Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 - May 2019
Short term functional and neurological outcome of short segment pedicle screw fixation in unstable thoracolumbar burst fractures
Gurumurthy B1, Madhukesh Rudramurthy2, Sujana Theja J S3, Manjunatha D N4
1,3Assistant Professor, 2Senior Resident, 4Junior Resident, Department of Orthopedics, JSS Medical College and Hospital JSSAHER, Mysuru, INDIA.
Abstract Background: Burst fractures are the most common type of thoracolumbar spine fractures (21-58%) associated with kyphotic deformity and neurological deficits. The treatment goals include restoration of spinal stability, kyphotic deformity correction and decompression of the spinal canal. Short segment pedicle screw fixation has become an increasingly popular, most common and simple method of treatment of thoracolumbar burst fractures, providing the advantage of incorporating fewer motion segments in the fixation and also prevents excessive loads on the adjacent discs. Methodology: It is a prospective study between January 2015 to January 2018, included a total of 60 patients who were operated with short segment pedicle screw fixation for unstable thoracolumbar burst fractures with TLICS score 4 or more than 4. Neurological evaluation was done using American Spinal Injury Association (ASIA) grading and fracture classified using AO classification. Sagittal Angle (SA) and Sagittal Index (SI)were calculated in plain radiograph of the TL spine pre-operatively, post-operatively and at final follow-up. All patients were followed up post operatively at 1,3,6 and 12 months for neurological and radiological evaluation. Results: Our study threw light on many aspects of thoracolumbar burst fractures. Fall from height was the most common mode of injury, followed by motor traffic accident. T12 vertebra was the most common level of incidence with 31.6% followed by L1 vertebra at 26.6%.34 patients had A3 type of AO fracture and 26 patients A4 type. Out of the 60 cases,12 had complete neurological injury (ASIA A), 48 had incomplete injury (ASIA B,C,D). 4 cases(33%) among complete neurological injury had improvement by one grade and 2cases (16.6%) had improvement by two grade in ASIA charting. Among 48 incomplete injuries 27 (56.25%) showed two grade improvement and 20patients (41.6%) showed one grade improvement at final follow up. Sagittal Angle (mean) improved from 21.80 to 9.460 immediate post-op and a gradual decrease of 1.70 noted at final follow-up. Conclusion: Short segment pedicle screw fixation without fusion is a safe and effective method as it achieves good stabilization with comparableneurological recovery, when addressed at the earliest. Short segment pedicle screw fixation also provides chance for early mobilisation thereby reducing the complication associated with long term recumbent bed rest in patients with unstable thoracolumbar fractures. Comparable Sagittal angle and sagittal index can be achieved to near normal by this method, maintaining the spinal curvature thereby by-passing associated complications of long segment fixation. Key Word: pedicle screw fixation.
INTRODUCTION Burst fractures are the most common type of fracture of the thoracolumbar spine, accounting for 21% to 58% of all thoracolumbar spinal fractures1. These are repeatedly associated with kyphotic deformity and neurological deficits. Burst fractures are very common in young working age group population and could have a great impact on their daily physical activities. Even though debate on operative and non operative management for thoracolumbar fractures exist, the added advantage of operative management for unstable thoracolumbar burst fractures like restoration of spinal stability and alignment, correction of kyphotic deformity and decompression of the spinal canal is commendable4,5,6. The added advantages of surgical treatment with pedicle screw and rod fixation system are shorter hospital stay, fewer complications of prolonged immobilization, complete rehabilitation and reduced morbidity and mortality7. Minimizing the number of vertebral levels involved in fusion of a spine fracture is a common goal of internal fixation, this is achievable by utilizing traditional short-segment posterior fixation (SSPF). SSPF is the use of pedicle screw instrumentation one level above and one level below the fractured vertebra. It has become an increasingly popular, most common and simple method of treatment of thoracolumbar burst fractures, providing the advantage of incorporating fewer motion segments in the fixation and also prevents excessive loads on the adjacent discs 8-11. The maximal mechanical stabilization of unstable thoracolumbar burst fractures, particularly with compromised bone quality, requires instrumentation at least 2 levels above and below the level of injury (Long segment fixation) 13-16. The biomechanical advantage of long segment fixation is countered by the negative effects of fusing multiple motion segments. In the present prospective study, we aimed to evaluate the overall clinical, radiological, as well as functional outcomes in patients with unstable thoracolumbar fractures managed by posterior instrumentation of the spine using the short segment pedicle screw fixation.
