|
Table of Content - Volume 18 Issue 1 - April 2021
A prospective case-controlled study on the outcome of cataract surgery in diabetic and non-diabetic patients in a government medical college, Hubli
Shivasagar N1*, Savitha Kanakpur2
1Senior Resident, Department of Ophthalmology, PES Institute of Medical Sciences and Research, Kuppam, INDIA. 2Professor and HOD, Department of Ophthalmology, Karnataka Institute of Medical Sciences, Hubli, INDIA. Email: reus.sagar10@gmail.com
Abstract Background: To compare the visual outcome following cataract surgery in diabetics and non-diabetics. Method: A prospective case series descriptive study of 50 eyes in the diabetic group and 50 eyes in the non - diabetic group that underwent small incision cataract surgery with posterior chamber intraocular lens implantation. Age, sex, surgical technique, follow up and pre- and postoperative best corrected visual acuity (BCVA) were evaluated. Results: Overall 100 patients (50 diabetic and 50 non diabetics), of which 38 were males and 62 females. The mean age group of the patients in diabetic group was 55.36 ± 8.41 years and 58.36 ± 6.83 years in control group. Of the diabetics 98% patients were on treatment and 44% patients had good glycaemic control prior to surgery. All patients underwent small incision cataract surgery. Follow up duration was 4 weeks. Mean pre-operative best corrected visual acuity in the diabetic group was 1.72 +0.48 and that in the control (non-diabetic) group was 1.51 +0.51. Mean post-operative best corrected visual acuity in logMAR units in the diabetic group was 0.44+ 0.38 and in the control group was 0.36+ 0.24. The difference in pre- and post-op visual outcome was statistically significant (p=0.001). Post-operative visual acuity of 6/12 or better was achieved in 56% eyes in diabetics and 68% among non-diabetics. Post-operative complications included: corneal edema, striate keratopathy, anterior chamber reaction, pigment dispersion, and posterior capsular opacification. The incidence was significantly higher in the diabetic group (p=0.001). Key Word: Cataract; Cataract surgery outcome; Diabetic Cataract; SICS; Visual outcome of cataract surgery,
INTRODUCTION Blindness due to cataract presents an enormous problem in India not only in terms of human morbidity but also in terms of economic loss and social burden. The annual incidence of cataract blindness in India is about 3.8 million. About one sixth of world’s total blind with visual acuity >3/60, lives in India. Worldwide more than 285 million people are affected by diabetes mellitus and is expected to increase to 439 million by 2030 according to the International Diabetes Federation. Globally, cataracts remain the leading cause of blindness, affecting approximately 18 million people. Persons with diabetes mellitus have been found to be at increased risk of developing cataract when compared to non-diabetic and nearly two third of the diabetic population shows evidence of cataract. Studies have shown an increased risk of ocular complications in diabetics after cataract surgery, but modern surgical techniques have minimized them, leading to an overall good visual outcome. Macular edema before surgery is the most common condition that limits post-operative visual recovery. Cataract surgery in diabetics is indicated for visual improvement or to allow assessment and treatment of posterior segment pathology. Overall, up to 20% of all cataract procedures are estimated to be performed for diabetic patients1 and many patients seeking cataract surgery have a co-existing diabetic eye disease. Diabetes mellitus influences the function and morphology of the eye lens. Poor visual outcome in diabetics has been linked with the severity of retinopathy and maculopathy prior to cataract surgery. Pre-operatively it is recognized that, in diabetics, there is higher incidence of pigment dispersion and fibrinous reaction in the anterior chamber, together with the development of posterior synechiae, as well as increased risk of capsule rupture and vitreous loss. Diabetic patients are more prone to postoperative complications such as Rubeosis, neovascular glaucoma, macular edema (Diabetic and cystoid), severe inflammation, (Iritis, uveitis, endophthalmitis) vitreous haemorrhage, synechiae to IOL, retinal detachment and corneal decompensation. Diabetic are more prone to develop posterior capsule opacification postoperatively. The increasing incidence of diabetes in developing countries such as India necessitates an assessment of the surgical outcome of diabetic cataract among the study population. This study is being carried out to assess and understand the visual outcome of surgery in Diabetic cataracts with the intention of making recommendations for improved care. Objectives:
MATERIALS AND METHODOLOGY Source of Data: Patients coming to Karnataka Institute Of Medical Sciences, Department Of Ophthalmology, Hubli.
