Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 - May 2019
V S Ravindranath1, B Sreekanth Rao2*
1,2Professor, Assistant Professor, Department of Orthopaedics, Bhaskar Medical College, Yenkapally,Hyderabad, Telangana, INDIA. Email:bsreerao@gmail.com
Abstract Background: In the past the most common surgery around the hip was DHS and Barrel plate for any trochanteric fractures. Of late the commonest surgeries done on the Femur are Proximal Femoral Nail (PFN) or the Interlocking Nailing for the fractures of the Femur or supracondylar nailing of the Femur. Aim: To study the advantages of the new device for percutaneous entry point in Greater Trochanter for any intra medullary fixation of the Femur compared to the conventional methods. Objectives: To access advantages of this new device over the conventional device used for the intramedullary femur entry point. The following intraoperative characteristics were compared by usage of new device and conventional device.1)C-Arm exposure time, 2)Technical difficulties during surgery along with complications, 3)Duration of surgery, 4)Blood loss, Materials and Methods: A total of sixty four cases are being treated from November 2017 to October 2018 at Bhaskar Medical College and Bhaskar General Hospital Yenkapally, thirty two cases each by this method of percutaneous entry point in the Trochanter using this new device and conventional device respectively for the Trochanteric fractures and for the fractures of shaft of the Femur. The device is designed by the author and his team indigenously in the work shop of the Mechanical engineering of Joginpally Institute of Engineering and Technology. All the patients gave the informed consent for inclusion into study and the study was authorized by the local ethical committee. Results: We have done this study in 64 patients, 32 patients each by new device and conventional device respectively. With the use of new device, there was ease getting into the exact point of entry in the Trochanter, the comfort of getting both AP and Lateral views of the C- arm pictures with avoidances of unnecessary exposure to radiation and minimal blood loss compared to the use of conventional device. Conclusion: The study has found that the new device is very effective and advantageous compared to the conventional device for percutaneous entry point in Greater Trochanter for any intra medullary fixation of the Femur Key Word: New device, entry point, Greater Trochanter.
INTRODUCTION The Trochanteric fractures and shaft of the Femur are very common injuries in both young as well as geriatric people. The intra medullary fixation of these fractures gives a stable fixation so as to mobilize these patients very early. All these surgeries are done on a fracture table and under imaging. The entry point in the Trochanter varies in different types of the fractures i.e. lateral to the tip of the Trochanter, medial to the tip of the Trochanter and sometimes through the piriformis fossa. Once if the entry point is made with the conventional Trochanter awl, it becomes very difficult to change direction of the tract in the Trochanter and it takes lot of time to change the entry point and also one gets exposed to radiation unnecessarily, more blood loss. The new device developed by us is very simple, surgeon friendly and less exposure to the radiation. Design of the device The device has three parts:
The device is designed from and manufactured from 316 SS metal.
