Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 1 - July 2019
Ganesh Madhavrao Nalge1, Jayant Jain2*, E D Pawar3, C R Thorat4
1Assistant Professor, 2Associate Professor, Department of Orthopaedics, Dhanalakshmi Srinivasan Medical College and Hospital, Perambalur -621113, Tamil Nadu, INDIA. 3Professor and Head, Department of Orthopaedics, G. G.M.C. Mumbai and J.J. Group of Hospital, Mumbai, Maharashtra, INDIA. 4Professor and Head, Department of Orthopaedics, Government Medical College, Aurangabad, Maharashtra, INDIA. Email: drjayanthj@rediffmail.com
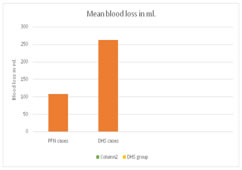
Abstract Background: Fracture of intertrochanteric femur has been recognised as a major challenge by the Orthopaedic community, not solely for achieving fracture union, but for restoration of optimal function in shortest possible time with minimal complications. Operative treatment in the form of internal fixation permits early rehabilitation and offers the best chance of functional recovery hence becomes the treatment of choice for virtually all fractures of trochanteric region. Among the various types of implant available i.e. fixed nail plate device, sliding screw plate and intramedullary devices, the compression hip screw is most commonly used but recent technique of closed intramedullary nailing is gaining popularity. The present study is to compare the results of Proximal femoral nailing (PFN) and Dynamic hip screw (DHS) in terms of effectiveness, strength of construct, early mobilisation of patients and their advantages / disadvantages when used to treat similar type of fractures. Material and methods: This prospective study was done at Government Medical college, Aurangabad between 2013-2016 under the guidance of its ethical committee. This study was conducted on 60 patients (30 patients were in PFN group and 30 patients were in DHS group). Clinical and radiological follow up of all patients were carried out regularly till the patients achieved maximum possible functions of injured limb. Results were evaluated using Harris hip scoring system. Results: Mean blood loss was 107ml. for PFN and 262ml. for DHS. Average surgical time was 79 minutes for PFN and 103 minutes for DHS. Average time of union was 12 weeks for PFN and 14.85 weeks in DHS. Conclusion: PFN has lesser operative time, lesser blood loss, early post-operative rehabilitation and better functional outcome especially in unstable fractures compared to DHS. Key Word: Proximal femoral nail, Dynamic hip screw, Intertrochanteric femoral fractures.
INTRODUCTION Intertrochanteric fractures are extra-capsular fractures extending from base of greater trochanter along intertrochanteric line to lesser trochanter just above medullary canal. Intertrochanteric fractures of femur are most commonly operated fractures. Intertrochanteric fractures are common in elderly people. The frequency of these fractures has increased primarily due to increased life span along with sedentary life due to urbanization. Trochanteric fractures when occur in younger population is due to high velocity trauma, whereas in elderly population it is mostly due to trivial trauma. Also, the geriatric age group (higher proportion in women) has a higher incidence of osteoporosis along with low energy falls from standing height accounts for approximately 90% of hip fractures in community. Higher velocity traumatic intertrochanteric fractures are relatively rare and are more common in men less than 40 years of age.1 Intertrochanteric fractures can be managed by conservative or operative methods. Conservative methods were the treatment of choice until 1960 when Horowitz2 documented that the mortality rates in conservative methods were higher as compared to operative methods. The trochanteric fractures managed by conservative methods usually unite. If suitable precautions are not taken than fracture undergoes malunion, leading to varus and external rotation deformity at the fracture site and shortening and limitation of hip movement.2 As conservative methods resulted in higher mortality rates and complications like decubitus ulcer, urinary tract infections, pneumonia, thromboembolic complications, these methods have been abandoned. Conservative methods are now indicated only under 2 conditions,