Method of Collection of Data: Study design: Prospective case-control study. Study period: Jan 2015-Aug 2016. Place of study: Karnataka Institute Of Medical Sciences, Department Of Ophthalmology, Hubli. Sample size: 50 non diabetics (controls) and 50 diabetic (cases) Patients. Inclusion criteria
Exclusion criteria
Methodology Demographic data (age, sex, occupation, address). All patients underwent ocular examination before and after Small incision cataract surgery with Intraocular lens implantation Statistical Analysis Descriptive statistics such as mean, SD and percentage was used to present the data. Comparison between control and diabetic groups was done using chi square test for qualitative data and t-tests for quantitative data. A p-value less than 0.05 was considered as significant. Data was analysed by using software SPSS v16.0
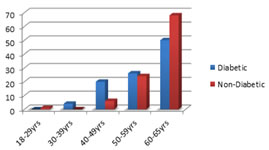
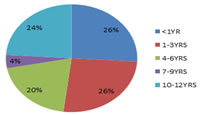
RESULTS The study group consists of 50 eyes of diabetics and 50 eyes of non-diabetics that underwent small incision cataract surgery with intraocular lens implantation. The age and sex wise distribution, glycaemic control, preoperative visual acuity, coexistent morbidities, complications of the procedure and final visual outcome were analysed. The mean age group of the patients in diabetic group was 55.36+8.41 and 58.36+6.83 in non diabetic group. Majority of the patients in both groups belonged to the age group 60-65 years (Fig.1). 21(42%) of the study participants were male and 29(58%) were female. Among the non-diabetics, 17(34%) were male and 33(66%) were female. Majority of patients 26(52%) were recently diagnosed diabetics with duration of disease being less than 3 years. There were about 12(24%) patients with duration of disease being more than 10 years.(Fig.2) Of the fifty patients in the diabetic group, 22(44%) had good glycaemic control (FBS: 70-100mg/dl). Remaining 28(56%) patients had high blood sugar levels (>100mg). This included patients with and without treatment. 49(98%) of the patients were on treatment for type 2 diabetes mellitus with either injection insulin or oral hypo-glycaemic agents while the remainder 1(2%) was not on any medication for the same.
Figure 1: Distribution of patients in two groups (Diabetic and non-diabetic) by age groups
*Patients above 65 years of age were excluded. Figure 2: Duration of diabetes in cases
Table 1: Comparison of two groups (diabetic and non-diabetic) with co-existing systemic condition
P <0.05 significant Systemic hypertension though the most frequent co-morbid disease in both the groups, was more frequent among diabetics as seen in this study, that is 20(40%) compared with 5(10%) of the non-diabetic counter parts. The difference was statistically significant. The other co-morbid diseases were hypothyroid which was seen in 2(4%) diabetic patients and ischaemic heart disease which was seen one patient in both the groups. Table 2: Comparison of two groups (diabetic and non-diabetic) with visual acuity at pre-operative BCVA
*P <0.05 significant Thirty patients (60%) in the diabetic group and twenty-five (50%) in the non-diabetic group were having vision of less than counting fingers 2 meters (<2/60). Majority of the patients 39(78%) in diabetic group and 38(76%) in non-diabetic group were having vision of less than 6/60. Only 11(22%) in diabetics and 12(24%) in non-diabetics had vision of 6/36-6/24(measured by Snellen visual acuity chart). The p value was not statistically significant. The mean best corrected pre-operative visual acuity in both the groups was calculated in logMAR units. The mean preoperative best corrected visual acuity in the diabetic group was 1.72+0.48 and that in non-diabetic group was 1.51+0.51. The p value (>0.05) was not statistically significant.
Table 8: Final visual outcome
*P value <0.05 Significant
Majority of the patients 28(56%) in the diabetic group and 34(68%) in the non diabetic group had visual acuity of 6/12 or better at the end of 4 weeks of follow up. Only 3 patients in the diabetic group and 1 patient in the non-diabetic group had visual acuity less than 6/60. The mean post-operative best corrected visual acuity in logMAR units in the diabetic group was 0.44+0.38 and in the non-diabetic group was 0.36+0.24. On comparing the pre-operative and post-operative visual acuity in both the groups the p value (0.001) was statistically significant.
