|
Table of Content - Volume 17 Issue 3 - March 2021
Study of safety and effectiveness of subtenon’s anesthesia versus peribulbar anesthesia in cataract surgeries
Gajanan D Channashetti1*, Smita S Kottagi2
{1Associate Professor, Department of Ophthalmology} {2Assistant Professor, Department of Biochemistry} Gadag Institute of Medical Sciences, Gadag, Karnataka, INDIA. Email: drgajudc@gmail.com
Abstract Background: To compare the safety and effectiveness of subtenon’s anesthesia verusus peribulbar anesthesia in small incision cataract surgeries done at Gadag Institute of Medical Sciences, Gadag, Karnataka. Methodology: It is a hospital based study of 150 patients out of which 75 patients underwent small incision cataract surgery under subtenon's anesthesia and 75 patients under peribulbar anesthesia. Sub conjunctival hemorraghe, chemosis, Akinesia and analgesia was graded on a subjective scale and recorded. Effect of anesthesia on IOP was studied. Results: Subtenon's anesthesia was less painful on administration and provided adequate analgesia and akinesia comparable to Peribulbar anesthesia without any complications. Conclusion: Subtenon's anesthesia is a safe technique to deliver local anesthesia providing equally good analgesia and akinesia to Peribulbar anesthesia. It is a safe alternative to Peribulbar anesthesia in manual small incision cataract surgery. Keywords: Subtenon's anesthesia , Peribulbar anesthesia.
INTRODUCTION In the past various types of anesthesia were successfully used for cataract surgeries with many disadvantages and complications associated with them. Advances in cataract surgical techniques have decreased the traditional universal demand for total akinetic anesthesia, while the safety and analgesia are still the required entities. Among regional anesthesia retrobulbar anesthesia, peribulbar anesthesia, perilimbal anesthesia, subtenon's anesthesia and topical anesthesia have been used with many advantages and disadvantages. Retrobulbar anesthesia which was used for almost a century was associated with a number of potential complications like chemosis, retrobulbar hemorrhage, globe perforation, extra-ocular muscle malfunction, optic nerve injury, and brain stem anesthesia. Peribulbar anesthesia while providing excellent analgesia and akinesia and comparatively safer than retrobulbar anesthesia still has been associated with complications like chemosis, extra ocular muscle malfunction, increased intraocular pressure, orbital hemorrhage, globe perforations and ptosis. Subtenon’s anesthesia was first described in 1956, and gained popularity since 1990. Subtenon’s anesthesia has emerged as a safer and effective method of anesthesia without complications of sharp needle injection’s like extra ocular muscle malfunction, increased IOP, orbital hemorrhage, globe perforations and ptosis. Topical anesthesia of cornea and conjunctiva has been recently used with success in latest surgeries like phacoemulsification where absolute demand for akinesia is not needed. Currently there are no criteria’s as to optimal approach to regional anesthesia, and the choice of local anesthetic technique, is largely determined by surgeon’s preference. So a study needs to be done to compare the safety and effectiveness of subtenon’s anesthesia and peribulbar anesthesia in cataract surgery. VARIOUS METHODS OF GIVING PERIBULBAR AND SUBTEON’S BLOCK. PERIBULBAR: volume varies from 3 to 10 ml. initial injection is at inferotemporal lower orbital margin midway between lateral canthus and lateral limbus. 5 ml is injected at a depth of 2.5 cm from inferior orbital rim. After 5 min amount of akinesia is accessed, and often a second injection is required to block the superior oblique. A 25 gauge needle is inserted between medial canthus and curuncle. At depth of 1.5cm, and 3ml anesthetic is injected.1 PERIBULBAR BLOCK GIVEN INFERO-TEMPORALY Figure 1: The needle is placed in the etraconal compartment (peribulbar block) through the inferotemporal area.
