Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 3 - December 2019
Comparison of various biomechanically studied items by Corvis ST and ocular response analyzer among myopic patients seeking refractive surgery
Tamer Adel Refai1*, M Tarek El-Naggar2
1,2Assistant Research Professor, Department of Ophthalmology, Refractive unit-Research Institute of ophthalmology –2 Al-Ahram street-Giza-EGYPT. Email:tamerrefai@hotmail.com
Abstract Purpose: comparing Corvis ST and ORA among myopic patients .Materials and Methods: (47) eyes of (25) patients with mild to high myopia with or astigmatism were subjected to comparative examination of their corneal biomechanics using Corvis ST for (IOPnct), (bIOP) in mmHg, (CCT) in microns, (DA)ratio, the integrated Radius in mm,the (ARTh), (SP-A1) and the Corvis Biomechanical Index(CBI).and Ocular Response Analyzer for the (IOPg), (IOPcc) (CH), (CRF), and,the (KS%). Studied item were subjected to statistical analysis. Observations and Results: Age range 18-41 years (28.64±7.02). A highly significant correlation (p<0.01) existed between both of non-corrected IOP(IOPnct) by Corvis ST and Goldmann-correlated IOP (IOPg) by ORA(r=0.66) and again between biomechanically corrected IOP(bIOP)by Corvis ST and corneal-compensated IOP (IOPcc)by ORA(r=0.63) . The CRF of ORAshowed a highly significant correlation (p<0.01) with the Integr.Radius, and SP-A1, a statistically significant correlation (p<0.05) with theCBI, (DA) ratio and a non significant correlation (p>0.05) with the ARTh of Corvis ST. with the exception of ARTh, the CH of ORA showed a non significant correlation (>0.05) with biomechanical items studied by Corvis ST. The KS% of ORAshowed a highly significant correlation (p<0.01) with the Integr. Radius,a statistically significant correlation (p<0.05) with the (DA) ratio and SP-A1, and a non significant correlation (p>0.05) with the CBI and ARTh of Corvis ST. The results of both Corvis ST and ORA were strongly affected by the central corneal thickness but not the age of patients. Conclusion: in normal myopic eyes, bIOP of corvis ST correlates significantly with the IOPcc of ORA. Also the CBI, DA ratio, SP-A1and Integrated. Radius of corvis ST correlates significantly with the CRF and to a lesser extent with the KS% but not with the CH of ORA. The results were significantly affected by central corneal thickness . Key words: Corvis –ORA-IOP-biomechanical criteria- myopia.
INTRODUCTION Studying the biomechanical properties of the cornea is vital for better understanding of the optical and the geometrical properties of the cornea 1.Determining of corneal biomechanical properties in vivo is of great clinical importance as it can help optimize several management procedures interacting or interfering mechanically with the eye; like measurement of intraocular pressure (IOP)2-3 for effective glaucoma management4-5, proper determining of keratoconus 6-10, refractive surgery planning11-12, evaluation and optimization of treatment protocols of collagen crosslinking.13-15 Also there is some evidence that significant corneal biomechanical alterations occurs in eyes with glaucoma and keratoconus.16-17 A commonly used device to measure the corneal biomechanical properties in vivo was the Reichert ORA, using a precisely metered collimated air pulse to move cornea inward, past a first applanation (flattening), and into a slight contractility. Then the pressure decreases and the cornea passes through a second applanation and returns to its normal curvature. The whole process of cornea deformation is recorded by an electo-optical infrared (IR) detection system2. It measures the Corneal Hysteresis (CH), which reflects corneal viscoelasticity, (corneal damping response), as well as the Corneal Resistance Factor (CRF), which reflects corneal rigidity. Both factors are considered useful in predicting the occurrence of post-Lasik ectasia 2.It