|
Table of Content - Volume 17 Issue 3 - March 2021
An observational study of the prevalence of dry eye disease with previous 10 years literature review
Merlin Saldanha1, Sanjiv Agrawal2, Anjana Mirajkar3*
1Associate Consultant, Retina and Uveitis Services, Kenia Eye Hospital, Mumbai, Maharashtra, INDIA 2Associate Professor, 3Senior Resident, Department of Ophthalmology, Bharati Vidyapeeth Medical College, Pune, Maharashtra, INDIA. Email: anje7777@gmail.com
Abstract Background: We conducted this study to know the prevalence of dry eye, to determine the association among the subjective and objective tests and to monitor the effects of the current treatment for dry eyes during the follow-up period of 12 months. Methods: The prospective observational study was conducted at a tertiary care hospital setting from December 2012 to May 2014. A total of 250 patients aged ≥ 18 years with dry eyes symptoms were included. An OSDI questionnaire was administered to all participants to assess the symptoms of dry eye which was correlated with tear film break up time(TBUT), Schirmer’s test, Lissamine staining and Fluorescein staining. All the individual patients were treated for the DED and were followed up for 12 weeks. Results: Among 250 subjects, DED was present in 148(59.2%) patients. There was a significant association of OSDI scores with Schirmer's test, TBUT, Tear meniscus height, Lissamine staining, and Fluorescein staining. There was a significant association of OSDI with DED increasing severity (P<.0001) During the follow up period of treatment, there was a significant improvement in the median OSDI scores at 12 weeks in comparison to the baseline (20.8 vs 25, p<.0001) Conclusion: The study found the prevalence of DED to be 59.2%. The diagnosis of DED can rely on both subjective and objective tests. With an early diagnosis and initiation of the treatment, significant improvement in the symptoms can be achieved within 3 months of follow up. Key Words: Dry eye disease, prevalence, OSDI score, objective tests, treatment.
INTRODUCTION Dry eye is a common disease with current prevalence of 9.5% to 90% in world and 18.4% to 54.3% in India. Its prevalence was 29.25% in 2010 which increased to 46.71% in 2016 and 54.3% in the current period.2 It manifests as a plethora of symptoms including pain, tearing, foreign body sensation, burning, blurred vision, grittiness, stinging sensation, and photophobia.2 It’s etiology may include Sjögren syndrome, lacrimal deficiency, lacrimal gland duct obstruction, reflex block, systemic drugs, meibomian oil deficiency, disorders of lid aperture, low blink rate, vitamin A deficiency, topical drugs preservatives, contact lens wear, and ocular surface diseases such as allergy.5 The significant associated factors for DED includes age, gender, occupation, residence, environmental factors including reduced relative humidity and extreme temperature, use of video display terminals (VDT), smoking, alcohol intake, contact lens wear, refractive surgery like LASIK, intake of medications like antihistamines, β-blockers, and oral contraceptives, as well as anxiety disorders, sleep disorders, and depression.i Recently its incidence among diabetics has also been explored which suggested the risk factors to be duration of diabetes mellitus, gender, old age, diabetic retinopathy, higher blood glucose, and higher levels of glycosylated hemoglobin HbA1c.6,7,8 The diagnosis of dry eyes involve objective (OSDI score) and subjective tests (Schirmers, TBUT, fluorescein staining) which have been found to be successful in the evaluation and monitoring. The association seen among the objective and subjective results further enhance the use of both of them to arrive at a definite conclusion.1,2,9 The continuous changing trends of prevalence of dry eyes makes it essential to monitor the prevalence and changing trends over the last decade which may help understand the mechanism and the effect of ongoing prevention and therapeutic measures. Thus we conducted this study to know the prevalence of dry eye, to determine the association among the subjective and objective tests and to monitor the effects of the current treatment for dry eyes during the follow-up period of 12 months.
