Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 1 - July 2019
Analysis of correlation between complex regional pain syndrome and fracture distal radius reduction method
Abdul Hameed Ansari1, A V Shabi2*
1,2Associate Professor, Department of Orthopaedics, Government Thiruvarur Medical College, Thiruvarur, Tamil Nadu, INDIA. Email: bansarinas@yahoo.com
Abstract Background: Fracture Distal end of Radius is more common fracture that may lead onto malunion in many cases and stiffness of some cases. This causes a disability in society even in hospital managed cases. We made a study at our institution to correlate the management method and occurrence of Complex regional pain syndrome. Aim of Study: To correlate occurrence of Complex regional pain syndrome and 2 different reduction methods for fracture Distal end of radius Materials and Methods: 100 patients of fracture Distal end of Radius are reduced alternatively with Traction method and pressure method (50 cases each)and they were followed for CRPS Results: Totally 5 cases were gone for CRPS. In traction method the occurrence is more (n=4)compared to pressure method (n=1). Conclusion: Pre reduction edema should be taken into consideration before advocating traction method Keywords: Colles fracture, CRPS, Traction method, Nerve conduction test.
INTRODUCTION Early documentation of Complex Regional pain syndrome (CRPS) dates back from Ambrose Pare’s report describing persistent pain and contracture during 16th century. Silas Weir Mitchell, the father of American Neurology gave the first detailed description of CRPS in 1864. Complex Regional pain syndrome is a disabling condition commonly occurs after fractures, surgeries and in some cases spontaneously. Increased sensitivity to tactile stimuli, swelling, sudomotor abnormality, impairment of motor function are the usual components of CRPS. The correlation between the occurrences of CRPS in Fracture distal of radius (Colles Fracture) is well proven. In case of displaced Colles Fracture, the correlation between the amount of displacement and subsequent correction and increased chances of occurrence of CRPS also well studied. CRPS associated with Nerve injury is well explained by another author. Our study is aimed at correlating the CRPS and Nerve injury caused by traction for reducing the Colles fracture.
AIM OF STUDY Our aim of doing this study is to 1compare the occurrence of CRPS in two groups of displaced Colles Fracture, one by traction method and another by pressure method2 to look for Nerve conduction abnormality in NCS amongst the CRPS individuals. Colles Fracture and reduction methods: Colles Fracture is one of the common fractures of elderly. Explained by Sir Abraham Colles during 1814, it occurs in the corticocancellous junction of distal end of radius. It gives raise to typical dinner fork deformity. If the deformity remains uncorrected, the result will be constant wrist pain, tendon dysfunction and attrition. In routine Orthopaedic practice, the deformity needs to be corrected to prevent complications. Usually two methods are used to reduce Colles Fracture.
METHODOLOGY The study was done at outpatient department at Department of Orthopaedics, Government Thiruvarur Medical College Hospital, from July 2017 to April 2019. Totally hundred patients of displaced Colles fracture among female patients were studied. Following were used as Inclusion criteria
Exclusion criteria
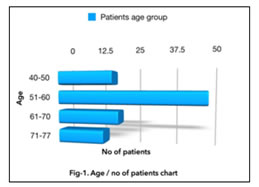
Figure 1: The age of patients ranged from 40-77. The average age being 54 All hundred patients received at Outpatient department, were taken X-rays of concerned wrist and then they were taken to minor procedure room. They were given hematoma block. Out of 100 patients, 50 patients were treated with traction-counter traction method. Other 50 patients were treated with pressure method to reduce the fracture. Alternative patients were taken into both methods. Amount of displacement was not taken into consideration for allotting specific method of reduction. Degree of displacement was averagely equal among both method study groups. After reducing the fracture, the styloid process of ulna and radius compared and Below elbow slab applied and arm sling pouch was given. X-rays of wrist AP and lateral were taken. All patients were treated as outpatients and were instructed to do regular finger mobilization exercises and to avoid prolonged dependent position to avoid edema. They were instructed to attend outpatient department every week till six weeks and once in fifteen days up to six months. During the first visit after fracture reduction, cast conversion was done for all patients after ruling out the edema. At the end of completion of six weeks Plaster was removed in all patients and Xray was taken to confirm the fracture union. In all cases fracture was uniting with good callus formation. Then patients were reviewed in every fifteen days. At the three months review, patients were checked for Complex regional pain syndrome symptoms. Again Xray was taken at three month visit to look for complete union in all patients and signs of Complex regional pain syndrome patients. They were followed up to six months. Again the remaining patients who are not enlisted in CRPS list checked for symptoms and signs of CRPS. For patients who are diagnosed of CRPS at three months, were done Nerve conduction study, to know about the reduction of amplitude and increase in reaction time. (Fig11). Analysis And Scoring: Clinical diagnosis of Complex regional pain syndrome is done with Budapest criterion (Ref. (Table -1)which is explained below
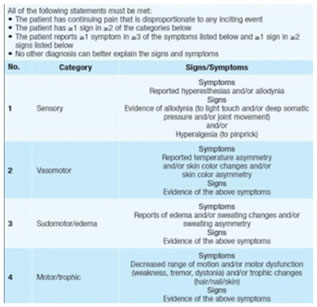
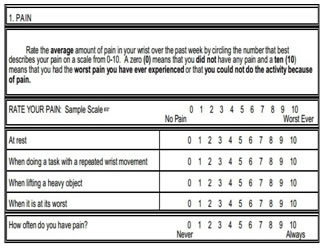
Table 1: Budapest criterion for CRPS Table 2 and 3: Patient-related Wrist evaluation score
The pain is regional (not in a specific nerve territory or dermatome) and usually has a distal predominance of abnormal sensory, motor, sudomotor, vasomotor, and/or trophic findings. The syndrome shows variable progression over time. To make the clinical diagnosis, the following criteria must be met: A. Continuing pain, which is disproportionate to any inciting event. B. Must report at least one symptom in all four of the following categories:
C. Must display at least one sign at time of evaluation in two or more of the following categories:
The above clinical criteria was imposed on our patients and the patients who met above criteria were marked as ‘Positive CRPS’ and who are negative were marked as ‘Negative CRPS’. All the 100 patients also evaluated for wrist and hand function with help of Patient Related Wrist Evaluation Score; A total score of evaluated for wrist and hand function with help of Patient Related Wrist Evaluation Score; A total score of 0- 100 was given to all patients and they are charted in Master chart. Radiological evaluation for all patients were done at 3rd and 6 the month ends in which a) Patchy osteopenia in periarticular region, b) sub periosteal bone resorption(Fig ) were used as points to mark ‘Radiologically positive’ in master chart. All the positive cases exhibited the radiological signs for CRPS only by end of six months. The only patients who were positive for Budapest, Patient related Wrist evaluation score and radiologically positive and labelled as Complex regional pain syndrome were included in Nerve conduction test by the end of six months. The prolongation of reaction time and decrease in amplitude of the wave are taken as criteria for Nerve injury associated with traction or pressure method.
