|
Table of Content - Volume 14 Issue 1 - April 2020
A study of ocular manifestations of head injury
Harish Shetty
Associate Professor, Department of Ophthalmology, Karwar Institute of Medical Sciences, Karwar, INDIA. Email: doc.hari12@gmail.com
Abstract Background: The leading cause of blindness in the world is due to the trauma. In fact, more than half a million people worldwide is directly or indirectly affected by it and this is the cause for partial loss of sight in many more and it is often the leading cause of unilateral loss of vision particularly in developing countries. Keywords: Blindness, Head Injury, Brain, Cross-section
INTRODUCTION The leading cause of blindness in the world is due to the trauma. In fact, more than half a million people worldwide is directly or indirectly affected by it and this is the cause for partial loss of sight in many more and it is often the leading cause of unilateral loss of vision particularly in developing countries.1 Brain injury mainly if it is traumatic in nature is a critical and most important burdening factor that is faced by the whole world. Majority of the cases will be lifelong morbid or even death can occur especially among young adults2 . Lifelong morbidity, disability and mortality ultimately are known to occur in those who survive. In India, it is estimated that nearly 15 to 20 lakh people annually are injured and around 10 lakh people succumb to death every year.3 The incidence of TBI as measured by combined emergency department visits, hospitalisations and death has steadily risen from 2001- 2010. Data from CDC indicate that each year in USA, 1.7 million sustain TBI.4 From 2001 to 2010, TBI rates increased from 521 to 824/per 1,00,000 population (CDC 2014). Between 3.2 and 5.3 million5 persons (1.1%-1.7% of US population) live with long-term disability from TBI and in European Union approximately 7.7 million6 people who have experienced TBI have disabilities and about 30-50% of these are associated with ocular and visual defects, which is an approximate estimate.7 This study is to put an effort to find the incidence of Ocular Manifestations of Head Injury.
AIMS AND OBJECTIVE To find the incidence of Ocular Manifestations of Head Injury.
MATERIALS AND METHODS This study was done in the Department of Ophthalmology, Karwar Institute of Medical Sciences. This study was done from August 2019 to Jan 20. This study was done by observing 30 patients that we treated in the Department. Inclusion Criteria: Patients below 16 years Exclusion Criteria: Past ocular pathology. Patients on immunosuppressant and anticancer treatment.
RESULTS
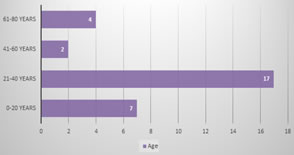
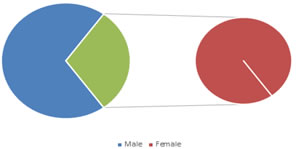
Figure 2: Sex Distribution Table 1: Mode
Table 2: Lesions
Table 3: Ocular Complications
DISCUSSION The role of ocular injuries secondary to head trauma in the causation of blindness has become a subject of immense importance. TBI leads to neurocognitive deficits such as impaired attention, inability to perform visuospatial associations and psychological health issues. TBI is considered a silent epidemic as society is unaware of magnitude of the problem. The manifestations of head injury and its numerous other systemic complications are so compelling that damage to the visual system is most likely to be ignored. Many a times, when the eye is examined as part of neurological assessment of a patient with head injury, the purpose is mainly to gauge the severity of the head injury itself. Many hypotheses have been advanced to explain the cause of head injuries, but most of these hypotheses have remained untested and unproven. With respect to soft tissue injuries to the globe and adnexa in the anterior segment of the eye, one hypothesis suggested that energy is transferred to these structures from the sturdy frontal bones to the orbit and from the lateral orbital margin to contiguous facial structures during the impact following head injury. Disorders of eye movement are thought to result from direct trauma to orbital contents, cranial nerves and other brain areas. In spite of the significance of problems associated with ocular manifestations of head injury, only few reviews of the whole spectrum are available in the literature. The aim of this study was to evaluate the clinical profile of ocular and visual complications in patients hospitalised and managed for head injury at our hospital. The first and the second decade of life ocular trauma forms about 20–50% of all eye injuries approximately 8–14% of total injuries in children below 10 years of age. Forty to sixty thousand of eye injuries lead to visual loss. Despite its public health importance, there is relatively less population-based data on the magnitude and risk factors for ocular trauma, especially from developing countries. Trauma to the eye and ensuing visual disability is an important cause of preventable monocular blindness in the paediatric age group in India. The ensuing visual disability has significant emotional, psychological, and Socioeconomically impact on the individual person, family, and to the society as a whole. Policy decisions helpful in preventing this kind of trauma and improving the required trauma management services warrant an accurate estimate of the pattern of the ocular trauma in Indian population. Most of our understanding of this issue is based on the studies from developed countries
CONCLUSION This study is successful in focusing a light on the different ocular manifestations of the head injury. The diagnosis should be prompt and the treatment should be precise and prompt.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home