METHODS The prospective observational study was conducted at the Department of Ophthalmology in a tertiary care hospital setting from December 2012 to May 2014. Approval for conducting study was taken from Ethics Review Committee of the hospital. An informed consent was obtained from the individuals. The sample size was calculated on the basis of the study by Rege A, et al.10 who observed that prevalence of dry eye disease was 16.4%. Taking this value as reference, the minimum required sample size with 5% margin of error and 5% level of significance is 211 patients. To reduce margin of error, total sample size taken is 250. A total of 250 patients aged ≥ 18 years with dry eyes who presented with symptoms such as burning sensation, sandy grity feeling, foreign body reaction, photophobia, and heavy lids were included. Patients with history of alkali burns, trachoma, ocular trauma, chronic uveitis, glaucoma, increased mucoid discharge and watery secretion suggestive of vernal keratoconjunctivitis, and ocular surgery within the last 6 months; those with acute ocular infection, corneal opacity or degeneration, impaired eyelid function such as in Bell’s palsy, nocturnal lagophthalmos, ectropion, and contact lens users were excluded from the study. Demographic characteristics of all patients were noted. An OSDI questionnaire was administered to all participants to assess the symptoms of dry eye. OSDI scale was included for subjective evaluation, so as to have a better subjective picture of the symptom in relation to its effect on the quality of life. A complete slit-lamp examination of the lid margins, tear meniscus, conjunctiva, cornea and tear film was done. Relevant examination of other important ocular structures was done. After this, the following tests were reformed to diagnose dry eye: tear film break up time(TBUT), Schirmer’s test, Lissamine staining and Fluorescein staining.
Standards of testing The TBUT is the time in seconds between the last blink and the appearance of the dry spot. The patient was seated at the slit lamp. After instilling a drop of 2% fluorescein into the right eye, the patient was asked to blink a few times before examination. The Break-up time of ≤10 seconds was considered positive, indicative of dry eye. Greater than 10 seconds was considered negative.11 Schirmer’s test was done using 5×35 mm sterile strips of Whatman No.41 filter paper. Measurements of ≤10mm were considered to be positive. and > 10 mm were considered as negative.11 Lissamine staining is a measure of assessing ocular surface damage using the Lissamine dye. One drop of antibiotic solution was put on a sterile, commercially available Lissamine strip. After 15 seconds, this eye was examined for staining of cornea and conjunctiva. The amount of staining in six areas of eye was then recorded and graded based on modified Van Bijsterveld rose bengal grading map. A quantitative scale of 0 to 3 was used in each area of the conjunctiva of each eye. An additive score of total 4 or more in the eye constituted a positive test. Fluorescein staining: 1-2% Na fluorescein solution was used to stain the tear film and was graded as per the standard scale of reporting. Statistical analysis Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected then non parametric test was used. Statistical tests were applied as follows-
A p value of <0.05 was considered statistically significant. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
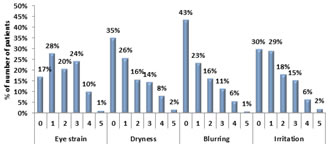
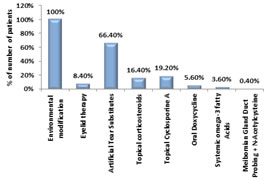
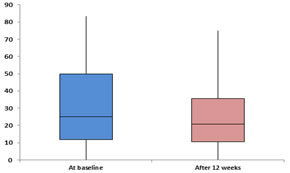