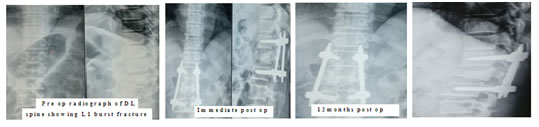
MATERIALS AND METHODS This is a prospective interventional study, conducted in JSS Medical College and Hospital from January 2015 to January2018, after obtaining clearance from institutional ethical committee. A total of 60 patients who had acute unstable thoracolumbar fractures within age group between 18 to 60 years, Thoracolumbar injury classification (TLIC)score 4 and more than 4 were included. Patients with multilevel spinal injuries, patients not fit for surgical intervention with associated other systemic injuries were excluded. A detailed history and clinical examination carried out. American Spinal Injury Association (ASIA) scale was used to evaluate neurological injury and fractures classified according on AO classification. Plain radiographs whole spine were taken to assess for the type of fracture, radiological evaluation done by measuring sagittal angle and sagittal index. ASIA grading used to evaluate neurological deficits and the level of neurological injury. Posterior approach was used to expose the DL-spine. Patients positioned prone over the bolsters under the chest and pelvis, with the abdomen hanging free, to reduce excessive intra-operative bleeding and to achieve a significant initial reduction of the spinal fracture. Image intensifier used to identify the fracture level and fracture reduction. In our study, Weinstein method of pedicle screw entry was preferred for Lumbar vertebra and Roy-Camille technique of pedicle entry for thoracic vertebra in all the cases. Free hand technique used for pedicle screw instrumentation, later position of screws confirmed with an image intensifier. Pedicle and the vertebral body were tapped to at least one half of the depth of the vertebral body using a tap for the screw diameter chosen from pre-operative pedicle measurements. Poly-axial pedicle screws of 6.5 mm (diameter)*40/45 mm (length) are used. Once all the screws have been placed, proper length rod selected and contoured to maintain normal lumbar lordosis. Rods inserted and reduction of fracture achieved by distraction technique and assembly fully tightened. Laminectomy is performed in all cases with neurological deficits to decompress the Dura and roots. Patients were made to sit bed side by 2nd post-operative day. Bed to chair mobilization was initiated on 5th post-op day. Check radiographs were taken on postoperative day 2 for evaluation of fracture reduction, implant position, sagittal angle and sagittal index. All patients were started on a rehabilitation program with the help of a physiotherapist for passive mobilization of lower limb joints, strengthening of upper limb muscles. Patients with partial neurological deficits were mobilized from 5th post-operative day has permissible with walker. Patients were followed up at 1, 3, 6, and 12 months. At every follow-up patients were assessed for neurological improvement using the ASIA grading. Radiographs were taken for the evaluation of sagittal angle, sagittal index and pedicle screw position. The data obtained was entered in a spread sheet and analysed using Independent t-test for quantitative variables, paired t-test for paired observation and chi-square test for categorical observations. All the values below 0.05 were considered statistically significant. Case 1:
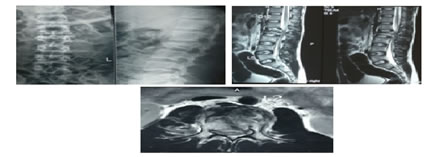
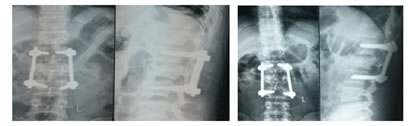
Pre-operative DL-spine x ray, MRI - sagittal and axial images showing burst fracture of L2 vertebra with PLC disruption, compressing on nerve roots. 18months follow-up Post-operative Radiographs showing improved sagittal angle and sagittal index with good position of pedicle screws and rods. Post-operative clinical pictures at 18months showing good range of flexion and extension movements at DL spine.