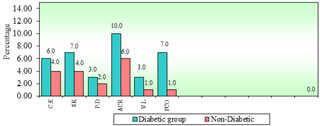
Figure 3: Post-operative complications
Corneal edema was found in 6 (12%) and 4 (8%) of the cases in diabetic and non-diabetic groups respectively which was higher in diabetics compared to non-diabetics. Striate keratopathy was found in 7 (14%) of the diabetics compared to 4 (8%) in non-diabetics. Pigments over IOL were seen in 3 (6%) of the cases in diabetics as compared to 2 (4%) in the control group. 10 (20%) among the diabetic group and 6 (12%) in the non diabetic group had anterior chamber reaction. The development of PCO in diabetics was seen in 7 patients (14%) compared to 1 patient (2%) in non-diabetics, at the end of 4 weeks. In our study all the patients in both the groups had various grades of immature cataract and we found that the prevalence of mixed cataract was higher (66%), than that of monotype cataract (24%). Of the mixed types, the most common type was a combination of nuclear cataract (NC), cortical cataract (CC), and posterior subcapsular cataract (PSC) (70%) followed by the combination of CC and PSC (26%). Of the monotype ones, the most common cataract CC (35%) followed by NC (15%) and PSC (10%). Out of 50 diabetics complications were seen in 36(72%) patients as compared to 18(36%) non diabetics. The p value(0.001) was found to be statistically significant
DISCUSSION The study includes cases consisting of 50 diabetic and 50 non diabetic patients (control), who underwent cataract surgery who compared for their visual outcome. The Framingham3 study shows a 3-4-fold increased prevalence of cataract in patients with diabetes under 65 and up to a twofold excess prevalence in patients above 65. It also showed a predisposition to women. In our study, we found that 25 (50%) in diabetics and 34(68%) in control group were in the age group of 60-65 years. And in diabetic group 29 (58%) were females and 21 (42%) were males. Among the controls, 17 (34%) were males and 33 (66%) were females. In diabetic group, majority of patients 28 (56%) had high blood glucose level (FBS: >100 mg/dl). 49 (98%) of the patients were on treatment for type 2 diabetes mellitus with either injection insulin or OHAs while the remainder 1 (2%) was not on any medication. In our study it was found that systemic hypertension though the most frequent co-morbid disease in both the groups, was more frequent among diabetics i.e. 20 (40%) compared to 5(10%) of the non-diabetic counter parts which was similar to a study by Oluwatoyin H et al.14 in which hypertension was seen in 60.9% compared with 26.1% in non-diabetic group. Similarly, Squirrel et al.4 found that 55% had hypertension, Mittra et al.5 found 68% had hypertension. Majority of the patients in our study had poor pre-operative visual acuity. 30(60%) of the diabetics and 25(50%) of the control patients had vision between counting fingers <2 meters (<2/60). Majority patients 39 (78%) of the diabetics and 38 (76%) of the non-diabetics had visual acuity less than 6/60. 11 (22%) of the diabetics and 12 (24%) of the control had vision of 6/36 – 6/24. Corneal edema was found in 6 (12%) and 4 (8%) of the cases in diabetic and non-diabetic groups respectively on post-op day 1, which was considerably higher in diabetics compared to non-diabetics. Striate keratopathy was found in 7 (14%) of the diabetics compared to 4 (8%) in nondiabetics. According to Oluwatoyin H et al.3 30% in diabetic compared to 13% in control group and Larsson et al.6 have shown that diabetes has been associated with structural changes in corneal endothelial cells such as polymegathism and pleomorphism. Lee JS et al.7 showed a decrease in corneal endothelial cell density and the coefficient of variation by cell size significantly increased the risk for proliferative diabetic retinopathy. Study by Morikuba S et al.8 has shown increase in the corneal thickness was greater on post-op day one among diabetic patients and also showed that corneal endothelial loss was maximal at 1st week after operation. Pigments over IOL were seen in 3 (6%) of the cases in diabetics as compared to 2 (4%) in the control group. But Oluwatoyin et al.14 found that there is increased pigment dispersion in diabetic patients undergoing cataract extraction and IOL implantation. In our study, 10 (20%) eyes in the diabetic group and 6 (12%) eyes in the non-diabetic group had anterior chamber reaction. Diabetic patients had more anterior chamber reaction compared to non-diabetics similar observations made by Oluwatoyin et al.14, I A Cunliffe et al.15 and Mechini et al.9. Ivancic et al.10 and Moriarty et al.11 reported inflammatory reaction fibrinous uveitis and PCO as the most common complications of cataract surgery among diabetics. In our study the development of PCO in diabetics was 7 eyes (14%) compared to 1 eye (2%) in non-diabetics, at the end of 4 weeks, similar to a study by Ebihara Y et al.12, also showed significant increase in PCO in diabetic compared to non-diabetic patients. A study by Hyashi K et al., also showed similar findings. Diabetic patients have significantly more extensive PCO after cataract surgery than non-diabetic patients. Majority of the patients, 28 (56%) in the diabetic group and 34 (48%) in the non-diabetic group had visual acuity of 6/12 or better at the end of 4 weeks of follow up. Only 3 patients in the diabetic group and 1 patient in the control group had visual acuity less than 6/60 which was due to posterior capsular opacification.
CONCLUSION This is a prospective case-control study of comparison of visual outcomes following small incision cataract surgery with intraocular lens implantation in diabetics and non-diabetics. There were 50 eyes each in the diabetic and non-diabetic group. The pre-operative best corrected visual acuity was compared to the post-operative best corrected visual acuity in both the groups and the P value was statistically significant (p=0.01). The post-operative complications that were observed during the period of this study were corneal edema, striate keratopathy, anterior chamber reaction, pigment dispersion over IOL, and posterior capsular opacification. These were significantly more in the diabetic group when compared to the non-diabetics. None of them were visually disabling and resolved during the course of follow up without any surgical intervention. Therefore, we concluded that small incision cataract surgery in diabetics without diabetic retinopathy yields similar visual outcomes as non-diabetics. There definitely is a higher incidence of post-operative complications among diabetics which can be conservatively managed. The drawbacks of this study were small sample size and shorter duration of follow up.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home