Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 - May 2019
Adult distal humerus trauma: Study of epidemiology and surgical intervention
Rajesh K Ambulgekar1, Kapil R Saoji2*
1Professor & HOD, IIIrd Year Resident, Department of Orthopaedics, Dr Shankarrao Chavan Government College and Hospital Nanded, Maharashtra, INDIA. Email: drkapil.saoji@gmail.com
Abstract Background: Fractures of the distal humerus comprised of approximately 2% of all fractures and one-third of all humeral fractures. The epidemiology of these fractures is well known in children, but it is not well described in adults. Aim: To study the epidemiology and surgical intervention with open reduction and internal fixation with bicolumnar plating by extensor mechanism sparing paratricipital approach. Material and Methods: In this prospective study all patients with distal end humerus fracture were studied and managed with open reduction and internal fixation with bicolumnar plating by extensor mechanism sparing paratricipital approach. Results: Majority of cases i.e. 17 (56.67%) were in the age group of >30 years. The minimum age of the patient was 18 years and maximum was 72 years with mean age of 38.77 years. Males were more common patients with intercondylar humerus fracture accounts for 56.67% of the cases. Right side has a marginal high predominance than Left side. Conclusion: Distal humerus fractures are relatively uncommon in adults but are increasing in frequency. Most of the fractures are common in mean age group of 38.77 years, occurred more in males with road traffic accident as most common cause. Key Word: Distal humerus fractures, adults, bicolumnar plating by extensor mechanism, epidemiology.
INTRODUCTION Fractures of the distal humerus comprised of approximately 2% of all fractures and one-third of all humeral fractures.1,2 The epidemiology of these fractures is well known in children, but it is not well described in adults.3,4 These fractures occur because of low-energy trauma in elderly patients. The incidence of distal radius fractures peaks in younger individuals who injure themselves through sports and road-traffic accidents and in the elderly population, in whom osteoporotic fractures are often due to simple falls.5 Distal humeral fractures in adults tend to progress to non-union or functional impairment when managed nonoperatively.6 The management of distal humeral fractures has evolved over the years from non-operative treatments to operative treatments. Distal articular humerus fractures are preferably treated by open reduction and internal fixation. Olecranon Osteotomy approach has been the gold standard amongst surgical approaches for fracture fixation of the distal articular surface of humerus.1,7,8 It is the most commonly used surgical approach and provide good visualization of the fracture.8 But this approach has many complications. To avoid the complications an extensor mechanism sparing Para tricipital posterior approach to distal humerus through midline posterior incision was suggested by Schildhauer et al.9 The study was conducted to study the epidemiology and surgical intervention with open reduction and internal fixation with bicolumnar plating by extensor mechanism sparing paratricipital approach.
MATERIAL AND METHODS In this prospective study all patients with distal end humerus fracture were screened using the inclusion and exclusion criteria. Informed consent was taken for all patients and approval of the Institutional Review Board was obtained prior to the commencement of the study. Inclusion Criteria
Exclusion Criteria
Detailed history regarding the etiology of the fracture, associated injuries was taken from the patient. General examination along with physical examination of the corresponding shoulder, elbow and wrist joints was carried out. Investigations were done in the form of elbow X-rays (AP and lateral views; both oblique views if required) and were evaluated. Fractures were classified based on the AO classification. Primary management was done and fracture immobilization in above elbow slab up to mid-arm level and the patient was shifted to ward with elevation of the affected upper limb. Patients included in the study were treated with open reduction and internal fixation with bi-columnar plating by extensor mechanism sparing paratricipital approach, and were assessed intra-operatively for blood loss, fracture reduction and articular continuity under the image intensifier (C-arm). Patients were followed up post-operatively at 1 month, 2 months, 6 months after treatment, and were evaluated clinically by Mayo Elbow Performance Score at each follow-up visit, along with X-rays (AP and lateral views). Secondary outcome measures used consisted of Elbow pain, Active and passive ROM (flexion, extension) of both elbow joints using a universal goniometer, Disability in performing daily activity and Complications (infection, neurovascular compromise, stiffness, subsequent or secondary intervention, arthritis). X-rays (antero-posterior and lateral views) were evaluated on every follow up for the signs of fracture healing and hardware failure or any other complications. Union was defined as the presence of bridging callus or the disappearance of the fracture line on three of four cortices seen on the anteroposterior and lateral radiographs.
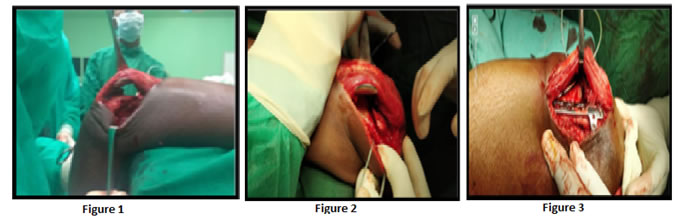
Figure A, B, C: The lateral column plating
RESULTS A hospital based prospective study was done with 30 patients with Fracture of Distal Humerus in adults treated with open reduction and internal fixation with Bicolumnar Plating by Extensor Mechanism sparing paratricipital approach.