also measures the Goldmann-correlated IOP measurement (IOPg) which simulates IOP measured by Goldmann tonometer and the Corneal-Compensated Intraocular Pressure (IOPcc) that takes corneal biomechanical properties into consideration as well as the keratoconus suspect percentage (KS%) (of the keratoconus match probabilities), also related to the degree of weakness of corneal biomechanics. The Corvis ST uses a consistent air puff to deform the cornea, along with an ultra-high speed Scheimpflug camera to capture images of the horizontal meridian at greater than 4,300 frames per second, resulting in 140 images during the 30ms air puff.18 It measures several indices related to the corneal biomechanical properties like deformation amplitude(DA) ratio and integrated Radius( both are considered dynamic Corneal Response parameters), the stiffness parameter at first applanation (SP-A1) (a novel stiffness parameter), Ambrósio’s Relational Thickness to the horizontal profile, which is based on the thickness profile in the temporal-nasal direction (ARTh) 19 and the Corvis Biomechanical Index(CBI),which represents optimal combination of best predictors from the individual indices for the accurate separation between normal and keratoconic eyes20.It also measures the non-corrected intraocular pressure in mmHg(IOPnct), the biomechanically corrected intraocular pressure (bIOP) in mmHg,the central corneal thickness(CCT) in microns. The bIOP is IOP corrected forthe central corneal thickness, patient’s age and the biomechanical properties of the cornea 3.In this research, we compared the different biomechanical indices as well as the IOP measurement taken by bothCorvis ST and ORA for myopic patients seeking ablative refractive surgery to have a better evaluation of these patients to try to avoid the risk of ectasia.
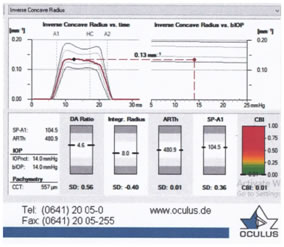
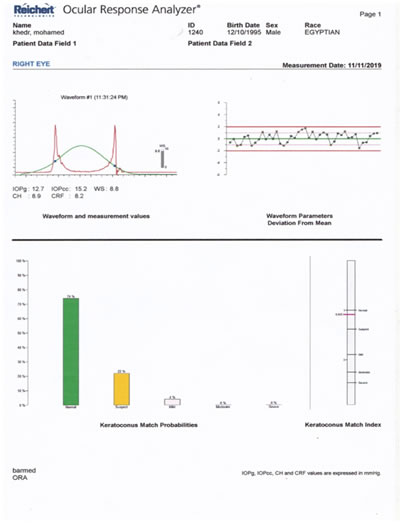
MATERIALS AND METHODS Forty-seven (47) eyes of twenty-five(25) patients with mild to high myopia with or astigmatism seeking for refractive correction at the research institute of ophthalmology-Egypt between July 2019 to November 2019, were subjected to examination for their corneal biomechanics using two machines; Corvis ST(CST; Oculus, Wetzlar, Germany) and Ocular Response Analyzer (ORA; Reichert, Buffalo, New York, USA). Patients were examined for uncorrected visual acuity, refraction measured by Topcon autorefractometer, best-corrected visual acuity Scheimflug imaging, followed by measurement of the corneal biomechanical properties by both the Corvis ST(CST; Oculus, Wetzlar, Germany) and Ocular Response Analyzer (ORA; Reichert, Buffalo, New York, USA). For The corvis ST, the following criteria were studied and recorded; the non-corrected intraocular pressure in mmHg(IOPnct), the biomechanically corrected intraocular pressure (bIOP) in mmHg, the central corneal thickness(CCT) in microns, the Deformation Amplitude (DA)ratio, the integrated Radius in mm(Integr.Radius), the Ambrósio’s Relational Thickness horizontal (ARTh), the stiffness parameter at first applanation (SP-A1) and the Corvis Biomechanical Index(CBI), all being considered to be related the biomechanical corneal properties (Fig 1). Fig 1: Corvis ST picture of one our patients, showing different studied items For the Ocular Response Analyzer, the following criteria were studied and recorded; the Goldmann-correlated IOP measurement (IOPg) which simulates IOP measured by Goldmann tonometer and the Corneal-Compensated Intraocular Pressure (IOPcc) that takes corneal biomechanical properties into consideration,the Corneal hysteresis CH, which reflects the corneal viscoelastic properties; the corneal resistance factor(CRF), which measures the whole corneal rigidity,the Keratoconus suspect percentage(KS%) (of the keratoconus match probabilities), which reflects the degree of weakness of corneal biomechanics. (Fig 2).
