|
Table of Content - Volume 22 Issue 1 - April 2022
Management of secondary glaucoma in post-traumatic cataract with open globe injury with self-sealed corneal laceration in a tribal pregnant woman- clinical challenges - A case report
Deepthi Janga1*, B Dharma Raju1
1Department Of Ophthalmology, Rangaraya Medical College, Government. General Hospital, Kakinada, Andhra Pradesh, INDIA. Email: deepthijanga9@gmail.com
Abstract Background: The management of secondary glaucoma with traumatic cataract with self sealed open globe injury in a pregnant woman presents unique challenges. Several glaucoma medications have potential adverse effects on the foetus while treating the pregnant mother. Control of secondary glaucoma, corneal wound repair, lens extraction with IOL implantation with prior control of secondary glaucoma and good visual outcome in mother and with minimal adverse effects of anti glaucoma drugs on foetus is our goal of management. Key words: Glaucoma, pregnancy, glaucoma in pregnancy Ethical consent was taken from the patient
INTRODUCTION Trauma can affect lens in several ways either subluxated or dislocated lens in open globe injuries leading to traumatic cataract. Occlusion of iridocorneal angle is possibility with phacomorphic, subluxated, luxated lens. If lens capsule is ruptured lens proteins can impair aqueous outflow ( lens particle glaucoma) and by causing inflammatory response in anterior chamber(phaco antigenic glaucoma). In self sealed corneal wounds with ruptured lens capsule lens particle glaucoma is possible as described in present case here. Preoperatative management of secondary lens induced glaucoma with open globe injury in pregnant woman poses certain clinical challenges which we managed at our tertiary care centre. Safety of glaucoma medication has been taken care so that foetal well being is also part of our management The FDA has classified drugs according to their safety in pregnancy as under: Category A- deemed safe, Category B- possibly safe to use in pregnancy, Category C - adverse effects reported in animal studies, Category D- definite risks but possible benefits, Category X- drugs with known risks to the foetus that cannot be outweighed by possible benefits. As per FDA on evidence available category A,B,C,D,X drugs were choosen carefully. Beta blockers as class C medication can cause foetal bradycardia and cadiac arrhythmias. Brimonidine category B medication can cause CNS depression and apnoea. PG analogues category C drugs has high index of miscarriage, increased risk of mobius syndrome and terminal transverse limb defects.so PG analogues not a choice of first line medication in pregnancy. Carbonic anhydrase inhibitors CAI category C medication Brinzolamide is a better alternative to dorzolamide can be used with caution when possible benefit to mother overweighs theoretical risk to foetus. oral CAI cause renal tubular acidosis in infant. We used topical CAI ,beta blockers and brimonidine with caution since our patient is in 3rd trimester of pregnancy. Topical CAI brinzolamide is 1st choice in our case. NLD occlusion and eyelid closure reduced systemic absorption of medication. As per studies systemic absorption of topical Timolol decreased by 67% by NLD obstruction and 65% by eyelid closure.It also increased drug eye contact time resulting in higher intra ocular drug concentration.
CASE REPORT Here we present 31 year old tribal pregnant woman presented to our ophthalmology department with open globe injury (self sealed corneal laceration) traumatic cataract with secondary glaucoma. Foetal well being is assessed by obstetrician and possible anaesthetic side effects to mother and foetus discussed with anaesthetist and appropriate measures taken. Pre and post surgery foetal well being assessed by obstetritian, good visual outcome achieved with corneal wound repair, lens extraction with IOL implantation with good control of secondary glaucoma preoperatively. A 32 year old tribal woman presented to the ophthalmology department with a complaint of injury to RE and defective vision of recent onset.
Table 1: On examination
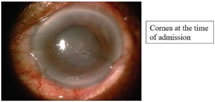
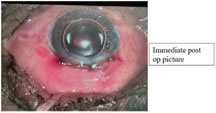
Patient being 7 th month of gestation, preoperative planning to decrease IOP medically was done carefully keeping in view of foetal wellbeing. Patient referred to obstetrician. Obstetric scan was done, intrauterine foetal status monitored. As per obstetrician advice systemic acetazolamide avoided to prevent oligohydramnios and the associated complications. Topical brinzolamide and timolol maleate combination used to control IOP. Topical systemic antibiotics, non-steroidal anti-inflammatory drugs used as a preoperative precaution to avoid possible infection in open globe injuries. After peribulbar anesthesia patient kept on oxygenation, prone waist position to avoid possible venacaval compression and hypotention. Corneal self-sealed laceration sutured with 10-0 nylon for wound strength, followed by sclerocorneal tunnel construction, cortical aspiration through ruptured anterior capsule, PCIOL implantation done. Anterior chamber maintained with air, postop recovery uneventful. Figure 1 Figure 2 Figure 3
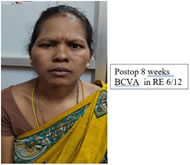
POST OP TREATMENT: Taxim 500mg BD, anti-inflammatory drops used, patient discharged after 1 week. Postop review done weakly for 8 weeks and is uneventful. Right eye
BCVA 8 weeks Postop in RE 6/12 Figure 4
DISCUSSION Management of lens induced glaucoma with open globe injury(corneal laceration) in pregnant woman in third trimester is challenging since ophthalmologist must establish good communication with both the patient and her obstetric specialist as well as anesthesiologist for foetal monitoring and maternal monitoring during surgery. Balancing the mothers risk to restore good vision and wellbeing of foetus is paramount importance. In our case management we carefully chosen preop glaucoma control with FDA approved category C drugs like topical Brinzolamide and Timolol. As pregnancy is advanced we avoided PGA's to lessen the risk of miscarriage or premature labor. Prior OBG/GYN and preanaesthetic checkup by anesthesiologist was done to avoid medico legal implications. Foetal well being monitored and documented preop intraop and Postop surgery. During peribulbar anaestbesia Bupivacaine is avoided since it causes foetal bradycardia and lidocaine was used. Surgical positioning of pregnant woman is important since gravid uterus can cause aortic and venacaval compression leading to hypotention so we rotated patient hips, abdomen, thighs while maintaining normal head position for ophthalmic surgery. Foetal heart rate monitoring was done to detect foetal asphyxia during surgery. Foetal ultrasound was done before and immediately after surgery to examine anatomical abnormality of foetus.
CONCLUSION The presentation of this case study highlights the importance of precautions to be taken while using anti glaucoma drugs for secondary glaucoma in open globe injuries in a pregnant woman and their effect on foetal well-being. Management of secondary glaucoma secondary to open globe injury and restoring good visual potential in pregnant mother and foetal well-being both preop and post op is our aim. Discussion with OBG/GYN and anesthesiologist help us to monitor possible potential side effects of an antiglaucoma drugs and anaesthetic drugs in mother and newborn. Proper positioning of pregnant mother during intraoperative period and foetal monitoring during surgery also important. This will avoid medicolegal implications along with proper documentation. In our case report we could able to achieve good visual recovery in mother and a healthy newborn.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home