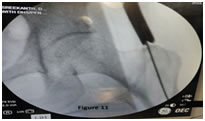
cannulated conical cylinder is curved long horizontal handle of 10mm diameter 3 mm diameter bar fixed to the horizontal rod again at right angle. Bio mechanics of the Device: The conical cylinder has got a proximal end and a distal end. The distal end has three teeth (Fig.3) which can rest on to Greater Trochanter firmly by gently tapping. The device can rest on the tip of the Greater Trochanter, lateral to the tip of the Greater Trochanter and also in the Piriform fossa. Moving the conical cylinder in coronal and sagittal planes facilitates the exact direction of the entry of the guide wire even before the Greater Trochanter is pierced (Fig 4,4A). The curvature facilitates an easy entry of the guide wire. Moving the conical cylinder in coronal plane The long handle is always stays away from the coronal plane the body (Fig. 5). Moving the handle in sagittal plane can change the location of the guide wire to be placed exactly in the center of the Intramedullary canal of the Femur even before the Greater Trochanter is pierced (Fig.6).As the handle is away from the body (fig.7) it is very easy to take the lateral view of the hip joint along with the Greater Trochanter to check the guide wire placement in the intramedullary canal of the Femur. Figure 5,6: The long handle is always stays away Greater Trochanter is pierced sagittal planefrom the coronal plane the body Figure 7: Handle is away from the body Surgical procedure: Procedure: All the 64 cases were admitted in the Emergency ward on the arrival. The cases were worked up for the fitness for Anaesthesia as well as for surgery. The patient was anaesthetized and shifted on to the fracture table. The fracture was reduced and the reduction was confirmed in AP and Lateral views by the imaging by C-arm. After scrubbing a 10 to 12 mm incision was made just proximal to the tip Greater Trochanter (Fig.8A). Incision of 20mm to 30mm was made when we used conventional awl. The new device was introduced to reach the tip of the Greater Trochanter. The position and the direction of the device for the entry point of the guide wire were confirmed in both views before penetrating the Greater Trochanter under C-arm (Fig.9). The ease, at which the lateral view was taken, is evident in the picture (Fig.10). Then the guide wire was passed with ease making a perfect entry in the Greater trochanter(fig11). The rest of the surgical procedure was done as usual. Figure 8:10 to 12 mm incision Figure 9,10 :Guide wire were confirmed in both viewsEaseofthe lateral view
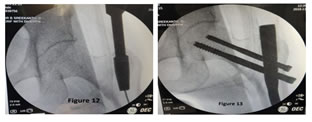
Figure 11:Guide wire was passed with easeFigure 12: The Greater Trochanter was reamedFigure13:Final post operative image For patients where we used conventional device the incision for entry point was 15mm to 20mm.
RESULTSWe have done this study in 64 patients. 32 patients each with new and conventional device respectively.The exact point of entry in the trochanter achieved with ease in shorter duration of time with new device. There was comfort with new device in getting both AP andlateral views of the C- arm pictures with avoidances of unnecessary exposure to radiation. Abductor power was normal in 30 patients when entry point made with new device and power 4 with conventional device in 31 patients. With use of new device, blood loss was minimal, wound healed well with a small scar with new device. These patients were in the age group of 22 to 75 years. There were 52 males and 12 females (Table .1).
Table 1:
The types of the fractures were Inter Trochanteric (58no) and Subtrochanteric fractures (6no).
Table 2:Outcome with our new Devise Outcome with conventional Device
DISCUSSION Worldwide literatures now support that intramedullary implant as better implants than extra-medullary implants in management of intertrochanteric fractures. Theoretically, there is an improved biomechanical environment with an intramedullary device, with a shorter lever arm, which provides more load sharing and allows less collapse for a stable medial configuration1. Intramedullary implants commonly used are Gamma nails, Proximal Femoral Nails,Trochanteric and Femoral antegrade nail,Supracondylar nail,Enders nails,Recon.The intramedullary nails are indicated for fractures of the femur, intertrochanteric, femoral neck fractures, subtrochanteric fractures, ipsilateral femoral neck/shaft fractures, stable and unstable shaft fractures, segmental fractures, nonunion, malunion, reconstructions, bone lengthening, shortening and polytrauma. Patient positioning: The patient in supine position on a fracture table. The foot of the fractured leg is placed in a foot/boot holder. The unaffected/opposite leg is extended below and away from the affected/fractured limb. The affected/fractured limb is assessed for length and rotation. Measurements of the opposite/ unaffected limb well recorded for assessment. Trunk is abducted 10°-20° to allow easy access to the entry point into the intramedullary canal. ‘C’ position on fracture table with eccentric perineal post and 5°-10° adduction fracture is reduced on fracture table. In intertrochanteric fractures if the proximal fragment is displaced posteriorly we tilted the pelvis superiorly by 