|
Table of Content - Volume 19 Issue 2 - August 2021
A clinical study on ocular manifestations of diabetes mellitus
Suhas S Sarawade1, Sharad S Jadhav2, Supriya Chitupe3, Roshani P Ghuge4*
1Professor and Head, 2Assistant Professor, 3Senior Resident, 4Junior Resident, Department of Ophthalmology, Dr.Vaishampayan Memorial Government Medical College, Solapur, Maharashtra, INDIA. Email: roshanighuge1920@gmail.com
Abstract Background: To study various ocular manifestations of diabetes mellitus. To find out the incidence of different ocular manifestations of diabetes mellitus. To study different conditions causing visual loss. Material and Methods: The ocular manifestations were studied in 500 patients attending the diabetic patients attending the Out Patient Department of Medicine of our tertiary care center during a period of 2 years. Results: It was noted that among the study population, majority of them (41.4%) were in the age group between 51-60 years and men (55.8%) were more in number than females (44.2%). Diabetic retinopathy was the most common ocular manifestation (46.6%) followed by glaucoma (2.6%). Cataract was found in 42.2% patients but it was senile in nature, not true diabetic cataract. In5.2%patients cataract appeared to occur earlier. This could be earlier onset of cataract. Conclusion: These ocular findings suggest that regular screening and eye examinations of diabetic patient is important to reduce the incidence of visual impairment. Key words: Diabetes Mellitus, Diabetic Retinopathy, Cataract
INTRODUCTION Diabetes mellitus is the most common metabolic disorder of the world. Diabetes mellitus along with its complications are becoming world’s most significant cause of morbidity and mortality. According to International Diabetes Federation, it affects more than 240 million people worldwide and this number is expected to reach roughly 370 million by 2030.1,2 According to the Diabetes Atlas 2006 published by the International Diabetes Federation, the number of people with diabetes in India currently around 40.9 million is expected to rise to 69.9 million by 2025.3 The increased number of diabetics in India is likely to be due to a significant increase in the incidence of type 2 diabetes, caused by unprecedented rates of urbanization of rural areas. In the developed world, diabetes is common among the elderly but in contrast 35-64 years is the most commonly affected age group in the developing world. The chronic complications of diabetes are due to pathological changes affecting the blood vessels of the involved organs. The disease can involve either the small blood vessels (microangiopathy) or the larger blood vessels (macroangiopathy). Diabetic retinopathy and diabetic nephropathy are predominantly the result of microvascular disease. There is a high potential for vision loss in patients with diabetes mellitus, manifesting with a range of ocular diseases involving structures from the lids to retina and to cranial nerves 3–5. Diabetic eye disease is becoming an increasing problem among developing countries due to longer life expectancy and a higher incidence of diabetes. Indians have a several-fold higher prevalence of diabetes for all age groups compared with European populations, as reported by the International Diabetes Epidemiology Group. Diabetic retinopathy, the most common microvascular complication of Diabetes mellitusis predicted to be the principal reason of new blindness among working population and a major cause for a higher percentage of visual loss in patients with Diabetes mellitus. Ocular complications of diabetes manifests in myriad ways, but manifestations of diabetes other than diabetic retinopathy are easily overlooked. Our study is a step towards the direction to prevent and manage ocular complications of diabetes by assessing the lacunae in the health awareness of the patients by
MATERIAL AND METHODS This prospective study was carried out on diabetic patients attending the Out Patient Department of Medicine of our tertiary care center. 500diabetes patients were studied in detail, for ocular manifestations, selected by random sampling over a period of 2 years. Patient’s basic information was noted first, which includes name, age, sex, reg. no, occupation etc. patient’s postal address was also noted in detail in order to call them again in future for follow up if required. Patient’s chief ocular complaints were also noted especially of dimness of vision, floaters, flashes, ocular pain, metamorphopsia etc. Patient’s complaints related to diabetes and other systemic diseases were also asked. A brief history about diabetes was asked in the form of type of diabetes, duration of diabetes and the present treatment for diabetes. Treatment history of other associated systemic disease was also noted. The diabetic age as calculated from the time of diagnosis, obviously need not accurately represent the true duration of diabetes, particularly in type 2 diabetics. Specific significant positive family history for diabetes was also asked and patient’s personal history was noted. Patient’s past history regarding other systemic disease and hospitalisation was also asked. The visual acuity was tested by snellen’s chart. The intraocular tension was measured with a Schiotz tonometer. The tension was taken prior to dilatation of pupils. Sac syringing of both the eyes were done. Colour vision was tested. Each eye was examined in detail with the help of a torch light. Slit lamp examination was done. The fundus examination was done by dilating the pupil with tropicamide and phenylephrine eye drops examining by direct and indirect ophthalmoscopes. The media, disc, vessels, macula, periphery were examined and the findings noted. The visual field examination and fundus fluorescein angiography was done wherever needed. The basic investigations were performed and noted, like FBS, PP2BS, HB1AC, urine examination, complete blood count etc. All the data regarding the patient was taken according to Proforma, which is given at the end of the study.