RESULTS Amongst our study on 250 subjects, DED was present in 148(59.2%) patients. The sociodemographic characteristics are shown in Table 1. The median age of the patients with DED was 41 years. Compared to those without DED, patients with DED had comparable median age (years) (41 vs 46.5, P=0.422) and comparable number of females (57.48% vs 42.52%) and males (60.98% vs 39.02%) (P=0.574). The common symptoms noted among the study patients were eye strain, dryness, blurring and irritation. The grading of the individual symptoms has been shown in Figure 1. OSDI score was 0 to 33 in majority of the patients (62.80%), 34 to 66 in 18.80% patients, and 67 to 100 in 18.40% patients. In most of the patients (26.40%), dry eye severity level was 2, followed by level 1 in 20.00% patients, level 3 in 11.20% patients, and level 4 in 1.60% patients. We found significant association between Schirmer’s test and OSDI score. Among 81 patients with Schirmer’s score <=10, 53.09% had high OSDI scores (>=67) and among 169 patients with Schirmer’s score >10, 98.22% had low OSDI scores (p<0.0001). We found significant association between TBUT test and OSDI score. Among 146 patients with TBUT score <=10, 68.49% had low OSDI scores (<67) and among 104 patients with TBUT score >10, 100% had low OSDI scores (p<0.0001). We found significant association between tear meniscus height and OSDI score. Among 52 patients with tear meniscus height <1, 76.92% had high OSDI scores (>=67) and among 198 patients with tear meniscus height >=1, 96.97% had low OSDI scores (p<0.0001). We found no significant association between blink rate and OSDI score. Among 219 patients with blink rate <10, 81.28% had low OSDI scores (<67) and among 31 patients with blink rate >=10, 83.87% had low OSDI scores (p=0.727). We found significant association between Lissamine staining - van Bijsterveld score and OSDI score. Among 167 patients with Lissamine staining - van Bijsterveld score <4, 95.81% had low OSDI scores (<67) and among 83 patients with Lissamine staining - van Bijsterveld score >=4, 53.01% had low OSDI scores (p<0.0001). We found significant association between Fluorescein staining and OSDI score. Among 168 patients with negative Fluorescein staining, 95.83% had low OSDI scores (<67) and among 82 patients with positive Fluorescein staining, 52.44% had low OSDI scores (p<0.0001). We found significant association between Mebomial gland disease and OSDI score. Among 228 patients without Mebomial gland disease, 85.09% had low OSDI scores (<67) and among 22 patients with Mebomial gland disease, 54.55% had high OSDI scores (>=67) (p<0.0001) (Table 2) We found a significant association between severity of DED and OSDI score. Among 102 patients with severity level 0 and 50 patients with severity level 1, 0% had high OSDI scores (≥67) whereas among 66 cases of level 2, 22.73% had high OSDI scores (≥67). Among the cases with severity level 3 and 4, 96.43% and 100% had high OSDI scores (≥67) (p<0.0001) (Table 3). The treatment approach encompassed a variety of modalities. Environmental modification was done in all patients. Artificial tear substitutes were provided to 66.40% patients, followed by topical cyclosporine A in 19.20%, topical corticosteroids in 16.40%, eyelid therapy in 8.40%, oral doxycycline in 5.60%, and systemic omega-3 fatty acids in 3.60% patients (Figure 2). During the follow up period of treatment, there was a significant improvement in the median OSDI scores at 12 weeks in comparison to the baseline (20.8 vs 25, p<.0001) (Figure 3). In addition, during the follow up period, there was a reduction in the severity level of the DED but statistically it was not significant. At baseline and 12 weeks, dry eye severity level 0 was comparable (40.80% vs 44%), level 1 was similar (20% vs 26.80%), level 2 was similar (26.40% vs 22%), level 3 was comparable (11.20% vs 6.80%), and level 4 was comparable (1.60% vs 0.40%) (p=0.082 for all) (Table 4).
DISCUSSION Dry eye as any other eye disease causes eye irritation and affects the quality of life. The prevalence of dry eye in the current study was found to be 59.2%. The trends in the prevalence rate over the last 10 years (worldwide and India) have been shown in Table 1 and 2.