Fig 2: Ocular response analyzer picture of same studied patient in figure 1, showing different studied items.
Exclusion criteria included; Previous corneal or intraocular surgery, cases of diagnosed keratoconus and similar ectasias, previous history of ocular trauma, patients younger than 18 years , patients with ocular or systemic diseases that can affect corneal biomechanics a well as patients with history of eye trauma.For each studied item, statistical analysis was used to calculate the mean value,the standard deviation, the minimum and maxmum values. Comparison and correlation tests were also performed as needed .P value (>0.05) was considered as non significant, P value (<0.05) was considered as statistically significant,while P value (<0.01) was considered as highly significant.
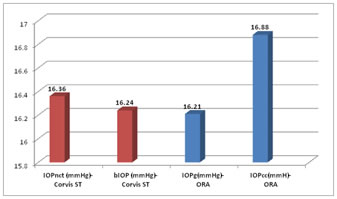
OBSERVATIONS AND RESULTS The age ranged from 18-41 years (mean 28.64±7.02).By corvis ST, the non-corrected intraocular pressure(IOPnct) ranged from 12-24 mmHg(mean 16.36±2.36), the biomechanically corrected IOP(bIOP) ranged from 12.9-22.8 mmHg(mean 16.24±1.93),the central corneal thickness ranged from 477 to 590 μm (mean 542.83±25.05), the deformation amplitude(DA) ratio at 2mm ranged from 3.7 to 5.4 (mean 4.33±0.41), the integrated Radius(Integr.Radius) ranged from 6.7 to 11.2mm (mean 7.79±0.95),the Ambrósio’s Relational Thickness horizontal ranged from 42.2 to 677.2 (mean 476.00±99.76), the stiffness parameter at first applanation(SP-A1) ranged from 70-143.5 (mean 107.62±17.18) and the Corvis Biomechanical Index(CBI) ranged from 0-0.87 (mean 0.10±0.20).By the Ocular Response Analyzer (ORA), the Corneal hysteresis(CH) ranged from 4.8 to 13 (mean 10.05±1.47), the Corneal resistsnce factor (CRF) ranged from 7.4 to 13.4 (mean 10.45±1.49), the Goldmann-correlated IOP (IOPg) ranged from 6.4-27.1 mmHg (mean 16.21±3.87), the corneal-compensated IOP (IOPcc) ranged from 8.5-32.1 (16.88±3.91) and the Keratoconus suspect percentage(KS%) (of the keratoconus match probabilities) ranged from 0-65% (mean 11.98±13.73) (Table 1 and Chart 1). Table 1:Demographic data for Corvis and ORA
Chart 1: Showing the mean values for the IOP(nct) and bIOP measured by Corvis ST as well as IOPg and IOPcc measured by ORA ,among patients under study. Regarding the Corvis ST,the mean value for the non-corrected IOP(IOPnct) was 16.36±2.36mmHg and for the biomechanically corrected IOP(bIOP) was 16.24±1.93 mmHg with the T-test=1.08,p=0.28,i.e; p>0.05, denoting a non significant difference(Table 2). Table 2: comparison of the mean value and standard deviation of both the IOPnct and the bIOP by Corvis and their comparison by t-test among patients under study
Regarding the ORA,the mean value for the Goldmann-correlated IOP (IOPg) was 16.21±3.87mmHg and for the corneal-compensated IOP (IOPcc) was16.88±3.91 mmHg with the T-test=3.11,p=0.00,i.e; p<0.05, denoting a statistically significant difference (Table 3).
Table 3: comparison of the mean value and standard deviation of both the IOPg and the IOPcc by ORA and their comparison by t-test among patients under study
Pearson correlation test showed a highly significant correlation (r=0.66,p<0.01) between non-corrected IOP(IOPnct) by Corvis ST and Goldmann-correlated IOP (IOPg) by ORA (Table 4).
