Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 - April 2019
Open tibia fractures: Analysis of correlation between timing of intervention, mode of management and outcome
Siddalingamurthy G1, Madhukesh Rudramurthy2*, Sachin Patel3, Vijay C4, Sujana Theja JS5
1,4Associate Professor, 2Senior Resident, 3Junior Resident, 5Assistant Professor, Department of Orthopedics, JSS Medical College and Hospital JSSAHER, Mysuru, Karnataka, INDIA.
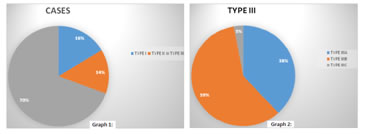
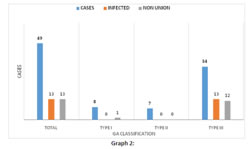
Abstract Background: Open fractures are one of the common emergencies seen in orthopaedics. The traditional teaching was that wound debridement preferably be completed within 6 hours. Current literature suggests no obvious advantage in performing debridement within 6 hours compared to debridement performed between 6 and 24 hours after injury. Our study aims to compare the outcomes of open tibia shaft fractures which were managed (i.e., initial wound debridement) within first 24hrs with those which could not be managed within first 24hrs (i.e., >24hrs) due to various reasons. Materials and Methods: A total of 49 open tibia fracture cases managed in our hospital from June 2017 to June 2018 were analysed based on the mode of injury, time from injury to intervention, method of fixation, use of antibiotics, fracture classification based on Gustilo Anderson classification for open fractures, functional outcome and development of two major complications i.e., infection and non union. All the patients underwent initial open fracture management protocol in the casualty i.e., wound irrigation, tetanus prophylaxis and i.v. antibiotics based on hospital antibiotics policy and culture swabs were taken when cases got delayed for >24hrs. The patients were divided into those operated <24hrs, 24-48hrs, 48-72hrs, 72-96hrs and >96 hrs and method of fixation i.e., IMIL nail or External fixator. Complications developed among them were analysed over a period of 6weeks, 3months, 6months and a maximum follow up of 1year. Comparison among the categorical variables was done using Chi square analysis and p value < 0.05 was considered significant. Statistical analysis was done using SPSS 16 software. Results: In previous studies, the data were based on surgical debridement done at <24 hours which showed infection rates of none to 2%, 2% to 10%, and 10% to 50% for Gustilo-Anderson types I, II, and III respectively. These values were similar in our study which showed infection rate of 0,0 and 25% when debridement was done <24hrs and 0,0 and 50% when debridement was done >24hrs for types I, II and III respectively. The data analysis done showed no correlation between type I and II open tibia fractures, timing of surgery and development of complications(i.e., p-value >0.05). Though the results were statistically insignificant (i.e., p-value >0.05) in open type III, a gradual increase in the rate of infection and non union with increase in timing of surgery in cases operated >24hrs was noted. Conclusion: Surgical debridement of open fractures should be performed as emergency for the limb salvage and better results in terms of functional outcome. But, the risk of infection and non-union is not strongly correlated to a delay to surgery. Open fracture management requires respect for several universally accepted principles in order to mitigate the risks of infection and non-union. The decision should be made on case-by-case basis, with medical optimization and trauma resuscitation always taking precedence over orthopaedic fixation and management. Key Word: Open tibia fractures.
