|
Table of Content - Volume 16 Issue 1 - October 2020
Visual outcome of management in traumatic cataract cases: A cross sectional study at tertiary care hospital
Sailesh S Katare1*, Nandakumar B Dole2, U S Mohite3
1Junior Resident1, 2Associate Professor, 3Professor & HOD, Department of Ophthalmology, Government Medical College, Latur, INDIA.
Abstract Background: The development of cataract is known complication following blunt or penetrating trauma to eye. With improved technology and increasing advantages of intraocular lenses the time has come when IOL can be used after the extraction of traumatic lens. Aim and objective: To assess the visual outcome following management of traumatic cataract. Methodology: This was a prospective study of 40 cases of traumatic cataract most of which were managed with lens extraction with IOL implantation. Visual acuity was assessed with snellens chart at 6 weeks postoperatively Results and discussion: Majority of the cases were seen in the age group of 21-40 years (55 %) with a Male predominance (72.5 %). Penetrating injury in 29 cases (72.5%) followed by blunt trauma in 11 cases (27.5%), penetrating injury was seen more in people of rural area, working in fields. SICS with PCIOL implantation was performed in 36 cases (90 %). Around 50 % of the eyes gained vision post-operatively more than 6/18.
INTRODUCTION Cataract remains the commonest cause of blindness in India contributing about 81%. The incidence of ocular injuries in India is estimated to be 20.5% with 75% cases occurring among those aged less than 40 years. Males are predominantly affected than females with a male to female ratio of 9:1. Further ocular trauma is a major cause of monocular blindness and visual impairment throughout the world, although little is known about its epidemiology or associated visual outcome in developing countries. 1 Cataract is the commonest complication following ocular injury. 2 Traumatic cataract results most commonly from either penetrating injuries from sharp objects like stick or thorn with direct injury to lens or through blunt trauma by objects like stone, cricket ball etc. Rarely, it can occur from electrical shock, ionizing radiation or infra-red rays (glass blower’s cataract). 3 Traumatic cataract following a perforating injury may be localized cataract, rosette cataract , intumescent cataract or lacerated cataract. Blunt trauma leads to concussion type of cataract due to coup or countercoup ocular injury. The lenticular opacity may be vossius ring, localized or diffuse type. 4-7 The pathophysiology of traumatic cataract is believed to involve direct rupture of capsule or coup, countercoup and equatorial expansion due to hydraulic forces transferring the energy of trauma to the opposite side of the eye. It can be accompanied by anterior and posterior segment abnormalities depending on the force of trauma and depth of globe penetration. 8,9 Traumatic cataract is a special clinical type since it is commonly seen in young individuals and in children. By causing severe visual impairment it leads to reduced productivity due to loss of manpower and in children it may lead to loss of binocular single vision if neglected. Since traumatic cataract causes significant visual impairment in younger population, it is necessary to evaluate the damages caused by it and manage it with timely intervention to restore the vision at the earliest. Traumatic cataract poses a significant medical and surgical challenge to an ophthalmologist. A detailed history, careful examination and a clear management plan can simplify these cases and provide the best possible visual outcome. 10,11 The methods used to evaluate the visual outcome in eyes managed for traumatic cataracts and senile cataracts are similar 12 but the damage to other ocular tissues due to trauma may compromise the visual gain in eyes operated on for traumatic cataracts. Post-operative inflammation is a common complication following traumatic cataracts, hampering visual outcome. Other complications leading to decreased post-operative vision are corneal scar, uveitis, secondary glaucoma, pupillary capture, posterior capsular opacification and retinal scar. 13 The management of such cases is an important problem in ophthalmology and prognosis is variable. Extent of associated damage to anterior and posterior segment, time of intervention, operative and post- operative complications go a long way in determining the ultimate prognosis. The type of trauma, extent of lenticular involvement and associated secondary rise of intraocular pressure are factors of paramount importance which could dictate the exact time of management of traumatic cataract. Thus this study has been undertaken to assess the visual outcome following management of traumatic cataract. Aim and objective: To assess the visual outcome following management of traumatic cataract.