Worldwide
India
The age and gender distribution of DED may show variation amongst previous studies depending on the age group studied. In the index study, the dry eye disease (DED) commonly affected the age group of 31–40 years with mean age of 43.24 years which was in line with the mean age of 45.24 years as reported by Shanti Y et al.1 Instead, Chavhan et al.27reported a mean age of 54.4 years, which is higher than that reported in our study. The gender distribution showed DED to be present in nearly equal number of males and females (P>0.05) in the index study. Similar findings were reported by Donthineni et al.,9 However, Titiyal et al.,2reported higher male prevalence (65.3%) and Chavhan et al.27 reported higher female prevalence; but in both the studies, the statistical difference was not significant as seen in the index study. DED is a symptomatic disease affecting quality of life (QOL) of the patients. Its assessment includes a plethora of tests. According to the 2017 International Dry Eye Workshop II (DEWS) and Asia Dry Eye Society (ADES) reports, determination of the necessity of tear film for healthy ocular surface and identification of tear film instability as key factors in diagnosis of DED generated attention toward stabilization of tear film layer, resulting in the development of strategy of “tear-film oriented therapy”.7 The index study conducted various diagnostic tests and there existed a significant association of OSDI scores with Schirmer's test, TBUT, Tear meniscus height, Lissamine staining-van Bijsterveld score, Fluorescein staining, and Mebomial gland disease. Also there was a significant association of OSDI with DED increasing severity (P<.0001) The findings were supported in studies by Baisoya et al.,4 Li J et al.29 and Basak et al.23 who found a significant association between OSDI and objective tests. This association suggests that objective dry eye tests can be useful in establishing a diagnosis of dry eye syndrome and for assessing the effects of treatments or the grade of disease severity. DED is characterized by tear film instability, hyperosmolarity, chronic inflammation as well as neurosensory abnormalities resulting in ocular surface damage. DED causes unstable tear film in the open-eye state that causes several corneal and conjunctival epithelial disturbances and also decreases corneal sensitivity to mechanical stimulation. DED impacts not only vision, but also has an impact on the quality of life (QOL) as it result in low vitality, pain, role limitations, and poor general health.9 To decrease the symptoms and improve the QOL, the patients in the study were treated with artificial tear substitutes, topical cyclosporine A, topical corticosteroids, eyelid therapy, oral doxycycline, and systemic omega-3 fatty acids, and environmental modification, and among them the DED severity of 5.6% patients decreased from severity of 3/4 to 0/1. The OSDI scores were found to significantly decrease in the follow-up period from 25 at baseline to 20.8 at 12 weeks.(p<0.05) Similarly, in study by Kim Y et al.,30significant improvement in OSDI score was observed at 1 month and 3 months after treatment with oral hyaluronic acid. Connor CG et al.31 also reported decrease in OSDI score after treating dry eye disease with 5% testosterone cream twice a day. The current study used plethora of treatments to provide a holistic approach to the patients because the clinical manifestations of DED are variable, and so the treatment of each patient should be based on targeting the specific mechanisms involved in the disease. The latest options available for treatment of DED are anti-inflammatory therapy, scleral contact lenses, and meibomian gland heating and expression.32 One of the limitations of study was that it was a hospital-based study, so inherented bias may be associated with it. Another limitation is that the postrefractive surgery patients, contact lens wearers, and patients with severe conjunctival as well as corneal disease were excluded from the study, which may lead to underestimation of the actual prevalence of DED.
CONCLUSION Prevalence of dry eye in our study was 59.2%, which suggests that dry eye is an underdiagnosed disease in India. The age group of 31–40 years was most commonly affected. A significant improvement was noted in the OSDI scores after follow-up at 12 weeks. Evaluation of DED with standard tests helps in diagnosis and treatment.
Table 1: Distribution of DED by age group and gender
Table 2:- Association of dry eye symptoms with OSDI score.
Table 3: Association of severity of dry eye disease with OSDI score
Figure 1: Distribution of grade of symptoms of study subjects Figure 2: Distribution of cases according to treatment
Figure 3: Comparison of OSDI at baseline and 12 weeks follow-up among the cases
Table 4: Comparison of dry eye severity level at baseline and 12 weeks follow-up among the cases
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home