Table 4:showing correlations between IOPnct by Corvis ST and the IOPg by ORA among cases under study
Pearson correlation test showed a highly significant correlation (r=0.63,p<0.01) between biomechanically corrected IOP(bIOP)by Corvis ST and corneal-compensated IOP (IOPcc) by ORA (Table 5).
Table 5:showing correlations between bIOP by Corvis ST and the IOPcc by ORA among cases under study
Pearson correlation test showed a highly significant correlation (p<0.01) between non-corrected IOP measurements by Corvis ST and central corneal thickness (CCT) (r=0.47).It also showed a statistically significant correlation(p<0.05) between CCT and both of biomechanically corrected IOP(bIOP)by Corvis ST(r=0.20) and Goldmann-correlated IOP (IOPg) by ORA(r=0.23) (Table 6). However, it showed a non significant correlation (p>0.05) between CCT and cornea compensated IOP(IOPcc) measurements made by ORA(r=0.13) (Table 6).
Table 6:showing correlations between Intraocular pressue valuesss measured by both Corvis ST and ORA and central corneal thickness (CCT) among cases under study
Pearson correlation test showed a non significant correlation (p>0.05) between age of patients in years and each of non-corrected IOP(IOPnct) ( r=-0.03) , biomechanically corrected IOP(bIOP) ( r=0.06) by Corvis ST and Goldmann-correlated IOP (IOPg) ( r=0.13) ,cornea compensated IOP(IOPcc) ( r=0.15) measurements made by ORA (Table 7).
Table 7 :showing correlations between Intraocular pressue values measured by both Corvis ST and ORA and the age of patients (years) among cases under study
Pearson correlation of Corvis biomechanical index(CBI) by Corvis ST and biomechanical criteria studied by ORA revealed a statistically significant correlation(p<0.05) between Corvis biomechanical index(CBI) by Corvis and Corneal resistsnce factor (CRF) (r=-0.21) of ORA but;with a non significant correlation (p>0.05) with both the Corneal hysteresis(CH) (r=-0.03) and Keratoconus suspect percentage(KS%) (r=0.19) of the ORA (Table 8).
Table 8 :showing correlations between Corvis biomechanical index(CBI) by Corvis ST and biomechanical criteria studied by ORA among cases under study
Pearson correlation of the deformation amplitude(DA) ratio at 2mm by Corvis ST and biomechanical criteria studied by ORA revealed a statistically significant correlation(p<0.05) between deformation amplitude(DA) ratio at 2mm by Corvis and both of Corneal resistsnce factor (CRF) (r=-0.40) and Keratoconus suspect percentage(KS%) (r=0.35) of ORA but;with a non significant correlation with the Corneal hysteresis(CH) of the ORA(p>0.05,r=-0.05) (Table 9). Table 9:showing correlations between Deformation Amplitude(DA) ratio by Corvis and biomechanical criteria studied by ORA among cases under study
Pearson correlation of the integrated Radius(Integr.Radius) by Corvis ST and biomechanical criteria studied by ORA revealed a highly significant correlation(p<0.01) between integrated Radius(Integr.Radius) by Corvis and both of Corneal resistance factor (CRF) (r=-0.46) and Keratoconus suspect percentage(KS%) (r=0.58) of ORA but;with a non significant correlation with the Corneal hysteresis(CH) of the ORA(p>0.05,r=-0.11) (Table 10).
Table 10: showing correlations between integrated radius by Corvis ST and biomechanical criteria studied by ORA among cases under study
Pearson correlation of the Ambrósio’s Relational Thickness horizontal (ARTh)by Corvis ST and biomechanical criteria studied by ORA revealed a statistically significant correlation(p<0.05) between Ambrósio’s Relational Thickness horizontal (ARTh) by Corvis and Corneal hysteresis(CH) (r=0.26) of ORA, but;with a non significant correlation(p>0.05) with the Corneal resistance factor (CRF) (r=0.18) and Keratoconus suspect percentage(KS%) (r=-0.19) of ORA (Table 11).