SUBTENON’S BLOCK Technique where after administering 4 % topical PARACAINE, at the supernasal quadrant approximately 3 mm from the limbus, a small nick incision was made with blunt scissors in conjunctiva and tenon’s until bare sclera was exposed. The scissors were then passed through nick to create a path in tenon’s capsule and intermuscular septal fascia. A blunt 19 gauge cannula was inserted and glided along the path posteriorly following contour of globe at a distance of 1.5 to 2 cm after which 2 ml of lignocaine 2 % without adrenaline was used. 22
SUBTENON’S BLOCK INFERO-NASALY Figure 2: A sub-tenon cannula is inserted into the su- tenon’s space
METHODOLOGY METHOD OF COLLECTION OF DATA:- Sample size: cataract surgery rate in India is 3400 per million per year. 9 It is 0.34 per 100 population = 0.34 % with prevalence 0.34% and allowable error 30% the calculated sample size is =143. Using statistical formula23:- n = 4pq/ L2 , P = Prevalence, q = 1- P, L = Allowable error. Source of data: It is a hospital based study of 150 patients who underwent small incision cataract surgery. All patients were inpatients of the Gadag Institute of Medical Sciences, Gadag. Before surgery full informed consent was taken, detailed history and examination of vision test, anterior segment examination and slit lamp examination was done. Fundus evaluation with direct and indirect ophthalmoscopy, tonometry and sac syringing was done in all cases. Systemic examination and physician consultation for fitness prior to surgery was sought for required cases. Inclusion criteria: All patients were inpatients of hospital. All patients undergoing small incision cataract surgery. All patients who have senile cataract. Exclusion criteria: Any patients having Complicated cataract, Traumatic cataract, Diabetic cataract, Patients with glaucoma, and Hypertensive patients were excluded. Out of 150 patients 75 patients received subtenon’s anesthesia randomly by lottery method and rest 75 patients received peribulbar anesthesia. STATISTICAL ANALYSIS: Diagrammatic representation. Mean ± SD. Student T test. Chi-square test. THE PARAMETERS STUDIED:
3- Involving 3-4 quadrant
1- Involving 1 quadrant 2- Involving 2 quadrant 3- Involving 3-4 quadrant PRELIMINIARY EXAMINATION: Preliminary examination under torch light and visual acuity testing by Snellen’s chart will be done for all patients participating in the study. Slit lamp examination. Schiotz tonometry. Lacrimal sac syringing. Direct and indirect ophthalmoscopy. Investigations to screen diabetic patients – Urine sugar. Hypertensive patients – Recording of blood pressure. TECHNIQUE OF PERIBULBAR ANESTHESIA: Preparation of anesthetic solution lignocaine 2% with adrenaline 1: 200000 will be used. Hyluronidase 1500 IU will be dissolved in 30 ml of 2% lignocaine with adrenaline (1:200000) resulting in 50 IU/ml of anesthetic mixture. Peribulbar anesthesia was given in Supine position after 5% betadine solution painted on skin around eye. Technique: Patient will be asked to look in primary gaze. A 5 ml syringe with 24 gauge 2.5 cm needle will be taken. The initial injection will be injected inferior-temporally at the lower orbital margin midway between lateral canthus and lateral limbus. The needle will be advanced parallel to the plane of the orbital floor till 2.5 cm and 3 ml of anesthetic solution injected after careful aspiration to rule out intra-vascular placements. At supero-nasal margin of orbit second injection will be given, needle advanced to about 2.5 cm along roof and 2 ml of anesthetic solution injected massage will be given to eye ball and akinesia, analgesia and IOP recorded at 5 min. Repeat injection of 2-3 ml will be given at infero temporal margin for patients who will not develop adequate akinesia and analgesia. The akinesia, analgesia, intraocular pressure, chemosis and subconjunctival hemorrhage at 15 min will be recorded. TECHNIQUE OF SUBTENON’S ANESTHESIA: Preparation of anesthetic solution lignocaine 2% with adrenaline 1: 200000 will be used. Hyluronidase 1500 IU will be dissolved in 30 ml of 2% lignocaine with adrenaline (1:200000) resulting in 50 IU/ml of anesthetic mixture. Technique: It will be performed in the operation theatre under aseptic conditions. Conjunctiva anesthetized by instilling 4% lignocaine eye drops 2-4 times. After anesthetizing conjunctiva suitable wire speculum will be inserted, a button hole will be made in conjunctiva along the tenon’s capsule 3 mm from the limbus in the infero-nasal quadrant. The infero-nasal quadrant is accessed by asking the patient to look upwards and outwards. Then by holding conjunctiva along with tenon’s capsule the capsule is dissected 2-3 mm along the sclera. A 2 mm wide 2.2 cm 24 gauge curved blunt cannula will be inserted into subtenon’s space and passed posteriorly on the sclera until its tip lays behind the equator of globe where 3 ml of anesthetic solution will be delivered into subtenon’s space. SURGERY TECHNIQUE: All patients will undergo small incision cataract surgery after administration of the anesthesia. Lids retracted with speculum, Superior rectus bridle suture taken, Fornix based conjunctival flap taken, Episcleral tissue separated, Light cautery applied, Sclero-corneal tunnel made, A entry made with keratome , Capsulotomy performed with 26 number needle, Extension of sclero-corneal tunnel done, Hydro dissection and hydro delineation procedure carried out, Delivery of nucleus into anterior chamber, Nucleus expression will be done by sandwich technique, Cortical aspiration will be done by using manual simcoe irrigation aspiration cannula , Reformation of anterior chamber with viscoelastic substance, Placement of the posterior chamber intra ocular lens, Anterior chamber reformed with saline, Hemostasis maintained throughout the procedure Subconjunctival injection of antibiotic and steroid given, Pad and plaster applied.