Table 1: Patient characteristics
Majority of cases i.e. 17 (56.67%) were in the age group of >30 years. The minimum age of the patient was 18 years and maximum was 72 years with mean age of 38.77 years. Males were more common patients with intercondylar humerus fracture accounts for 56.67% of the cases. Right side has a marginal high predominance than Left side.
Table 2: Distribution of fracture type: AO Classification
Majority of the cases studied were type A2 (30%) followed by type A3 (20%) supracondylar humerus fracture. In our study we used Mayo elbow score for functional outcome. At the end of 6 month follow up as per Mayo Elbow Performance Score, we found excellent result in 26 patients, Good result in 3 patient and Fair result in 1 patient. Using Mayo elbow score we had more than 96% excellent to good results with mean score of 95.46. We did not have any poor results at the end of 6 month follow up. Since we could achieve good reduction, stable fracture construct, early rehabilitation we were able to get functional range of motion of 94-166 degrees in most of the patients, and thus our functional outcome measures were also good. DISCUSSION Distal humerus fractures account for 1–2% of all fractures in adults,10 but the incidence varies between countries. In 2003, the incidence was 6/100,000 per year in the United Kingdom.11 The incidence was 0.5% (5.8/100,000) in 2000 at an Edinburgh (UK) trauma unit, with nearly three-quarters of the fractures occurring in women.12 The fracture distribution curve showed a unimodal distribution in older women that corresponded to osteoporotic fractures. In our study the mean age was 38.77 years ranging from 18 years to 72 years, which was comparable to other studies by Ali et al (mean - 32.5 years),13 Patel et al (mean - 35 years)14 and Mondal et al (mean - 32.89 years).15 Out of 30 patients 17 patients (56.67 %) were males and 13 patients (43.33 %) were females in our study. The sex ratio was inclined towards males in most other studies too. The male ratio in our series was higher, which could be attributed to the Indian social pattern, where males were generally more engaged in outdoor activities and driving automobiles, thus exposing them to a greater risk. Ali et al (males 72.72% vs females 27.27%)13 and Yadav et al (males 64% vs females 36%)16 also found males as majority cases in their study. In our study with right side involvement was in 20 (66.67%) patients and left side involvement in 10 (33.33%) patients. Involvement of both side were comparable with Patel et al and Mondal et al who observed left side involvement in 70% cases.14,15 In our study, road traffic accidents accounted for 18 patients (60%) and fall accounted for 12 patients (40%). Therefore, road traffic accident was the major contributor to these fractures in our study and this could be well explained from increased use of high velocity vehicles especially two wheelers and also this was comparable with the literature. The main etiology identified in literature for the mode of trauma were road traffic accident and fall. Table 3: Mode of trauma in studies by other authors
The common fracture type (AO classification) we accounted in our study were Type A2 which was in 9 patients (30 %) and Type A3 which was also in 6 patients (20 %), Type B1 in 3 patients (10%), Type B2 in 3 patients(10%), Type B3 in 4 patients(13.33%), Type C1 in 2 patients(6.67%) and Type C2 in 3 patents(10%). This distribution was comparable to the study by Mondal et al where 50% fractures were Type A, 33.33% fractures were Type B, 10% of fractures were Type C1, 6.66% of fractures were Type C2.15 Patel et al accounted for 9 cases (22.5%) of type A, 5 cases (12.5%) of type B, 26 cases (65%) of fractures of type C.14 Previous investigators of triceps-splitting or peeling approaches had postulated a negative effect on muscle strength on the basis of the potential for weakened reattachment, direct muscle injury with resultant fibrosis, and injury to intramuscular nerve branches. Our results compared favourably with other studies utilizing different approaches, as this approach maintained the triceps attachment to the olecranon, eliminated the need for triceps repair and protection postoperatively, allowed active range of motion in the injured elbow. Restoration of the articular surface was the most important step followed by stabilization of the largest columnar fragments. Several options were available for fixation, these include the use of Y-shaped plates, reconstruction plates, LC-DCP, single plates, pre-contoured locking distal humerus plates. The aim was to achieve the stable reconstruct. At the end of 6 month follow up in our study, the mean range of motion of elbow was 141.5 degree (94- 166o). In our study we found that there is significant difference between mean ROM at POD 1 to 1 month, 1 month to 2 months and 2 month to 6 month follow up. In the study of Mondal et al,15 the median arc of elbow motion was 115 degrees (range 70 to 140 degrees) with standard deviation of 1.33. Arc of motion >120 degrees seen in 66.66% of patients, arc 90-120 degrees present in 23.33% of cases, arc <90 degrees seen in 10% of cases. In the study of Patel et al,14 24(60%) patients could move their elbow with an arc of 50-100 degrees and 4(10%) patients could move their elbow with an arc of less than 50 degrees, 12(30%) patients could move their elbow with an arc of more than 100 degrees. In the study of Yadav et al,16 mean motion arc was 114.92°(range 65°-140°).
CONCLUSION Distal humerus fractures are relatively uncommon in adults but are increasing in frequency. Most of the fractures are common in mean age of 38.77 years, occurred more in males with road traffic accident as most common cause. Despite recent treatment advances, management of distal humerus fractures in the elderly remains one of the most challenging aspects of trauma surgery.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home