|
Table of Content - Volume 14 Issue 1 - April 2020
Efficacy of amniotic membrane grafting after pterygium excision surgery
Aditya S Parmar1*, M B Dongre2, E B Shelke3, H N Yerkade4
1Junior Resident, 2Professor & HOD, 3Associate Professor, 4Assistant Professor, Department of Ophthalmology, S.R.T.R.G.M.C., Ambajogai, Beed, Maharashtra, INDIA. Email: : adi8392@gmail.com , dr.mbd@rediffmail.com , ebshelke35@gmail.com, harshalyerkade@gmail.com
Abstract Background: Pterygium is a common disorder of ocular surfaceand several different surgeries are being performed to decrease the high recurrence of bare sclera technique, such as conjunctival autografting and amniotic membrane grafting. Aim: To evaluate the effect of pterygium size on corneal astigmatism before and after pterygium excision surgery with amniotic membrane grafting; and the benefits and safety of amniotic membrane grafting in pterygium surgery. Material and Methods: A total of 100 patients with primary pterygium underwent pterygium excision surgery with amniotic membrane grafting. All patients were subjected to clinical refraction at 6 weeks after recording uncorrected and best corrected visual acuity on Snellen’s chart. Results: Out of the 100 patients 95 patients (95%) had improvement in unaided visual acuity of one line or more on Snellen’s chart and the remaining 5 patients (5%) had no improvement in unaided visual acuity. There was a highly significant difference in residual astigmatism with increasing grade/size of pterygium. None of the patients had recurrence or graft infection or any vision threatening complications. Conclusion: Early excision of pterygium with amniotic membrane grafting should be employed in all cases of pterygium as early as possible as it is safe, highly effective modality in the management of primary pterygium. Keywords: Primary pterygium, amniotic membrane grafting, visual acuity, astigmatism, complications
INTRODUCTION Pterygium is a common disorder of ocular surface in many parts of world described as ophthalmic enigma. Pterygium is commonly seen in India, which is a part of the pterygium belt.1It leads to significant astigmatism is actually a wing shaped, triangular, degenerative, fibrovascular connective tissue of bulbar conjunctiva which moves towards and onto the cornea. Vision may be reduced due to direct invasion of the visual axis or astigmatism induced by the pterygium.2In the treatment, several different surgeries are being performed to decrease the high recurrence of bare sclera technique, such as conjunctival autografting and amniotic membrane grafting.3 In the present study, we aimed to evaluate the effect of pterygium size on corneal astigmatism before and after pterygium excision surgery with amniotic membrane grafting; and the benefits and safety of amniotic membrane grafting in pterygium surgery.
MATERIAL AND METHODS This cross-sectional observational study was conducted on 100 cases of primary pterygium attending outpatient Department of Ophthalmology, in a Tertiary care centre in Rural Maharashtra. Inclusion criteria
Exclusion criteria:
Approval from Institutional Ethics Committee was taken before starting study. Informed written consent of all patients included in the study was taken after explaining the procedure and purpose of the study to the patients. A complete history was taken which included complaints of diminution of vision, its onset, duration and progress, complaints of redness, pain, watering and discharge from eyes, photophobia, past history of ocular injury, any systemic illness and previous ocular surgery. Then the patient was examined under diffuse illumination and by using the slit lamp. The size of the pterygium and its extent was noted and the pterygium was graded accordingly by using the slit lamp. The orbital anatomy was noted and also the normalcy of the lid closure was noted. After this patient underwent refraction, automated keratometry and autorefractometry. Grading of pterygium was done.2All patients selected for the study were subjected to following detailed ocular examination:Visual acuity, IOP measurement, slit lamp biomicroscopy, automated keratometry, autorefractometry, lacrimal sac syringing and refraction. All routine investigations like Hemoglobin, Complete blood count, Random blood sugar level, urine routine and microscopy, ECG, ELISA, HBsAg were done. All patients underwent pterygium excision surgery with amniotic membrane grafting using 10-0 nylon sutures under combined topical and subconjunctival anaesthesia. Pre-operative preparation All patients received Tab. ciprofloxacin 500mg twice a day and topical ciprofloxacin eye drops (0.3%) one drop four times a day, one day prior to surgery. Xylocaine sensitivity was done in all patients. Tablet Diazepam 5 mg or similar anti-anxiety medications were considered for anxious patients. Technique of Topical