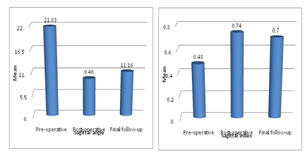
RESULTS 60 patients were evaluated in the study,51 males and 9 females. The mean age was 34 years. The most common mode of injury was fall from height 53 patients(88%), followed by motor traffic accidents 7 cases (12%). Most common level of injury was at D12 (19 cases) and L1 (16 cases) junction combined accounting to 58.3% of the cases and12 patients(20%) had injury at L2 level. Out of 60 patients, 34 patients had AO type A-3 fracture and 26 had A-4 fracture.. 31 patients were operated within 24 hours of injury and 23 patients were operated within 1-3 days after injury, Mean injury to surgical interval was 1.86 days(1-3 days). Out of the 60 cases,12 had complete neurological injury (ASIA A), 48 had incomplete injury (ASIA B,C,D).4 cases(33%)among complete neurological injury had improvement by one grade and 2cases (16.6%) had improvement by two grade in ASIA charting. Among 48 incomplete injuries 27 (56.25%) showed two grade improvement and 20patients (41.6%) showed one grade improvement at final follow up, which had statistically significance with p value < 0.01 Mean sagittal angle calculated pre-operatively was 21.830, which improved to 9.460 in immediate post-operative radiograph. The mean difference in the sagittal angle between pre-operative and immediate post-operative radiograph was 12.370and between post-operative and final follow-up was 1.70. Mean sagittal angle at final follow-up was 11.160. Mean sagittal index calculated pre-operatively was 0.48, which improved to 0.74 in immediate post-operative radiograph and reduced to 0.7 at the final follow-up. There was no statistically significance among radiological evaluated data, with p value of >0.01
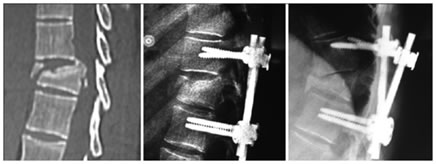
Three patients had implant failure , among them one patient with screw back out and increasing kyphotic deformity and detioration by grade one from ASIA grade D to Grade C at 3 months was observed. The above patient underwent revision procedure with implant removal and spanning instrumentation 2 level above and below. 2 patients had implant failure with screw backout and screw breakage at 9 months, both of them underwent implant removal and managed with extension brace
DISCUSSION The common consensus regarding operative management of Burst fracture of Thoracolumbar region is still a debatable topic in many forum. In our study 58.2% of fractures occurred at D12 and L1 junction, which were comparable with the studies of Roop Singh et al (57.6%)15 and Sharvil H. Gujjar et al (53.05%)17. Among 60 cases studied, 12 had complete neurological injury (ASIA A), 48 had incomplete injury (ASIA B,C,D).4 cases(33%)among complete neurological injury had improvement by one grade and 2cases (16.6%) had improvement by two grade in ASIA charting. Among 48 incomplete injuries 27 (56.25%) showed two grade improvement and 20patients (41.6%) showed one grade improvement at final follow up. The mean sagittal angle calculated pre, post-op, at final follow-up was 21.830, 9.460, 11.160 respectively which are comparable to the study done by Mohammad F. Butt et al (21.40, 12.80, 16.20) (12) and Muralidhar B.M. et al (23.50, 10.750, 15.50)16. The mean sagittal index calculated pre, post-op and at final follow-up was 0.48, 0.74, 0.7 respectively which are comparable with the values of Mohammad F. Butt et al study (0.44, 0.72, 0.69) and Muralidhar B.M et al study (0.53, 0.75, 0.72)12.The post-operative near normal values of mean sagittal angle and mean sagittal index achieved gives commendable outcome of short segment fixation technique. The neurological recovery rates found to be similar in patients who were operated <24 hours of injury and patients operated >3 days after the injury. There was no injury- surgical interval showed no significant difference. 3 cases (5%) having implant failure in the form of screw back out or breakage, probably as observed related to fracture configuration with 1 patient at T12 level and 2 patients at L1 level. These patients had immediate post operative good achievement of sagittal index and sagittal angle, however at follow up by 1year there was increase in sagittal index and sagittal angle . The D12 and L1 region being the transition zone, increased kyphosis and early forward bending by the patient who were manual labourer by occupation can be attributed to the cause of failure of implants.
CONCLUSION Fractures of thoracolumbar spine are the most common type of osseous spine injuries. The main aim of treatment resides in early stabilization of the fracture, direct or indirect decompression of the neural elements and early mobilization of the patients to prevent complications. This also avoids the burden on the family of the patient and the care givers12. It reduces the hospital stay compared with that of conservative methods of treatment. Incomplete burst fractures were the most common type of fracture encountered in the study which leads to deformity and neurological compromise. The radiological and neurological evaluations were the parameters taken into account to assess the instability, indication for surgery and recovery. There was a marked improvement in the radiological parameters comparable to other studies done in both Western and Asian countries. The neurological improvement was observed to be fair in cases of complete neurological injury and significant improvement in cases of incomplete neurological injury. Short segment pedicle screw fixation without fusion is a safe and effective method as it achieves good stabilization with comparable neurological recovery, when addressed at the earliest. Short segment pedicle screw fixation also provides chance for early mobilisation thereby reducing the complication associated with long term recumbent bed rest in patients with unstable thoracolumbar fractures. Comparable Sagittal angle and sagittal index can be achieved to near normal by this method ,maintaining the spinal curvature thereby by-passing associated complications of long segment fixation. However the role of short segment fixation in osteoporotic patients and long term follow up is necessary for more strong evidence.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||
 Home
Home