Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 2 - February 2019
Lens induced glaucoma - Need of early diagnosis and treatment among rural population
Pranjali Kshirsagar1, M B Dongre2*
1Resident, 2Professor and HOD, Department of Ophthalmology, SRTR MC Ambejogai, Maharashtra, INDIA.
Abstract Purpose: To determine clinical presentation of lens induced glaucoma, complications and outcome of treatment. Methods: Retrospective analysis of 50 cases of lens induced glaucoma over period of 1 year between June 2017 to June 2018 at tertiary care centre. visual acuity and intraocular pressure (iop) was assessed preoperatively and postoperatively along with duration of symptoms and complications. Key Word: Lens induced glaucoma.
INTRODUCTION cataract is most important cause of preventable blindness in India. Negligence in cataract patient may land up into lens induced glaucoma and poor visual outcome if treatment is delayed. Though it is preventable and curable condition, late reporting among rural population may cause irreversible loss of vision. lens induced glaucoma described by Gifford1 as glaucoma associated with hypermature cataract. Von reuss2 described LIG as glaucoma associated with spontaneous absorption of lens substance through intact capsule. lens induced glaucoma may occur as open angle or angle closure glaucoma. open angle glaucoma can occur due to release of lens proteins through capsule in hypermature cataract that is phacolytic glaucoma or hypersensitivity to own lens protein following penetrating trauma or surgery (phacoantigenic glaucoma).angle closure may occur as in phacomorphic glaucoma. so LIG can be described3,4,5 by various names like lens induced uveitis and glaucoma, phacotoxic glaucoma, phacogenic glaucoma and phacolytic glaucoma. The study is retrospective hospital based study. the records of cataract cases who were diagnosed as LIG and operated during given period were analysed. Aim was to study profile of lens induced glaucoma leading to blindness in rural population.
MATERIALS AND METHODS Study was conducted at Tertiary care centre,which included 50 cases of Lens Induced Glaucoma, reported during one year period and operated for same. All of them reported with pain, redness and watering in addition to gradual progressive loss of vision in affected eye. All cases were diagnosed as LIG based on clinical findings and raised IOP. Other causes of glaucoma such as, traumatic cataract, complicated cataract, secondary cataract were excluded from study. Details Assessed were:
Ethical consideration- IEC approved study.
RESULTS AND DISCUSSION
Figure 1: Duration of Symptoms of lens induced glaucoma
Time gap between onset of acute symptoms of decrease in vision, pain and redness of affected eye and reporting of patients to hospital were analysed. Most of the patients reported within 4 to 6 days after onset of symptoms. 10% patients reported after 10 days of onset of symptoms. Late reporting among older patient was major determining factor along with surgical complications responsible for poor outcomes9.
Visual acuity was markedly reduced in all cases due to cataract as well as due to loss of corneal transparency due to raised IOP. Table 2: Post operative visual acuity of patients
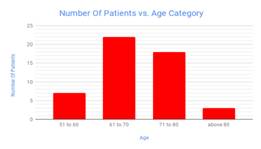
was noted from above table that 8% of all cases gained good vision. Maximum patients were having vision up to 1/ 60 ( 44%).Result can be compared with other studies like study Pradhan et al10 where 21% had postoperative vision less than 6/60. Table 3: Comparison for age category and number of Patients
Patient age ranged from 52 to 83 years. Youngest patient was 52 years female and oldest was 83 years male.
Table 4: Assessment of complications
Few intraoperative and postoperative complications noted in this study, which were responsible for poor vision11 Most common was striate keratopathy, noted in 10 cases out of 50.Only one patient had postoperative rise in IOP, other all patients were having IOP less than 20 without any antiglaucoma medications.12,13.
Table 5: Comparative Analysis Of Duration Of Symptoms and Best Corrected Visual Acuity In Post Operative Period
Duration of symptoms and BCVA had positive correlation. Earlier reported patients had better visual acuity as IOP was controlled earlier8 with less number of complications. Patient reported late found to have optic disc changes due to persistently raised IOP for longer duration.
Table 6: Analysis of effect of preoperative iop during admission and average best corrected visual acuity in postoperative period
Preoperative IOP also influenced best corrected visual acuity. Lesser rise in IOP at time of admission had better vision8 in postoperative period. Higher IOP at time of admission was controlled with use of Mannitol, topical antiglaucoma medications and oral Acetazolamide. CONCLUSION Despite high levels of IOP at time of admission, IOP get normalised after cataract extraction. Results give us importance of early diagnosis of vision threatening lens induced glaucoma. It is important to spread awareness among patient about visually disabling cataract and early reporting if above symptoms present. Poor outcome may occur if treatment is delayed and prompt early intervention may reduce further complications. It also reflects importance of use of advances in cataract extraction surgery in preventing complications and restoring best possible vision.
REFERENCES
|
|
 Home
Home