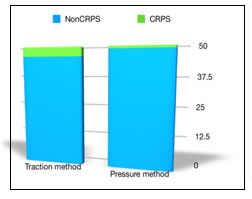
RESULTS Totally hundred patients were evaluated; Out of these hundred patients, Five patients developed Complex regional pain syndrome under Budapest criteria were marked as ‘Positive CRPS’. One patient in pressure Figure 2: distribution of CRPS patient amongst traction method and pressure method
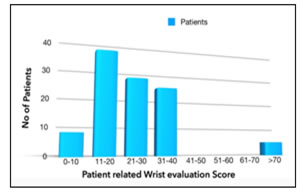
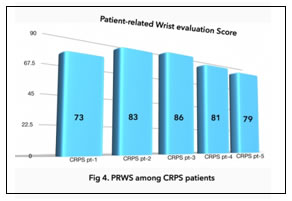
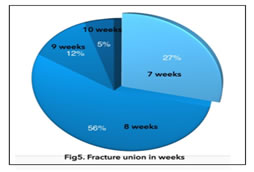
reduction method and four patients in traction method is affected by Complex regional pain syndrome.(Fig2 ) Distribution of scores(out of hundred) of Patient-related Wrist score is depicted in Fig.3 . All non CRPS patients had a score ranging from 8-37. All five Complex regional pain syndrome patients had score more Figure 3: distribution of patients in patient-related wrist evaluation score; Figure 4: PRWS among CRPS patients than70.(Fig 4).All non CRPS patients PRWE scores were less than 40. CRPS patients’ score were more than 70 (73,83,86,81 and 79 respectively. In nerve conduction tests, among 5 patients, CRPS patient in pressure method group had a normal nerve conduction test. All the four CRPS patients in traction reduction method group had abnormality in nerve conduction test, 3 patients in median Nerve and one patient in superficial Radial nerve. In all hundred cases fracture united well.The radiological union of fractures distal radius ranged between 7 weeks to 10 weeks. There was no correlation between occurrence of CRPS and Fracture union Figure 5: Table 4: Incidence of CRPS in various studies
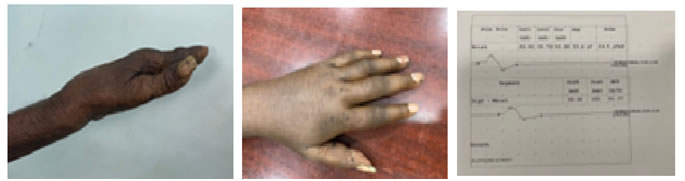
Figure 6: Clinical picture of CRPSPt-1; Figure 7: Xray of CRPS patient Figure 8: Dinner fork deformity; Figure 9: Clinical picture of CRPSpatient-3; Figure 10: Nerve conduction study of CRPS pt -5 DISCUSSION The incidence of CRPS in Fracture distal radius is ranging from 1% to 35%; Following table gives the comparison of incidence of CRPS in various prominent studies available in literature and our study. The incidence is comparable with other studies available in literature available. Comparing the two groups, traction reduction method group has more incidence of CRPS comparing the pressure reduction method group. The traction probably causes traction injury of nerves which is followed by CRPS on follow up. This is proved by the nerve conduction test results of traction reduction method group. CRPS associated with nerve injury is classified under CRPS -2 and CRPS in non injury type is classified under CRPS-1. The noxious stimulus caused by nerve injury becomes the cause for CRPS in traction reduction method group. Another restriction in our study is psychological scoring was not included in our study.
CONCLUSION Even though the traction reduction method is golden standard reduction technique for displaced distal radius fractures, the oedema prior to reduction, plays a major role. More the oedema, more will be the traction to bring back the normal anatomy and subsequently more chances for nerve damage and eventually Complex regional pain syndrome. So , when a case of fracture distal radius fracture comes to Outpatient department with increasing oedema, admission, limb elevation and anti oedema measures should be the priority than immediate reduction. This point is protocolled in our department after this study.
REFERENCES
|
|
 Home
Home