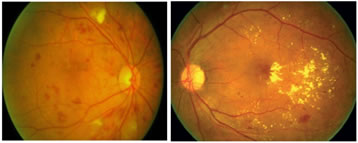
Figure 1: Picture showing Severe non-proliferative diabetic retinopathy; Figure 2: Picture showingClinically significant macular edema
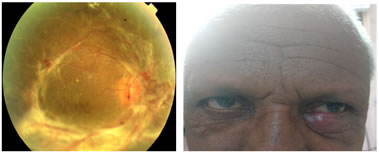
Figure 3: Picture showing Proliferative diabetic retinopathy; Figure 4: Picture showingStye in a diabetic patient
RESULTS AND DISCUSSION Sex In the present study 279 patients were male while 221 patients were female. (male to female ratio - 1.26) Table 1: Distribution of Patients according to Sex
Similar sex distribution wherein males outnumbering females was found in a study conducted by Muawyah.4 The prevalence of NPDR was higher in male diabetes patients (41.2 %) than in female diabetes patients (33 %). Our study showed a higher prevalence of DR amongst male subjects, while Wisconsin Epidemiological study of Diabetic Retinopathy found higher prevalence of Diabetic Retinopathy in females .5,6 Comparable results with regard to increased incidence of diabetic retinopathy in male patients was found in a study by Sunil Gupta.7 In UKPDS study (1998) retinopathy was present in 39% males and35% females. Male: female ratio was1.6:1. In the CURES eye study (2005) Mohan Rema, Sundaram Premkumar and others found that Diabetic retinopathy was more common in males.8 Age In this study most of the patients were found to be in the age group of 51-60 years (41.4 %).
Table 2: Distribution of patients according to age group
Comparable age distribution was found in a study by Raheja. (9)According to Duke elder (1967) diabetes mellitus occurs in people in the fifth and sixth decades of life , 50% cases appearbetween the age of 40 and 50 yearand only 5 % in the first decade of life .In the study done by Harold A Kahnand Robert F Bradley in 1975 , out of914 patients studied527 were in age group of 45-74 years (58%).(10) In 1999 ,Vijay Vishwanathan,did a studyin which most of the diabetic patients were in age group of 45- 65 years .(11) Distribution by type of diabetes mellitus In our study, 52(10.4%) patients were of type 1 diabetes mellitus and 448 (89.6%) patients were of type 2 diabetes mellitus.
Table 3: Distribution of patients by type of diabetes
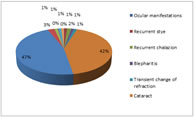
I.K. Brown and A. Thelwall Jones in 1964 found in relation to type of diabetes mellitus and prevalence of diabetic retinopathy.12 H.J .Bodansky , A. G. Cuuworth et al. in 1982 found that there was a strongly significant association between type 1 diabetes and proliferative diabetic retinopathy and type 2 diabetes and diabetic maculopathy.13 Ocular manifestations and their percentage of occurrence In the present study we found retinopathy to be the most common ocular manifestation occurring in diabetes subjects (46.6%). The prevalence of Primary open angle glaucoma was (2.6%) and of neovascular glaucoma was 1.2%. Recurrent stye was found in 1.2%patients and extraocular muscle palsy was found in 1% of patients.