Anaesthesia Patients in Topical anaesthesia group (Group-B) received Proparacaine Hydrochloride 0.5%, it was instilled 6 times (approximately 40 µl per dose) starting 30 minutes before surgery. Five minutes before surgery one more time topical anesthetic was instilled on the cornea. Pain during surgery was controlled with additional 2 doses of topical anesthetic if required. Patients were instructed to keep their eyes closed after instillation of topical anesthetic. The patients were in the supine position on the operating table with their eyes open and requested to minimize movement of eyeball. Surgical technique Under all aseptic precautions painting with povidone iodine and draping was done. Wire speculum was applied. A single drop of Proparacaine Hydrochloride 0.5% was instilled at the outset of surgery. Subconjunctival local anaesthesia was given in all the cases using 0.25-0.5cc of 2% xylocaine and 0.5% bupivacaine (4:1) injection within the body of pterygium. The head of the pterygium was separated from the limbus and dissected towards the center of the cornea using conjunctival scissors. The head and part of the body were then excised. Residual fibrovascular tissue on the cornea was scraped with size 11 surgical blade or a crescent knife. The Tenon’s capsule and subconjunctival fibrovascular tissues were separated from the overlying conjunctiva and excised upward and downward towards the medial caruncle being careful not to damage the medial rectus tendinous attachment leaving an area of bare sclera. Bleeding vessels were gently cauterized with wet field cautery. Minimal use of cautery was done. Hemostasis was also achieved by pressure over bleeding points with the help of cotton buds. After the excision of the pterygium, the defect is then closed with human processed amniotic membrane. The defect is measured with the help of Castrovejo’s caliper and amniotic membrane of required size is taken and then placed over the bare sclera with the basement membrane side up. The amniotic membrane is sutured through the episcleral tissue to the adjacent at the edge of the bare sclera border with 10-0 nylon sutures. Ciprofloxacin eye ointment 0.3% was instilled and eyepadding was done. Post-operative management On the 1st postoperative day eye pad was removed and eye was cleaned. Topical antibiotic steroid eye drops were started every 2 hourly and tapered for next 6 weeks. Patients were asked to follow up on the 1st, 3rd, 7th day and 6 weeks. Assessment included ocular symptoms, slit lamp examination for graft position, complications and recurrence. Recurrences were evaluated at 6 weeks and 3rd month. All patients were subjected to clinical refraction at 6 weeks after recording uncorrected and best corrected visual acuity on Snellen’s chart. Statistical analysis Qualitative data was represented in the form of frequency and percentage. Association between variables was carried out with Chi Square test. Quantitative data represented using mean and SD. Pre-operative and post-operative comparison was done with paired t test. ANOVA was used to compare the mean difference between three groups. A P value of <0.05 was considered statistically significant. IBM SPSS Version 22 for windows was used to do statistical analysis.
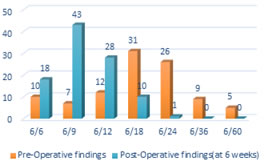
RESULTS Maximum number of patients were in the age group of 40-49 years which included 51 patients (51%) followed by 30-39 years which had 27 patients (27%). This signifies that pterygium is more common in the working age group. The minimum age was 19 years and maximum age was 54 years. The mean age was 40.14 years and the standard deviation was 7.60.70 patients were females(70%) and 30 patients were males(30%) showing a clear female preponderance in the study. Male to female ratio was 0.42:1. In our study, 48 patients (48%) underwent right eye pterygium excision with amniotic membrane grafting and 52 patients (52%) underwent left eye pterygium excision with amniotic membrane grafting. Majority of the patients; i.e. 78 patients(78%) presented with Grade 2 pterygium. 13 patients(13%) had grade 3 pterygium and 9 patients(9%) had grade 1 pterygium. All patients had primary nasal pterygium. Figure 1: Pre-operative unaided vision v/s Post-operative unaided vision
In the present study, maximum patients had 6/18(31 patients, 31%) unaided pre-operative vision, followed by 6/24(26 patients, 26%) and 6/12(12 patients, 12%). Maximum patients had 6/9(43 patients, 43%) unaided post-operative vision, followed by 6/12(28 patients, 28%) and 6/6(18 patients, 18%). There is a shift of frequencies from poorer visual acuity (6/18, 6/24) to better visual acuity (6/9, 6/12) after pterygium surgery. Out of the 100 patients 95 patients (95%) had improvement in unaided visual acuity of one line or more and the remaining 5 patients (5%) had no improvement in unaided visual acuity.