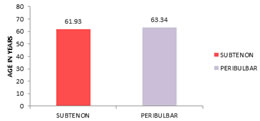
RESULTS A Total of 150 patients were selected for current study of which 75 patients underwent small incision cataract surgery under subtenon's anesthesia and 75 under peribulbar anesthesia satisfying all inclusion and exclusion criteria. Study was conducted from January 2018 to January 2019 AGE DISTRIBUTION In our study, patient’s age in subtenon's group was ranging from 40-80 years and in peribulbar group from 42-85 years. Student T test showed no significant difference in age distribution of the study groups. ( t value = - 0.162. P value = 0.327). TABLE 1: MEAN AGE DISTRIBUTION OF STUDY GROUP
Figure 1: Mean age distribution of study group
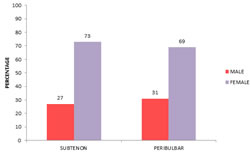
SEX DISTRIBUTION: In subtenon's group out of 75 patients 20(27%) were males, 55(73%) were females. In peribulbar group out of 75 patients 24(31%) were males, 51(69%) were females. Student T test showed no significant difference in sex distribution of study groups. (P value = 0.108).
TABLE 2: GENDER DISTRIBUTION OF STUDY GROUP
Figure 2: Gender distribution of study group INTRA OCULAR PRESSURE:- Pre op IOP: In subtenon's group mean IOP was 16.72 mmHg +/- 1.11 SD. In peribulbar group it was 16.36 mmHg +/- 1.34 SD. Student T test showed no statistical significant difference in the pre operative intraocular pressure between two groups. (t value = - 0.321. P value = 0.08).
TABLE 3: MEAN PRE OPERATIVE IOP AMONG STUDY GROUP
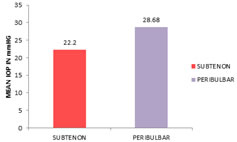
Figure 3: Comparison of pre operative IOP IOP at 1 min: In subtenon's group mean IOP was 22.20 mmHg +/- 4.22 SD, In peribulbar group it was 28.68 mmHg +/- 6.30 SD. Student T test showed significant difference. (t value = - 1.52. P value = 0.001). TABLE 4: MEAN IOP AT 1 MIN AMONG STUDY GROUP
Figure 4: Comparision of IOP at 1 min
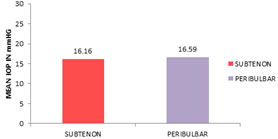
IOP at 15 min: In subtenon's group mean IOP was 16.16 mmHg +/- 1.41 SD, In peribulbar group it was 16.59 mmHg +/- 1.44 SD. Student T test showed no significant difference between the two groups. (t value = - 0.0307. P value = 0.07). Indicating no significant difference in intraocular pressure at 15 min. TABLE 5: MEAN IOP AT 15 MIN AMONG STUDY GROUP
Figure 5: Comparision of IOP at 15 min
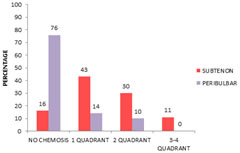
CHEMOSIS: Out of 75 patients in subtenon's group 12(16%) had no chemosis, 32(43%) had chemosis in one quadrant, 23(30%) in two quadrants, 8(11%) in three or more quadrants. In peribulbar group 57(76%) had no chemosis, 11(14%) had chemosis in one quadrant, and 7(10%) in two quadrants. 0 in three or more quadrants. Chi-square test showed significant difference between two groups. (Chi value 56.137 at 3ds. P value = 0.00).