Table 4: Ocular manifestations and their percentage of occurrence
The prevalence of diabetic retinopathy varied from 28.8%in persons who had diabetes for less than five years to 77.8% in persons who had diabetes for 15 or more years in a study conducted by Klein et al.5 Findings similar our present study regarding primary open angle glaucoma prevalence was found in studies conducted by Dobson and Girarid.14 Diabetes is the underlying cause in 25–30% of patients aged 45 years and older who develop acute extra ocular muscle palsy (Rush JA) .(15) In a study by Watanabe K, 1% of patients with diabetes were found to have cranial nerve palsies, compared with only 0.13% of control subjects.16
Figure 5: Percentage
Type of diabetes and associated ocular manifestation A significant association was noted between the type of diabetes and associated ocular manifestation in the present study. In our study21.15 % of patients with type 1 diabetes mellitus had NPDR while 39.5 % of patients with type 2 diabetes mellitus had NPDR. The prevalence of NPDR was higher in type 2 diabetes subjects, while the prevalence of PDR was higher in subjects with type 1 diabetes (9.61%) This result is similar to the results obtained by Muawyah.4 Diabetic maculopathy Macular edema was found in 30.9 % of patients in this study. The prevalence of maculopathy was remarkably high (42% in type 1 and 53% in type 2 diabetic patients) in a study conducted by zander et al.17 Duration of diabetes and associated ocular manifestation In this study we found a significant correlation between duration of diabetes and associated ocular manifestation. The most notable manifestation seen with increased duration of diabetes was NPDR (seen in48 % subjects with diabetes for 6-10 year duration). Increased incidence of retinopathy with increase in duration of diabetes (type1 and type 2) was noted in studies conducted by Klein et al. and Yanko et al.18 Retinopathy versus regular and irregular treatment That subjects taking regular treatment(oral tablets/insulin) with controlled sugar level had lower prevalence of mild NPDR(42.6 %), moderate NPDR(45 %) and severe NPDR(39.8 %) when compared to the group not taking treatment regularly. Regular treatment and follow up should be stressed in the management of diabetes mellitus. In a study conducted by jacobson et al. Compared with individuals with continuous follow-up, patients with irregular clinical visits were more likely to be from families of lower socioeconomic class levels and rural areas.19 Severity of NPDR versus control of diabetes In our study, diabetic retinopathy was graded according to ETDRS classification of diabetic retinopathy. In our study, out of 500 patients, NPDR was present in (45.6 %) patients. Maximum no. of patients, 89 i.e. (39.3%), had moderatenon –proliferative diabetic retinopathy (moderate NPDR), followed by 61i.e (26.7%) patients with mild NPDR, 38i.e. (16.7%) patients had severe NPDR and40i.e (17.5 %) patients had proliferative diabetic retinopathy (PDR). In our study, glycemic control was defined on the basis of fasting (F) and post prandial (PP) blood sugar levels (BSL), HBA1C and past and drug history. Patients with F BSL > 130 mg %, PP BSL > 180 mg %, HBA1C > 7% were labelled having poor control of diabetes mellitus. Remaining patients were having good control of diabetes mellitus. All cases of PDR and severe NPDR in our study had poor control of diabetes and were on insulin treatment. Krolewski et al. (1986) found that the risk for development of proliferative diabetic retinopathy was greatestfor those with poor glycemic controlprior to development of PDR. (20) Diabetes control and complication trial and United Kingdom prospective diabetic study both showed that intensive blood glucose control retards the rate of progression of diabetic retinopathy.21,22
SUMMERY AND CONCLUSIONS A clinical study on ocular manifestations of diabetes mellitus was carried out in our hospital has following conclusions. Out of 500 patients studied, diabetic retinopathy was the commonest ocular manifestation of diabetes, followed by primary open angle glaucoma, neovascular glaucoma, recurrent stye and extraocular muscle palsy. Diabetic retinopathy was predominantly seen in males (279) than in females (221). The male to female ratio was 1.6 :1 . Most of the cases were in the age group of 51-60 years. 52 (10.4%) patients were of type 1 diabetes mellitus and 448 (89.6 %) patients were of type 2 diabetes mellitus. Out of 500 cases studied, 188 (37.6%) patients had NPDR with fundus findings like multiple microaneurysms, dot blot haemorrhages, hard exudates, cotton wool spots and venous dilatation with loop formation.40(8%) patients had PDR with fundus findings like microaneurysms, dot and large blot haemorrhages, hard exudates with NVD and NVE. Patients had advanced diabetic eye disease with findings like retinal detachment and vitreous haemorrhage. 26.7% patients had mild NPDR, 39.3% patients had moderate NPDR, 16.7 % patients had severe NPDR. PDR was present in 17.5 % cases.114 out of 188 patients of NPDR had duration of diabetes 6 to 10 years .22out of 40 patients of PDR had duration of diabetes >10 years. So incidence and severity of diabetes mellitus correlates well with duration of diabetes mellitus .Diabetic maculopathy was present in 72 (30.9%) patients out of 233 patients of diabetic retinopathy . The prevalence of maculopathy was greater in subjects with type 2 diabetes mellitus. Maculopathy was found more in PDR than NPDR.5patients with diabetic retinopathy had uncontrolled status of hyperglycemia. It correlates well with severity of diabetic retinopathy. Extra ocular muscle palsy is a also an ocular manifestation of diabetes. In this study, it was found in 1.0 % patients. There was no significant correlation between age of the diabetic subject and the associated ocular manifestations.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home