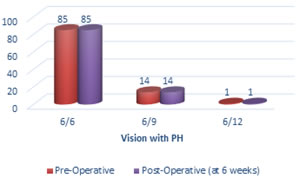
Figure 2: Pre-operative v/s Post-operative vision with pinhole It was observed that all patients had the same vision with pinhole even after surgery. This was probably because none of the patients had a pterygium large enough to impinge on the visual axis. 85 patients (85%) had vision with pinhole 6/6. 14 patients (14%) had vision with pinhole 6/9 and only one patient had vision with pinhole 6/12.
Table 1: Pre-operative v/s Post-operative astigmatism according to keratometry values
It was observed on the basis of keratometry values, that the pre-operative mean astigmatism in Grade 1 pterygium was 0.83 D. Whereas, it increased to 1.38 D in Grade 2 pterygium and further to 1.50 D in Grade 3 pterygium. The P value<0.02 showed there was a significant increase in astigmatism with increasing grade/size of pterygium. Also, the post-operative mean astigmatism according to keratometry values in Grade 1 pterygium was 0.44 D, 0.66 D in Grade 2 pterygium and 1.06 D in Grade 3 pterygium. The P value<0.001 proved there was a highly significant difference in residual astigmatism with increasing grade/size of pterygium. Comparing the pre and post-operative astigmatism according to keratometry values, P values for Grade 1, Grade 2 and Grade 3 were 0.002, 0.001 and 0.005 respectively. This signifies that pterygium surgery causes a highly significant change in astigmatism by decreasing it. All patients underwent subjective refraction and the astigmatism giving best corrected visual acuity was noted.
Table 2: Pre-operative v/s Post-operative astigmatism by manifest refraction
Out of the 100 patients that were operated, 8 patients (8%) had no change in manifest astigmatism, 2 (2%) patients had increase, and the remaining 90 patients (90%) had improvement in manifest astigmatism. 8 patients out of these 90 patients had been rendered free of spectacle/contact lens usage, i.e. their manifest refraction was nil. In our study, the pre-operative mean astigmatism by manifest refraction in Grade 1 pterygium was 0.66 D, which increased to 1.25 D in Grade 2 pterygium and further to 1.46 D in Grade 3 pterygium. The P value by ANOVA test was <0.008, which showed there was a highly significant increase in astigmatism with increasing grade/size of pterygium. The post-operative mean astigmatism by manifest refraction in Grade 1 pterygium was 0.31 D, 0.61 D in Grade 2 pterygium and 0.61 D in Grade 3 pterygium. The P value which was <0.001 proved there was a highly significant difference in residual astigmatism with increasing grade/size of pterygium. Comparing the pre and post-operative astigmatism according to manifest refraction, P values for Grade 1, Grade 2 and Grade 3 were 0.007, 0.001 and 0.001 respectively. Therefore, there was a highly significant difference between pre and post-operative astigmatism in pterygium patients.