TABLE 6: DISTRIBUTION OF CHEMOSIS AMONGST STUDY GROUP
Figure 6: Distribution of chemosis amongst study group
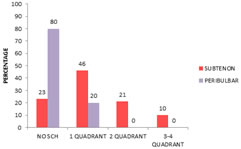
SUBCONJUNCTIVAL HEMORRHAGE: Out of 75 patients in subtenon's group 17(23%) had no SCH, 35(46%) had SCH in one quadrant, 16(21%) in two quadrants, 7(10%) in three or more quadrants. In peribulbar group 60(80%) had no SCH, 15(20%) had SCH in one quadrant, and 0 in two quadrants. 0 in three or more quadrants. Chi-square test showed a significant difference between two groups. (Chi value 55.013 at 3ds. P value = 0.00). TABLE 7: DISTRIBUTON OF SCH AMONGT STUDY GROUP
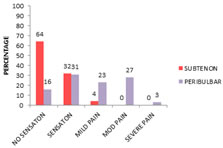
Figure 7: Distribution of sub conjunctival hemorraghe amongst study group ANALGESIA: During administration of anesthetic. In subtenon's group 48(64%) had no sensation or pain, 24(32%) experienced sensation, 3(4%) experienced mild pain, 0-none had moderate pain and 0-none had severe pain. In peribulbar group 12(16%) had no sensation or pain, 23(31%) experienced sensation, 17(23%) experienced mild pain, 21(27%) had moderate pain and 2(3%) had severe pain. Chi-square test showed significant difference between two groups. (Chi value 56.858 at 4ds. P value = 0.00).
TABLE 8: DISTRIBUTION OF ANALGESIA DURING ADMINISTRATION OF ANESTHESIA AMONST STUDY GROUP
Figure 8: Distribution of analgesia during administration of anesthesia among study group
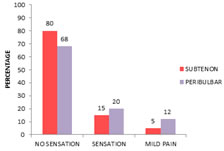
INTRA OPERATIVE ANALGESIA: In subtenon's group 60(80%) had no sensation or pain, 11(15%) experienced sensation, 4(5%) experienced mild pain, 0-none had moderate pain and 0-none had severe pain. In peribulbar group 51(68%) had no sensation or pain, 15(20%) experienced sensation, 9(12%) experienced mild pain, 0-none had moderate pain and 0-none had severe pain. Chi-square test showed no significant difference between two groups. (Chi value 8.581 at 2ds. P value = 0.102).
TABLE 9: DISTRIBUTION OF ANALGESIA INTRAOPERATIVE AMONG STUDY GROUP
Figure 9: Distribution of analgesia intraoperative among study group
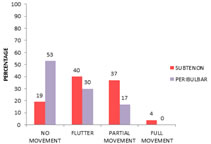
AKINESIA AT 5 MIN: In subtenon's group 14(19%) had no movements, 30(40%) had flutter, 28(37%) had partial movements, 3(4%) had full movements. In peribulbar group 40(53%) had no movements, 22(30%) had flutter, 13(17%) had partial movements, 0-none had full movements. Chi-square test showed significant difference between two groups. (Chi value 21.223 at 3ds. P value = 0.001).
TABLE 10: DISTRIBUTION OF AKINESIA 5 MIN AFTER ANESTHESIA AMONG STUDY GROUP
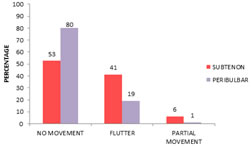
Figure 10: Distribution of akinesia 5 min among study group AKINESIA AT 15 MIN: In subtenon's group 40(53%) had no movements, 31(41%) had flutter, 4(6%) had partial movements, 0-none had full movements. In peribulbar group 60(80%) had no movements, 14(19%) had flutter, 1(1%) had partial movements, 0-none had full movements. Chi-square test showed significant difference between two groups. (Chi value 12.367 at 2ds. P value = 0.001). TABLE 11: DISTRIBUTION OF AKINESIA 15 MIN AFTER ANESTHESIA AMONG STUDY GROUP
Figure 11: Distribution of akinesia 15 min among study group
DISCUSSION EFFECTS OF ANESTHESIA : INTRAOCULAR PRESSURE: In our study of subtenon's group the mean IOP was 22.20 mmHg and in peribulbar group the mean IOP was 28.68 mmHg at 1 min. difference was significant between two groups. Barak Azmon et al. in their study of 64 patients found a significant difference in the mean IOP between the two groups at 1 min.6 Pazit Pianka in their study of 40 patients compared effect of peribulbar and subtenon's anesthesia on IOP found no significant change in IOP at 1 min and 10 min. this was not similar to our study. In their study 2 ml of lignocaine was used in the peribulbar group where as in our study 8 ml of lignocaine was used. This difference in volume explains the difference between the results of the two studies.22 The mechanism of intraocular pressure rise after local ocular anesthesia has been attributed to the mechanical compression of the eye caused by large volume of solution injected in the small orbital space.6 CHEMOSIS: Chemosis in subtenon's anesthesia is very frequent. In our study only 16 % had no chemosis, 50 % had 1 quadrant chemosis and 44% had more than 1 quadrant chemosis, where as in peribulbar anesthesia 76% had no chemosis, 14% in 1 quadrant, and 10% more than 1 quadrant chemosis. The chemosis was probably due to anterior tracking of local anesthetic fluid into subconjunctival space. Stan