10°-20° to align the fragmentsin anatomical reduction which made the procedure simpler by easy entry into medullary canal by my new devise.A trochanteric overhang may result in a much more medial entry point than intended, which may increase the risk of additional fracture or avascular femoral head necrosis2C-Arm operated by trained assistant AP and lateral visualization of the entire femur with optimal positioning keeping in mindfor minimal exposure to radiation of C-Armand shorteningthe duration of surgery. Incision and entry point: A longitudinal incision10mm to12mm is made proximal to the greater trochanter.The incision extended through the fascia and tip of the greater trochanter is palpated. The ideal entry point is located lateral to the tip of the greater trochanter, approximately 5° from the anatomical axis in the AP view and in-line with the intramedullary canal in the lateral view. The entry point for the Recon/Femoral antegrade nail is via the piriformis fossa, in-line with the femoral intramedullary canal in the AP and the lateral views, here the entry point is slightly posterior in the lateral. Gausepohlet al. (2002) recommended the piriform fossa as the correct entry point for straight nails; bent nails should be implanted more dorsally3. Entry portal acquisition: The new device was introduced to reach the tip of the Greater Trochanter. The position and the direction of the device for the entry point of the guide wire were confirmed in both views before penetrating the Greater Trochanter under C-arm (Fig.9). The ease, at which the lateral view was taken, is evident in the picture (Fig.10). Then the guide wire was passed with ease making a perfect entry in the Greater Trochanter (Fig.11). An incorrect entry point may lead to tensions in the implant-bone interface, inducing additional iatrogenic fractures3.The risk of cut-out is directly dependent on the quality of fracture reduction and on implant position4. In AP view entry point to be more medial. This allows 2 screws in head in good position5. If starting/entry point is placed more lateral to the tip of the trochanter it may result in varusmalreduction6,7A slightly anterior entry point in the lateral projection could prevent hitting the anterior cortex while adducting the limb and keeping the nail insertion device handle as close to flank as possible will help to prevent breach of the medial cortex. The AO study group noted that ‘‘the nail should not be introduced through the top of the greater trochanter, but somewhat more laterally, so that neither the retinacular vessels nor the hip joint are damaged8.With limited access approach, one can reduce the blood loss, soft tissue trauma and infection9Three entry portals were defined. (A)entry portal lateral to the junction of the neck and the greater trochanter; (B)entry portal at the base of the greater trochanter anterior to a line along the longitudinal axis of the femoral neck; and (C)entry portal at the base of the greater trochanter posterior to a line along the axis of the femoral neck (at the piriformis fossa).We need to respect the soft tissue and neurovascular structures at entry point to femur as little attention is paid to insertion site morbidity associated with antegrade femoral nailing. In a study made by Dora. Entry point soft tissue damage in antegrade femoral nailing: a cadaver study10, performed dissection of the proximal part of the femur to assess possible damage to the soft tissues. Three entry portals were defined, Group A, partial avulsion of the piriformis and the obturator internus tendon were present in four and in one of five specimens, respectively. Group B showed injuries to the piriformis tendon in two and to the gluteus minimus tendon in one of four cases. In Group C, partial avulsion of the piriformis, obturator internus, and obturator externus tendon were encountered in five, six, and two of seven specimens, respectively. Anterior branches of the ramus profundus of the medial femoral circumflex artery within the synovial fold were damaged in all of these cases 10 Our new devise safe guards the soft tissue, minimizes radiation and blood loss, reduced trial and error method to find the entry point. It is patient and surgeon friendly devise.
SUMMARY AND CONCLUSION It is very important to select the best nail entry portal, the ease of nail insertion must be considered against the resulting soft tissue damage at the site of insertion. The nail entry portal at the piriformis fossa, although geometrically ideal and most recommended, causes the most significant damage to muscle and tendons as well as to the blood supply to the femoral head10. We need to respect the soft tissue and neurovascular structures at entry point to femur as little attention is paid to insertion site morbidity associated with antegrade femoral nailing. Ease of finding the entry portal with our new device has minimized soft tissue damage, negligible blood loss, shortened the duration of surgery, comfortable positioning of device and passing guide wire in lateral position viewing under C-Arm, reduced exposure to radiation, small healthy surgical scar. Our device compared to conventional device is patient and surgeon friendly device.
REFERENCES
|
|
 Home
Home