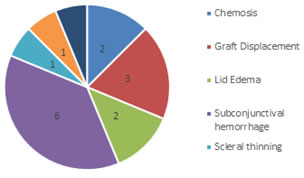
Figure 3: Post-operative complications
In our study out of 100 patients, only 16 patients had complications over the 3 month follow up period. The most frequently observed complication was subconjunctival hemorrhage (6 patients), followed by graft displacement (3 patients). 2 patients had chemosis and 2 had lid edema on post-operative day 1. 1 patient developed sclera thinning which presented at 6 week follow-up. One patient developed conjunctival cyst at 3 months and one patient developed Dellen ulcer at 3 months. Subconjunctival hemorrhage was seen on post-operative day 1 and was managed by oral Vitamin C supplementation and it subsided in all patients by post-operative day 14. Chemosis and Lid edema seen in immediate post-operative period was treated with topical Flurbiprofen 0.003% eyedrops and increasing the dose frequency of topical steroid+antibiotic combination and was cured by post-operative day 3. Scleral thinning was seen in one patient which was probably due to use bipolar cautery and was managed by multi-layered amniotic membrane grafting and suturing with 10-0 Ethilon. Graft displacement was seen in 3 patients on post operative day 1 and the patients were subjected to graft re-suturing. 1 patient developed Dellen ulcer on post-operative day 7. 1 patient developed conjunctival cyst on post-operative 3 months which was treated with excision followed with the same topical treatment. Notably, none of the patients developed recurrence, proving that pterygium excision with amniotic membrane grafting reduces recurrence of pterygium. However, a longer follow-up is required for a better documentation of recurrence. Majority of the complications were seen in the patients with Grade 2 pterygium, followed by Grade 3 pterygium patients. No complications were seen in Grade 1 pterygium patients. By using Chi-square test, P value was <0.277 which suggests no significant difference in post-operative complications with increasing size of pterygium. Such a distribution might be because a large majority (78%) of the patients had Grade 2 pterygium. However, the more serious complications like sclera thinning and Dellen ulcer were seen in patients with Grade 3 pterygium.
DISCUSSION In our study, majority of the patients; i.e. 78 patients (78%) presented with Grade 2 pterygium. 13 patients (13%) had grade 3 pterygium and 9 patients (9%) had grade 1 pterygium. All patients had primary nasal pterygium. A study by Maheshwari S on 36 eyes showed that 16 eyes (44.45%) had Grade 2 pterygium, 12 eyes (33.33%) had grade 3 pterygium, 7 eyes (19.45%) had grade 4 pterygium and 1 eye (2.77%) had a double headed pterygium. None of the patients had Grade 1 pterygium in that study.2 Pterygia do not only lead to visual impairment by invading the visual axis or distorting the central topography, but they also induce a focal corneal flattening and severe astigmatism.4 In the present study, maximum patients had 6/18(31 patients, 31%) unaided pre-operative vision and maximum patients had 6/9(43 patients, 43%) unaided post-operative vision. Out of the 100 patients, 95 patients (95%) had improvement in unaided visual acuity of one line or more on Snellen’s chart and the remaining 5 patients (5%) had no improvement in unaided visual acuity and none of the patients had deterioration in vision after surgery. Gumus et al. in their study of 40 eyes in 34 patients observed statistically lower uncorrected visual acuity in patients with pterygium in comparison to their uncorrected visual acuity after surgery.4 Previous studies have shown pterygium induces with-the-rule astigmatism.5-7 In our study, all patients had with the rule astigmatism. It was observed on the basis of automated keratometry values, that the pre-operative astigmatism in Grade 1 pterygium was 0.83±0.66D, whereas, it increased to 1.38±0.61D in Grade 2 pterygium and further to 1.50±0.49D in Grade 3 pterygium. The P value<0.02 showed there was a significant increase in astigmatism with increasing grade/size of pterygium. Avisar et al. conducted a study on 94 eyes with primary pterygium with the help of computerized topography and concluded that significant astigmatism was induced by pterygium larger than 1mm from the limbus and it tends to increase with increasing size of the pterygium. The study also suggested an early surgical intervention when the pterygium size was more than 1mm from the limbus.6 The results of pre-operative astigmatism were confirmed by checking manifest refraction in the patients. The pre-operative astigmatism by manifest refraction in Grade 1 pterygium was 0.66±0.72 D, which increased to 1.25±0.61 D in Grade 2 pterygium and further to 1.46±0.57 D in Grade 3 pterygium. The P value by ANOVA test was <0.008, thus, providing more evidence that there was a highly significant