Table 11: showing correlations between Ambrósio’s Relational Thickness horizontal (ARTh) by Corvis ST and biomechanical criteria studied by ORA among cases under study
Pearson correlation of the stiffness parameter at first applanation(SP-A1) by Corvis and biomechanical criteria studied by ORA revealed a highly significant correlation(r=0.43,p<0.01) with the Corneal resistance factor (CRF),a statistically significant correlation(r=-0.25,p<0.05) with the Keratoconus suspect percentage(KS%) of ORA but;with a non significant correlation with the Corneal hysteresis(CH) (r=0.04) (p>0.05) (Table 12).
Table 12: showing correlations between stiffness parameter at first applanation(SP-A1) by Corvis and biomechanical criteria studied by ORA among cases under study
Pearson correlation revealed a highly significant correlation(p<0.01) between the central corneal thickness(CCT) studied by Corvis and each of Corvis parameters; deformation amplitude(DA) ratio at 2mm (r=-0.53), Integrated.Radius (r=-0.44), stiffness parameter at first applanation(SP-A1) (r=0.67), as well as Corvis Biomechanical Index(CBI) (r=-0.54) , but with a statistically significant correlation with the Ambrósio’s Relational Thickness Horizontal(ARTh) (r=0.39,p<0.05) (Table 13).
Table 13:showing correlations between various biomechanical indices studied by Corvis and central corneal thickness(CCT) studied by Corvis among cases under study
Pearson correlation revealed a statistically significant correlation(p<0.05) between the central corneal thickness(CCT) and both of Corneal resistance factor (CRF) (r=0.27),and Keratoconus suspect percentage(KS%)(r=-0.27) but with a non significant correlation (>0.05) with Corneal hysteresis(CH) (r=0.19),of ORA (Table 14).
Table 14:showing correlations between various biomechanical indices studied by ORA and central corneal thickness(CCT) among cases under study
Pearson correlation revealed a statistically significant correlation(p<0.05) between the age of patient in years a and each of Corvis parameters; deformation amplitude(DA) ratio at 2mm (r=0.24) , as well as Corvis Biomechanical Index(CBI) (r=0.24) ,but with a non significant correlation (P>0.05) with each of Integrated.Radius (r=0.09), (Ambrósio’s Relational Thickness Horizontal(ARTh) (r=-0.08) as well as stiffness parameter at first applanation(SP-A1) (r=0.12) (Table 15).
Table 15:showing correlations between various biomechanical indices studied by Corvis and the age among cases under study
Pearson correlation revealed a non significant correlation(p>0.05) between the age of patient(years) and each of Corneal hysteresis(CH) (r=-0.11),Corneal resistance factor (CRF) (r=-0.01),and Keratoconus suspect percentage(KS%)(r=0.01) of ORA (Table 16).
Table 16: showing correlations between various biomechanical indices studied by ORA and the age among cases under study
DISCCUSION Studying the biomechanical properties of the cornea is of great clinical importance as helps better evaluation of refractive surgery patients11-12, accurate keratoconus diagnosis13, accurate measurements of intraocular pressure for proper glaucoma management 4-5, in addition to studying treatment protocols of collagen crosslinking13,15.Some studies on biomechanical properties used the Ocular response analyzer 2,21,while others used the Corvis ST3-4,18-20.Matsuura etal 2016,studied Ninety-five eyes of 95 POAG patients (53 males and 42 females) .They found more Corvis ST parameters to be significantly correlated with CRF than CH, however, the magnitude of the correlation coefficients were weak to moderate at best 22.Joda etal 2015, studied correlations of the Corvis ST non-corrected IOP with both central corneal thickness and age,they found a strong correlation with CCT (r2 = 0.204) and weaker correlation with age (r2 = 0.009) 3.Vinciguerra etal 2016, studied patients from two clinics located on different continents to test the capability of the CBI to separate healthy and keratoconic eyes in more than one ethnic group using the Corvis ST, they found that CBI With a cut-off value of 0.5, 98.2% of the cases were