, irregular red lines, red horizontal lines, red atolls, lagoons, scleroderma pattern and structure less bluish patches. Polymorphous patterns with a combination of two or more types are also documented. In our study on lichen planus, 84% lesions showed an increased vascularity appearing as red globules, diffuse erythema, red dots and red lines. Red globules were the major vascular finding (32%) followed by diffuse erythema 20%, red dots 20% and red lines 14%. Red lines were usually arranged in a radial pattern along the projections of Wickham’s striae. In a study on dermoscopic differentiation of lichen planus and psoriasis by Vazquez et al.3 red lines and red dots constituted 80% of LP lesions whereas red globules were seen in a few (12%) patients. These variations may be attributed to the difference in the intensity of disease activity at the time of presentation to the dermatologist. Diffuse erythema around faint contours of WS was noticed in the very early lesions of lichen planus. Red lines and globules appeared as the disease became more established and progressive. Red lines and hairpin vessels were noted in between the projections of the WS, indicating the most active and progressing front of the lesion. Histologically, red dots represent the tip of the vessels at dermal papillae whereas the red globules are the tortuous ‘coiled up’ dermal capillaries. Red lines are deeper ectatic horizontal capillaries of subpapillary plexus. 2, 3, Blood vessels disappear fast with the appearance of coarse pigment granules. Other inflammatory skin disorders like psoriasis are characterized by homogenously distributed red globules and hairpin vessels with white scales. Chronic eczema commonly shows dotted vessels with yellow scales in patches on dull erythema.4 Dotted, linear and globular vessels are also considered major diagnostic criteria for melanoma. Arborizing, comma shaped, hairpin and crown vessels are highly sensitive and specific for basal cell carcinoma.5According to a study done by Vazquez et al.2,3, Wickham’s Striae- a nonvascular feature was the most significant and consistent dermoscopic feature of lichen planus (92%). However, in our study WS was observed in 100% of the initial papules of lichen planus. This discrepancy may be due to the inclusion of cases of hypertrophic LP in the former study whereas our study mostly included acute and sub acute papules and plaques of LP. The different patterns of WS noted were reticulate ( most common), arboriform, globular, linear and annular. In fact, WS in the initial lesions of lichen planus appeared as pale white globules or lines on a background of diffuse erythema under dermoscope. As the disease progressed, the lines were found to become thicker, vessels gained a particular shape and pigment granules started appearing at the margin of WS. The central yellow brown dots were noted in a few cases. In literature, these have been explained by vacuolar degeneration of basal keratinocytes and spongiosis in the spinous zone3. Therefore, prominent melanin incontinence occurs here. This can be corroborated with a dermoscope which shows the central yellow brown areas being gradually replaced by coarse brown to black pigment granules. Ultimately, as the lesions regress, coarse granules and dark blotchy pigmentation remain while the vascular features and WS disappear. Granular6 and blotchy pigmentation was observed in 36 patients (72%) along the borders of WS and also at the centre in mature LP lesions. Blotchy melanin deposits can be seen at areas where Wickham’s striae are slowly fading. LP lesions are devoid of the normal pigment network that is formed by the pattern of rete ridges of the epidermis. Instead a mature plaque of lichen planus is a combination of different colors ranging from pearly white WS, diffuse erythema to prominent red dots, globules and black to bluish black melanin deposits at selected areas of the plaques. Black dots7 are formed by non- uniform melanin accumulation in upper epidermis. Grey blue dots are produced by free melanin due to melanin incontinence to papillary dermis. Melanin in deeper layers of skin produce a bluish hue as light of shorter wavelength are more dispersed than those of longer wavelength. Blotches are structureless brown pigmentation caused by large concentration of melanin in epidermis and dermis obscuring the underlying structures. On histopathology melanophages are common in these areas. Other features like comedo like openings (9 lesions) and corn pearls (7 plaques) were observed in comparatively larger and long standing lesions. Comedo- like openings, also called pseudo follicular openings are crypts on the surface of the lesions. They are observed in seborrheic keratosis and papillomatous melanocytic nevi apart from lichen planus hypertrophicus. 2,8 However, in seborrheic keratosis, comedo like openings are surrounded by pigmented ‘network-like structures’ The histopathology shows hyperplastic, dilated, hypergranulotic infundibula with orthokeratosis.1 Corn pearls are rounded solid corned structures with well defined circular or oval margins present on the surface of lesions, occupying the crypts. They are believed to represent transepidermal elimination.1 Milia like cysts are intra epidermal keratin-filled cysts that appear as yellowish-white flat globular structures with irregular margin lying below the surface of the lesions. They are commonly seen in seborrheic keratosis,8 congenital nevi, papillomatous melanocytic nevi7 and acanthosis nigricans.6 Therefore, to conclude, dermoscopy, in addition to clinical examination is an effective and essential tool for diagnosing Lichen planus. It improves recognition of the pathognomonic feature- Wickham striae (often difficult to discern with naked eye), apart from the other supportive clues. Dermatoscopy thus provides a cost- effective non-invasive alternative to biopsy. Moreover, evolution of the disease can be studied in detail which adds to the overall knowledge of morphology and thereby helps our understanding of the disease and assessment of the disease activity. This in turn decides the necessity for aggressive management, if any.
REFERENCES Zalaudek I, Argenziano G, Di Stefani A, Ferrara G, Marghoob AA, Hofmann-Wellenhof R, Soyer HP, Braun R, Kerl H. Dermoscopy in general dermatology. Dermatology. 2006;212(1):7-18.
Vázquez-López F, Manjón-Haces JA, Maldonado-Seral C, Raya-Aguado C, Pérez-Oliva N, Marghoob AA. Dermoscopic features of plaque psoriasis and lichen planus: new observations. Dermatology. 2003;207(2):151-6. Zalaudek I, Lallas A, Moscarella E, Longo C, Soyer HP, Argenziano G. The dermatologist’s stethoscope—traditional and new application of dermoscopy. Dermatol Pract Conc. 2013;3(2):11.
Braun RP, Rabinovitz HS, Oliviero M, Kopf AW, Saurat JH. Dermoscopy of pigmented skin lesions. J Am Acad Dermatol. 2005 Jan;52(1):109-21. Review
Policy for Articles with Open Access
|
|
 Home
Home