INTRODUCTION Open fractures are one of the common emergencies seen in orthopaedics. The principles of treatment of open injuries have gradually evolved over the centuries. The management of open injuries is now in the “Era of Functional Restoration.” Functional restoration is aided by aggressive wound debridement, early definitive fracture stabilization and early wound closure or cover to achieve bone and soft tissue healing as soon as possible.1 The traditional teaching was that wound debridement preferably be completed within 6 hours. The basis of the 6-hour rule was animal studies where a threshold of 10^5 organisms per gram of tissue was found to be critical to establish infection.2 This limit was achieved in 5.17 hours. This led to the practice of debridement being done even in the middle of the night when an experienced work force was often not available. The 6-hour rule has been challenged by many recent studies.3,4,5,6,7 Current literature suggests no obvious advantage in performing debridement within 6 hours compared to debridement performed between 6 and 24 hours after injury.4The effect of delaying debridement >24 hours is however not yet clear.8 Our study aims to compare the outcomes of open tibia shaft fractures which were managed (i.e., initial wound debridement) within first 24hrs with those which could not be managed within first 24hrs (i.e., >24hrs). The primary objective was to evaluate the relationship between timing of initial wound debridement and the development of two major complications i.e., infection and non-union. The secondary objective was to compare the rate of complications according to time of debridement and grading of open fractures (i.e., Gustilo and Anderson classification for open fractures. MATERIALS AND METHODS After the institutional review board approval from JSSHER centre, we performed a retrospective review and analysis of all open tibia fracture managed in JSS Hospital Mysuru from 2015 - 2018 which accounted for 89 patients including 2 bilateral cases with 91 open tibia fractures. Information regarding the patients was gathered from the hospital register and hospital computer database. The information gathered included the patient demographics (i.e., patients name, age, sex , phone number ), mode of injury, time from injury to initial surgical management, method of fixation, use of antibiotics, fracture classification based on Gustilo Anderson classification for open fractures, number of secondary surgeries underwent and duration of hospitalisation. Patients with inadequate information in the hospital database regarding the above mentioned parameters and where excluded from the study group. This accounted for a total of 51 patients with 53 open tibia fractures were considered for further review and analysis. All the patients had underwent initial open fracture management protocol in the casualty i.e., wound irrigation, tetanus prophylaxis, i.v. antibiotics was started based on hospital antibiotics policy i.e., 2nd generation cephalosporin Cefuroxime 1.5g for open type I and II and for type III cases Amikacin 500mg and Metrogyl 500mg was added along with Cefuroxime within 1hr of presentation to the hospital, splinting of the limb and plain radiographs were taken after the patient was stabilised. The patients were taken to the operation theatre for wound debridement and stabilisation of fracture once patients were medically fit for anaesthesia and surgery. Intraoperatively fractures were classified based on Gustilo Anderson classification for open fractures and fractures were stabilised either with an external fixator
Figure 1and 2: open type iii right leg both bone fracture at the time of presentation and after wound irrigation and stay sutures in casualty; Figure 3: After Surgical Wound Debridement And Stabilisation With External; Figure 4and5: Pre Operative (Left) And Post Operative(Right) X Rays Of The Same Patient Based on the information gathered patients were divided into Gustilo Anderson groups and were subdivided based on timing of surgery from the time of injury into <24hrs, 24-48hrs, 48-72hrs, 72-96hrs, >96hrs (Table 1.) and also into <24hrs and >24hrs (Table 2.). The two major complications seen in open fractures i.e., infection and non union were assessed among these groups based on the clinical signs and symptoms and plane radiographs. For the assessment of postoperative infection clinical signs and symptoms such as fever, chills, erythema, local warmth, localized swelling, discharge from the wound, purulent localized accumulation, draining sinus and laboratory investigations which included raised ESR, CRP and total leucocyte counts were considered. In patients who developed infection, culture was taken and antibiotics were administered based on the sensitivity report. For the assessment of non union, clinical examination, plain radiographs and secondary surgical procedures undergone in view of delayed union were considered. Nonunion was defined as a fracture with no signs of bone healing or callus formation 9 months after initial management, or a fracture 6 months after initial management with no signs or progression of radiographic bone healing during 3 consecutive months.
During the process of gathering information 4 patients were lost for follow up which ended up to 47 patients with 49 open tibia fractures for further analysis. Comparison among the categorical variables was done using Chi square analysis and p value < 0.05 was considered significant. Statistical analysis was done using SPSS software.
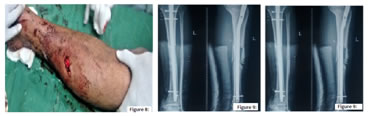
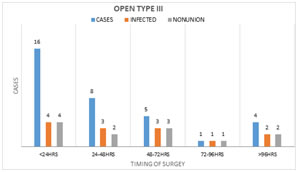
Figure 8, 9 and 10: open type ii both bone left leg fracture fixed with intramedullary nail. Wound picture and pre and post operative xrays Out of 34 cases 16(47%) cases were operated within 24hrs, 8(23.5%) cases b/w 24-48hrs, 5(14.7%) cases b/w 48-72hrs, 1(0.03%) case b/w 72-96hrs and 4(11.4%) cases >96hrs.