correctly classified as keratoconic with 100% specificity and 94.1% sensitivity(in the training dataset). In the validation dataset, the same cut-off point correctly classified 98.8% of the cases as keratoconic with 98.4% specificity and 100% sensitivity 20.Zhang et al 2013, conducted a study of normal myopic eyes (from 240 healthy volunteers), with ages ranging from 18 to 44 years (mean, std: 23.84 ± 5.08) and they found a good correlation between CH, CRF, and CCT (CH: r = 0.54, p = 0.000, CRF: r = 0.61, p = 0.000), however, no statistical significant correlation was found between CH, CRF and age 21. In our study, Regarding the Corvis ST,the mean value for the non-corrected IOP(IOPnct) was 16. 36 ±2. 36mmHg and for the biomechanically corrected IOP(bIOP) was 16. 24 ±1.9 3mmHg with the T-test, denoting a non significant difference(p>0.05). Regarding the ORA,the mean value for the Goldmann-correlated IOP (IOPg) was 16.21±3.87mmHg and for the corneal-compensated IOP (IOPcc) was16.88±3.91 mmHg with the T-test denoting a non significant difference(p>0.05). Pearson correlation test showed a highly significant correlation (p<0.01) between both non-corrected IOP(IOPnct) by Corvis ST and Goldmann-correlated IOP (IOPg) by ORA and also between biomechanically corrected IOP(bIOP)by Corvis ST and corneal-compensated IOP (IOPcc) by ORA .Pearson correlation test showed a highly significant correlation (p<0.01) between non-corrected IOP measuements by Corvis ST and central corneal thickness (CCT) (r=0.47).It also showed a statistically significant correlation(p<0.05) between CCT and both of biomechanically corrected IOP(bIOP)by Corvis ST(r=0.20) and Goldmann-correlated IOP (IOPg) by ORA(r=0.23) and these results agreed with the results found by Joda etal 2015 3. However, it showed a non significant correlation (p>0.05) between CCT and cornea compensated IOP(IOPcc) measurements made by ORA(r=0.13) and this might be attributed to the correction of the IOPcc according to corneal thickness.Pearson correlation test showed a non significant correlation (p>0.05) between age of patients in years and each of non-corrected IOP(IOPnct), biomechanically corrected IOP(bIOP) by Corvis ST and Goldmann-correlated IOP (IOPg),cornea compensated IOP(IOPcc) measurements made by ORA and again these results agreed with the results found by Joda etal 2015 3.Corvis Biomechanical Index(CBI) ranged from 0-0.87 (mean 0.10±0.20) and these values agreed with the study made by Vinciguerra etal 2016 20that statedthat the cut-off value of abnormality 0.5 and above . The deformation amplitude (DA) ratio at 2mm ranged from 3.7 to 5.4 (mean 4.33±0.41), the integrated Radius(Integr.Radius) ranged from 6.7 to 11.2mm (mean 7.79±0.95),the Ambrósio’s Relational Thickness horizontal ranged from 42.2 to 677.2 (mean 476.00±99.76), the stiffness parameter at first applanation(SP-A1) ranged from 70-143.5 (mean 107.62±17.18),but these items were not included in the study made by Vinciguerra etal 2016 [20].Pearson correlation of Corvis biomechanical index(CBI) by Corvis ST and biomechanical criteria studied by ORA revealed a statistically significant correlation(p<0.05) between Corvis biomechanical index(CBI) by Corvis and Corneal resistsnce factor (CRF) of ORA but;with a non significant correlation (p>0.05) with both the Corneal hysteresis(CH) and Keratoconus suspect percentage(KS%) of the ORA .Pearson correlation of the deformation amplitude(DA) ratio at 2mm by Corvis ST and biomechanical criteria studied by ORA revealed a statistically significant correlation(p<0.05) between deformation amplitude(DA) ratio at 2mm by Corvis and both of Corneal resistsnce factor (CRF) and Keratoconus suspect percentage(KS%) of ORA but;with a non significant correlation with the Corneal hysteresis(CH) of the ORA(p>0.05) .Pearson correlation of the integrated Radius(Integr.Radius) by Corvis ST and biomechanical criteria studied by ORA revealed a highly significant correlation(p<0.01) between integrated Radius(Integr.Radius) by Corvis and both of Corneal resistsnce factor (CRF) and Keratoconus suspect