J Roman et al. reported in their study that 39% had chemosis involving more than 1 quadrant in subtenon's anesthesia. It takes a little practice to limit chemosis by ensuring that the local anesthetic solution is truly delivered to posterior subtenon's space and not to anterior subconjunctival space. Chemosis did not interfere in any surgical steps in our study.20 ANALGESIA Analgesia during administration: In our study in subtenon's group 64% of patients did not experience any sensation or pain during administration, while in peribulbar group only 16% of patients did not experience pain rest all patients experienced moderate to severe pain. Roman et al. in their study reported that administration of subtenon's anesthesia was painless in 99% patients of which 55% had no pain and 44% had only sensation.20 Briggs M C et al. in their study reported that subtenon's anesthesia administration was slightly less painful than peribulbar anesthesia administration. 24 Intra operative analgesia: In our study 80% patients of subtenon's group did not experience pain intra operatively while in peribulbar group 70% patients did not experience any pain or sensation. There was no significant difference between two groups. Tasneem Parker et al. in their study reported no significant difference between peribulbar and subtenon's groups in intra operative pain during surgery. 9 Yoshihiro Tokuda et al. compared analgesic effect of different doses of subtenon's anesthesia and reported that 3 ml of subtenon's anesthesia was significantly more effective than lower doses. 785 of patients did not experience any pain or sensation during surgery which is comparable to our study.21Karpran et al. reported that 67% of patients did not experience any pain or sensation in subtenon's anesthesia, and only 16% reported no pain or sensation in retrobulbar anesthesia.25 Subtenon's and peribulbar anesthesia comparably provide effective and adequate intra operative analgesia in cataract surgery. AKINESIA: In our study at 5 min after administration of anesthesia, in subtenon's group 20% had no movements and in peribulbar group 53% had no movements. At 15 min after administration of anesthesia, in subtenon's group 54% had no movements and in peribulbar group 80% had no movements. Stevens et al. reported complete akinesia at 15 min after administration of anesthesia in 52% of patients in subtenon's anesthesia.26 Khurana et al. reported complete akinesia with subtenon's anesthesia in 52% of patients after 15 min of administration.27 Kollaritis et al. reported complete akinesia in 82% of cases in peribulbar and 80% in subtenon's anesthesia.28 Delivery of local anesthetic fluid in the posterior space between sclera and tenon’s capsule allows direct spread along extra ocular muscles. It also enables diffusion of local anesthetic. This diffusion from subtenon's space into conal space explains the time taken for obtaining complete akinesia. This mechanism of action by diffusion is supported by following studies. Steven A Rowley et al. in their study reported hyaluronidase has a beneficial effect in improving the quality of motor blockage achieved with subtenon's local anesthesia.29 Guise P et al. showed better akinesia after 9 min with hyaluronidase group with the control group in subtenon's local anesthesia.30In our study mild flutter or partial move ments of subtenon's anesthesia group did not affect the surgery, it was negotiated by patient cooperation and fixation of globe by forceps.
CONCLUSION Subtenon's anesthesia and peribulbar anesthesia provide adequate analgesia, akinesia during cataract surgery. However there is slight difference between two groups in providing akinesia, Subtenon's anesthesia has some partial residual movements which can be negotiated with patient cooperation or fixation forceps. The residual partial movements of subtenon's anesthesia did not hamper any steps in cataract surgery. Subtenon's anesthesia is less painful during administration compared to peribulbar anesthesia. Intraocular pressure in subtenon's anesthesia remains within acceptable limits where as it is raised immediately after peribulbar anesthesia. Subconjuctival hemorrhage and chemosis are frequently encountered in subtenon's anesthesia compared to peribulbar anesthesia, which also do not hamper any steps of cataract surgery. Subtenon's anesthesia is a safe and effective anesthesia compared to peribulbar anesthesia in small incision cataract surgeries.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home