13 cases under grade III got infected and 12 cases went for non union, which accounted for an infection rate of 38% and non union rate of 35% in grade III cases. In cases operated within 24hrs,24-48hrs,48-72hrs,72-96hrs and >96hrs the number of cases which got infected were 4(25%),3(37.5%),3(60%),1(100%),2(50% )respectively and number of cases which went for non-union were 4(25%),2(25%),3(60%),1(100%),2(50%) respectively.(Graph 4.) Table 1:
When only 2 groups were considered i.e., <24hrs and >24hrs; the infection and nonunion rate was 25% and 25% respectively in <24hrs group and 50% and 44.4% respectively in >24hrs group. In 13 cases under grade IIIA, none of the 6 cases operated <24hrs developed any complications. In the rest 7 operated >24hrs 3(42.8%)developed infection and 2(28.5%) went for nonunion. In type IIIB out of 20 cases 9 were operated <24hrs and 11 cases >24. Infection and non union rate among these two groups were 44.4% and 44.4% in <24hrs group and 54.5% and 54.5% in >24hrs group respectively. (Table 2., Graph 5. and 6.) Table 2:
There was only one case of open type IIIC which eventually underwent amputation due to unsuccessful vascular repair. The statistical Chi square analysis comparing the infection and non union rate among the categorical variables showed no statistical significance i.e., p value was >0.05.
DISCUSSION Current literature suggests no obvious advantage in performing debridement within 6 hours compared to debridement performed between 6 and 24 hours after injury.4 Current guidelines suggest open fractures should be debrided within 24 hrs from the time of injury. The management of these open fractures i.e., the time to the first surgical debridement, sometimes gets delayed for >24hrs. Reasons for delayed debridement include late presentation to the trauma care centre due to lack of transportation in rural areas, lack of trauma surgeons in the periphery, delay in transfer from periphery to trauma care centre, need for medical optimization and clearance for surgical treatment and other life threatening injuries which needs first priority. These patients who underwent surgery after 24 hrs from the time of injury due to various reasons, needs to be evaluated to correlate the complications of late wound debridement and to recommend any changes in the management protocol in these patients if needed. The data collected by us and the analysis done showed no correlation between type I and II open tibia fractures, timing of surgery and development of complications(i.e., p-value >0.05). Though the results were statistically insignificant (i.e., p-value >0.05) in open type III, a gradual increase in the rate of infection and non union with increase in timing of surgery in cases operated >24hrs was noted. In type IIIA, all cases operated <24hrs showed no development of complications whereas those operated >24hrs showed infection and non union rate of 42.8% and 28.5% respectively. In type IIIB there was a 10% increase in the rate of infection and non-union when operated >24hrs when compared with those cases which were operated <24hrs. In previous studies in which the data were based on surgical debridement done at <24 hours after injury showed infection rates of none to 2%, 2% to 10%, and 10% to 50% for Gustilo-Anderson types 1, 2, and 3, respectively.9,10 These valueswere similar in our study which showed infection rate of 0,0 and 25% when debridement was done <24hrs and 0,0 and 50% when debridement was done >24hrs for types I, II and III respectively.
CONCLUSION Open fracture management requires respect for several universally accepted principles in order to mitigate the risks of infection and non-union. The key elements in managing open fractures of tibia include prompt and earliest antibiotics initiation, debridement, skeletal stabilization and early soft tissue cover.11Advances in surgical, microbial, and pharmacological understanding have contributed to changes over time in these principles. Surgical debridement of open fractures should be performed as emergency, but the risk of infection and non-union is not strongly correlated to a delay to surgery.12 Weber et al. (2013)in their prospective cohort study of 736 subjects with 791 open fractures concluded that “Development of deep infection after open fracture was not associated with time to surgery; instead increasing Gustilo grade or tibial/fibular fractures were associated with developing a deep infection.”13The timing of debridement in open fractures is a controversial topic. Strict observance of a 6 hour cut off, however, has not borne out in the clinical evidence, with the severity of traumatic injury, anatomic location of injury (especially tibia), and patient comorbidities being more predictive of infection risk. 9, 14, 15, 16-18 Based on our study results, we would like to conclude that timing of wound debridement does not affect the results in Gustilo Anderson open type I and II fractures. In open type III, timing does affect the results with increasing rate of infection and non union with increase in timing of initial wound debridement. In these cases early debridement is recommended, but the quality of wound debridement and early administration of antibiotics as per protocol does have an equal weightage. The decision should be made on case-by-case basis, with medical optimization and trauma resuscitation always taking precedence over orthopaedic fixation.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home