percentage(KS%) of ORA but;with a non significant correlation with the Corneal hysteresis(CH) of the ORA(p>0.05) . Pearson correlation of the Ambrósio’s Relational Thickness horizontal (ARTh)by Corvis ST and biomechanical criteria studied by ORA revealed a statistically significant correlation(p<0.05) between Ambrósio’s Relational Thickness horizontal (ARTh) by Corvis and Corneal hysteresis(CH) of ORA, but;with a non significant correlation(p>0.05) with the Corneal resistsnce factor (CRF) and Keratoconus suspect percentage(KS%) of ORA .Pearson correlation of the stiffness parameter at first applanation(SP-A1) by Corvis and biomechanical criteria studied by ORA revealed a highly significant correlation(p<0.01) with the Corneal resistsnce factor (CRF),a statistically significant correlation(p<0.05) with the Keratoconus suspect percentage(KS%) of ORA but;with a non significant correlation with the Corneal hysteresis(CH) (r=0.04) (p>0.05) .These correlations between biomechanical parameters of the Corvis ST and the ORA in our study agreed with the study of Matsuura etal 2016 [22],in whichmore Corvis ST parameters were significantly correlated with CRF than CH 21, but we found a correlation ( although not statistically significant) between Corvis ST biomechanical indices and the keratoconus suspect percentage of the ORA and these correlations were not included in the study maded by Matsuura etal 2016 22.Pearson correlation revealed a highly significant correlation(p<0.01) between the central corneal thickness(CCT) studied by Corvis and each of Corvis parameters; deformation amplitude(DA) ratio at 2mm , Integrated.Radius (r=-0.44), stiffness parameter at first applanation(SP-A1) , as well as Corvis Biomechanical Index(CBI), but with a statistically significant correlation with the Ambrósio’s Relational Thickness Horizontal(ARTh) (p<0.05) .Also Pearson correlation revealed a statistically significant correlation(p<0.05) between the age of patient in years a and each of Corvis parameters; deformation amplitude(DA) ratio at 2mm (r=0.24) , as well as Corvis Biomechanical Index(CBI) (r=0.24) ,but with a non significant correlation (P>0.05) with each of Integrated.Radius, (Ambrósio’s Relational Thickness Horizontal(ARTh) as well as stiffness parameter at first applanation(SP-A1)and these correlations were not included in the previously mentioned studies that focused on intraocular pressure measurements by Corvis ST in particular rather than other parameters. Similarly, a statistically significant correlation(p<0.05) was found between the central corneal thickness(CCT) and both of Corneal resistsnce factor (CRF) (r=0.27),and Keratoconus suspect percentage(KS%)(r=-0.27) but with a non significant correlation (>0.05) with Corneal hysteresis(CH) (r=0.19),of ORA. Also Pearson correlation revealed a non significant correlation(p>0.05) between the age of patient(years) and each of Corneal hysteresis(CH) (r=-0.11),Corneal resistsnce factor (CRF) (r=-0.01),and Keratoconus suspect percentage(KS%)(r=0.01) of ORA and these results (apart from corneal hysteresis; which is a measure of the corneal viscoelastic properties rather than corneal rigidity) agreed with results found by Zhang et al 2013 22,however they do not study thekeratoconus suspect percentage which was included in our study .
CONCLUSION in normal myopic eyes, bIOP of corvis ST correlates significantly with the IOPcc of ORA. Also the CBI, DA ratio, SP-A1 and Integrated.Radius of corvis ST correlates significantly with the CRF and to a lesser extent with the KS% but not with the CH of ORA.The results were are significantly affected by central corneal thickness but not age of patients.
ACKNOWLEDGMENT Acknowledgments are made for the Refractive Unit in theResearch Institute of Ophthalmology, Giza, Egypt, that funded the research and specially for Professor Dr.Mostafa Salah-EL-Din;the previous Head of the Refractive unit of the Institute for his efforts in providing the refractive unit with the Corvis ST; the chief tool in this Research.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home