increase in astigmatism with increasing grade/size of pterygium. On comparing the pre and post-operative astigmatism by keratometry, Grade 1 pterygium patients had 0.83±0.66D astigmatism which reduced to 0.44±0.62D postoperatively with a highly significant P<0.002 showing a highly significant reduction in astigmatism after surgery. Similarly, Grade 2 pterygium patients had preoperative astigmatism 1.38±0.61D which reduced to 0.66±0.30D with P value<0.001. Grade 3 pterygium patients had preoperative astigmatism 1.50±0.49D which reduced to 1.06±0.65D after surgery, with P value<0.005. Therefore, there was a highly significant decrease in astigmatism after pterygium excision surgery. These findings were similarly seen on manifest refraction wherein all 3 classes showed highly significant reduction in astigmatism post-operatively. Maheshwari S in her study on 140 eyes with pterygium, observed refractive cylinder reduction from 1.94–2.24D to 0.78–1.07D, which is similar to our study.2In another study by her, the preoperative refractive cylinder was 4.60±2D, which improved to 2.20±2.04D with surgery.2Popat etal in his study on 100 eyes with pterygium showed that amount of corneal astigmatism induced by pterygium increases in direct proportion with the size of pterygium. Also, the postoperative decrease in astigmatism is also more in those patients with a larger pterygium. Mean astigmatism on keratometry was found to be 6.20±3.58D preoperatively which subsequently decreased to 1.20±1.27D on post-operative day 45.8 Garg P et al. studied the changes in corneal astigmatism before and after pterygium excision as well as with differences between various surgical techniques like bare sclera, conjunctival autograft, amniotic membrane graft. Changes in astigmatism were significantly more with amniotic membrane graft and conjunctival autograft technique as compared to the bare sclera technique, mainly due to better healing and less granulation tissue formation.9 Complications are known to occur in every ophthalmic surgery. In our study, out of 100 patients, only 16 patients had complications over the 3 month follow up period. The most frequently observed complication was subconjunctival hemorrhage (6 patients) which was managed by oral Vitamin C supplementation and it subsided in all patients by post-operative day 14. This was followed by graft displacement (3 patients) on post-operative day 1 and the patients underwent graft re-suturing. 2 patients had chemosis and 2 had lid edema on post-operative day 1. These patients were treated with topical Flurbiprofen 0.003% eyedrops and increasing the dose frequency of topical steroid+antibiotic combination and was cured by post-operative day 3. One patient developed conjunctival cyst at 3 months who was subjected to cyst excision at 3 months and one patient developed Dellen ulcer at 3 months. 1 patient developed scleral thinning which presented at 6 weeks follow-up who was managed by multi-layered amniotic membrane grafting and suturing with 10-0 Ethilon. Recurrence after pterygium surgery is a quite common phenomenon. Okoye et al. in their study with 30 eyes pterygium treated with surgery and amniotic membrane grafting had a recurrence rate of 6%.10 In a study conducted by Katircioglu et al., percentages of recurrence seen in groups of conjunctival autograft, amniotic membrane grafting and conjunctival autograft with adjuvant mitomycin C were 16%, 25% and 0% respectively.11 Luaratanakorn etal in his study observed that the recurrence rate was 12.3%, 21.4% and 13.1% for primary, recurrent and all pterygia, respectively in patients with conjunctival autograft. In the amniotic membrane group, the recurrence rate was 25.0%, 52.6% and 28.1% for primary, recurrent and all pterygia.12 However in our study, a longer follow-up is required for better evaluation of long term complication and recurrence. Although the recurrence was lower in conjunctival autograft, amniotic membrane grafting serves to be good alternative to it especially in cases with large defects, double pterygium or in cases where bulbar conjunctiva is required for future glaucoma filtration surgery. However, the use of amniotic membrane is limited by its high cost. Moreover, recurrence can be reduced by adjuvants like Mitomycin C. Using amniotic membrane reduces surgical time of harvesting the conjunctival autograft and using fibrin glue along with it, decreases further.
CONCLUSION Our study suggests that early excision of pterygium with amniotic membrane grafting should be employed in all cases of pterygium as early as possible as it is safe, highly effective modality in the management of primary pterygium as it also reduces recurrence. However, a longer follow up is required for documentation of recurrence.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home