MATERIAL AND METHODS Present study was a cross sectional study carried out in Ophthalmology outpatient Department of a tertiary care centre during December 2017 to June 2018. Study population was all the patients presenting with cataract. Inclusion criteria:
Exclusion criteria:
Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. With reference to study done by Doutetien et.al (2008) sample size is calculated as below: n= 4pq/L2, n= 4 x 6.9 x 93.1 /1.38 x 1.38, n= 1349 Total 2136 were cataract patients were examined among which 47 traumatic cataract cases were identified. 40 cases from these cases of traumatic cataract were included for this study as the remaining patients did not fulfill the inclusion criteria. All 40 cases were evaluated, with respect to a detailed history, regarding type of trauma, duration between trauma and presentation, associated ocular injury, intra- operative and post-operative complications. The visual prognosis after surgery was noted. All patients with traumatic cataract presenting at the tertiary care centre fulfilling sampling criteria were selected for surgery. Detailed Systemic examination was done. Each patient was subjected to detailed examination and investigation needed. Routine blood analysis Lacrimal syringing, Intraocular pressure assessment were done. Radiological investigation, B-scan ultrasonography to rule out intraocular foreign body, vitreous hemorrhage, RD. Ocular examination included Torch light examination, slit lamp biomicroscopic examination and indirect ophthalmoscopy. Preoperative visual acuity was recorded in both eyes. Keratometry and A-scan biometry was done for intraocular power calculation, but in case of corneal scarring the power of other eye was calculated. Topical antibiotics and NSAIDS were administered hourly the day before surgery. Antiglaucoma medication was given in cases associated with raised IOP. Pupil was dilated with 0.5% tropicamide with 10% phenylephrine until full dilatation was attained. In cases associated with inflammation it was controlled with topical steroids and antibiotics before surgery. Peribulbar block was given which consisted of a mixture of 2% lignocaine with adrenaline with hyluronidase 10 units per ml. All cases were operated under operating microscope with co- axial illumination. Eye was painted and draped. Superior rectus bridles suture was taken. Fornix based conjunctival flap was raised. A 6.5-7.00 mm partial thickness sclerocorneal tunnel was made. Side port entry was made. CCC was done. Hydro dissection was done where required. Nucleas was prolapsed in AC where possible and was expressed with viscoelastics, where it was imbibed lens matter it was directly aspirated. Epinucleas and residual cortex was aspirated with simcoe cannula. A 6mm optic single piece PMMA lens was placed in the bag, sulcus as per the case. Wound hydration was done and wound was checked for its apposition. Subconjunctival injection dexamethasone and gentamycin was given and eye was padded and bandaged. Post operatively, Systemic analgesics were administered along with systemic antibiotics. Next morning eye was examined under slit lamp to look for any postoperative complications. Patients were started on topical antibiotic steroids, NSAIDS and mydriatics eye drops. Antiglaucoma medications were given in selected cases. Patients were discharged with postoperative instructions regarding the medications and other measures. Patient were instructed to come for follow-up after 1 week and after 6 weeks. Visual acuity was assessed with snellens chart at each postoperative visit along with slit lamp examination. Antibiotic steroid drops were gradually tapered. Refraction was done at 6th weeks postoperatively and glasses were prescribed based on patients refractive status. The clinical data of each patient was collected in the proforma for analysis of the study. Data was analysed with SPSS version 22.
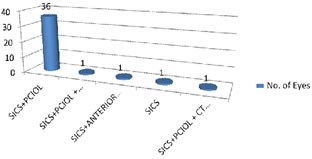
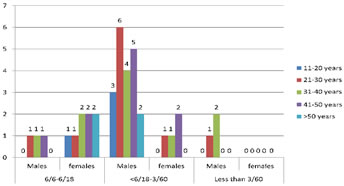
RESULTS A total of 29772 patients presented to ophthalmology department over a period of one and half years. Out of these 2136 (7.17 %) were cataract patients. Traumatic cataract accounted for 47 of these cases. 40 cases from these cases of traumatic cataract were included in this study as the remaining patients did not fulfill the inclusion criteria. Thus prevalence of traumatic cataract was 2.2% among the cataract patients attending the OPD and 0.15% among all patients attending OPD. The age group ranged from 17-61 years. More number of cases were found in the age group of 21-40 years (55%). Out of 40 cases, 28 were males and 12 were females. The male-female ratio is 2.33:1. (table 1) Out of 40 cases of traumatic cataract, 21 were caused by stick or thorn, 6 were caused by stone particles, 9 were caused by metallic particles, 1 was caused by Ball, 1 was caused by plastic wire and 1 was caused by glass piece and 1 was caused by forceful water jet. (table 2) Analyzing the type of cataract, it was found that 36 cases had total cataract, 2 of the cases had white soft cataract, 1 case had rosette cataract and 1 case was found to be of anterior subcapsular cataract. ````Pre-operative visual acuity was recorded in all cases. In 15 cases (37.5 %), the preoperative visual acuity was PL/PR. In 17 cases (42.5 %), the preoperative visual acuity was perception of hand movements. In 8 cases (20 %), the preoperative visual acuity was 3/60 to counting fingers ½ meters. Visual acuity of the uninjured eye was recorded in all the patients and was found to be within the normal limit. (table 3) Out of 40 cases of traumatic cataract, 5 (12.5 %) cases presented with uveitis , 8 (20 %) cases presented with lens matter in AC, 4(10%) presented with secondary glaucoma. Out of 40 cases of traumatic cataract, 36 cases underwent ECCE (Small Incision Cataract Surgery) with PCIOL implantation, 1 case underwent small incision cataract surgery with PCIOL implantation with corneal tear repair, 1 case underwent small incision cataract surgery with PCIOL implantation with anterior vitrectomy, 1 case underwent small incision cataract surgery with aphakia. (fig 1) Final visual acuity (best corrected visual acuity) was checked at the end of 6 weeks. Two cases lost for follow up in the study. The final visual acuity was graded into three categories based on ‘WHO Vision Categories’ Vision of < 3/60 as blind, Vision of 3/60 < 6/18 visually impaired (Low vision), 6/18 and above as adequate vision. In these 40 cases of traumatic cataract, none of the patients were managed conservatively as all these patients had significant cataract which was responsible for reduced vision mainly and other complications like uveitis (12.5 %) and secondary glaucoma (10 %). Associated uveitis was adequately controlled before surgery with antibiotic steroid drops given 6-8 times per day. A total of 36 patients underwent cataract extraction with PCIOL implantation .In 2 patient with major vitreous loss and zonular weakness were kept aphakic after SICS. In 2 patients anterior vitrectomy was done along with SICS. In 1 case corneal tear repair was done along with SICS. Out of 38 cases, final visual acuity of 6/6 to 6/18 was seen in 11 (29 %) cases in which 3 ( 8 %) were males and 8 (21%) were females. Final visual acuity of less than 6/18 to 6/60 was seen in 24 patients (63 %) which included 20 (52%) males and 4 (11 %) females. Three male patients (8 %) had visual acuity less than 3/60. (fig 2)
Table 1: Distribution of traumatic Cataract patients according to age and sex
Table 2: Distribution of traumatic Cataract patients according to type of trauma
Table 3: Distribution of traumatic Cataract patients according to pre operative visual acuity
Figure 1: Distribution of traumatic Cataract patients according to type of surgery
Table 4: Distribution of traumatic Cataract according to final visual acuity
Figure 2: Age and sex wise final visual acuity
DISCUSSION Age wise analysis showed that majority of cases occurred in younger age group (21-40). This is because of the greater involvement in outdoor activity and recreational activity and work pattern of people. Most injuries resulted from stick followed by metal. Other studies also showed an increased incidence of traumatic cataract in younger age group. Daljit Singh showed similar age group distribution. 14 This study showed a male preponderance (72.5 %). This is because men are more exposed to ocular trauma because of occupation and they are from age earning group. The study found that most of the cases i.e. 23 (57.5 %) were caused by stick and metal. This is because of the rural people who are working in fields. The type of injury was mostly of penetrating type. Nine cases (22.5%) with metallic particles and 7 cases (17.5 %) with thorn and 6 cases (15 %) with stone. These were seen in people working in farming and road construction works. One cases injury was caused by cricket ball, one case injury was caused by glass piece and one case was caused by forceful trauma by water jet at vehicle washing centre seen in young individuals engaged in recreational activity. Krishnamachary M also found that most of the injuries i.e., 54.7% were caused by stick or bow and arrow. 15 The preoperative visual acuity in this series of study is as follows, 15 (37.5 %) of the eyes had PL and PR only. 17 (42.5 %) of eyes had perception of hand movements and 8 cases (20 %) had 3/60 to counting fingers ½ meters. In the studies conducted by Renuka and Srinivasan et al. and Krishnamachary M, the preoperative visual acuity was less than 6/60 to PL and PR in most of their cases. 15, 16 Out of 40 cases which were followed up after 6 weeks, in 11 cases (29 %) final visual outcome was 6/18 and above and in 24 cases (63 %) final visual outcome was between 6/18-3/60. The main cause for the impaired vision in this study was due to corneal scars and opacity obstructing the visual axis and causing irregular astigmatism. In 3 cases (8%) visual acuity was less than 3/60. In one case patient had developed a traumatic vitreous hemorrhage which resolved minimally and patient had poor vision. In the other 2 cases there was significant vitreous loss and weak zonular support were kept aphakic resulted in poor visual outcome. Marcus Blum reported good visual outcome of 90%. 17 Daljit Singh reported 70%. Renuka Srinivasan noted 88.2% of visual outcome. 14,16 This study of 40 cases of traumatic cataract almost all of which were managed by cataract extraction with IOL implantation showed moderate visual outcome of 50% in comparison with other studies
CONCLUSION With improved technology and increasing advantages of IOL implantation, around 50 % of the eyes gained vision post-operatively more than 6/18.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home