Since this fracture is more common in the elderly patients, the aim of treatment should be prevention of malunion, and early mobilization. Taking all the factors into consideration, surgery by internal fixation of the fracture is an ideal choice.3 Factors determining the strength of fracture implant assembly depends on the bone quality, fragment geometry, fracture reduction, implant type and implant placement.4 Surgeon can control only the quality of reduction, choice of implant and its placement. As intertrochanteric fractures have the highest post-operative fatality rate among surgically treated fractures, they have become an important health issue and is very important to study and compare different surgical options available for these fractures. Implants for the fixation of intertrochanteric fractures can broadly be divided into
The most commonly used device is the Dynamic Hip Screw with Side Plate (D.H.S). This is a collapsible fixation device, which permits the proximal fragment to collapse or settle on the fixation device, seeking its own position of stability. The latest implant for management of intertrochanteric fracture is P.F.N (Proximal Femoral Nail). This implant is a cephalo-medullary device and has many potential advantages like5
In view of these conditions, this study is taken up to compare the results of D.H.S and P.F.N. MATERIAL AND METHODS This was a prospective, analytical study aimed to achieve fracture union by using two different kind of internal fixation modalities in similar type of fractures. Inclusion criteria: includes recent traumatic history, isolated intertrochanteric fractures, stable and unstable fractures and the consent to participate in study. Exclusion criteria: includes patients with multiple fractures, pathological fractures, old neglected fractures, paediatric age group, reverse intertrochanteric fractures and elderly patients with high medical risk for anaesthesia and surgery. IMPLANT DETAILS: Dynamic hip screw Components: The implant consists of a lag screw, a compression screw and a barrel side plate attached to it. Lag Screw is available in lengths from 60-110mm.Compression Screw of 36 mm is used which allows compression at the fracture site. Barrel side plate are available in angles of 1250,1300, 1350, 1400and from 4-12 holes. 1350 and 1400 plates are more often used. 4.5 mm cortical screws are used to fix the side plate with shaft. In our study we used lag screw of 60-110 mm and a side plate that allowed a purchase of at least 8 cortices with shaft of femur and 130-140⁰ angled plate depending upon the neck shaft angle determined pre-operatively. Figure 1: 1 - Compression screw 2 - Richard’s screw 3 - Barrel plate
Figure 2: 1 - T Handle 2 - Angle guide 3 - Tap 4 - Guide wire
Figure 3: 1 - Screw driver for Richard’s screw 2 - Triple reamer
PROXIMAL FEMORAL NAIL Components: The implant consists of a Proximal Femoral Nail, a self-tapping de-rotation 6.5mm screw, a self-tapping 8mm femoral neck lag screw, 4.9mm distal locking screws and an end cap. PFN is made up of either 316L stainless steel or titanium alloy. PFN comes in following sizes: Length of standard PFN is 250 mm and available length of Long PFN is 340, 360, 380, 400 and 420 mm. Diameter: 9, 10, 11, 12 mm Neck shaft angle range: 1300, 1350 The nail is having 14 mm proximal diameter. This increases the stability of the implant. There is 6⁰ medio-lateral valgus angle which prevents varus collapse of fracture, even when there is medial communition. The distal diameter is tapered to 9-12 mm, which also has a groove to prevent stress concentration at the end of the nail and avoids fracture of the shaft distal to the nail. Proximally it has two holes, the distal one for insertion of 8mm neck screw which acts as a sliding screw and the proximal one is for 6.5mm hip screw which helps to prevent the rotation. Distally the nail has two holes for insertion of 4.9mm locking screws of which one is static and the other one is dynamic hole which allows dynamization. In our study we used the standard length PFN of 250mm with distal diameter of 9, 10 and 11mm. The common neck shaft angle used was 135⁰ followed by 130⁰. End cap was not used. Figure 4: 1 - Cannulated awl 2 - Proximal reamer 3 - T-handle
Figure 5: 1 - Proximal femoral nail with 14mm diameter with 6⁰medio-lateral valgus and tapered tip. 2 - 6.5mm de-rotation screw. 3 - 8mm lag screw. 4 - 4.9mm locking bolt in static mode 5 - 4.9mm locking both in dynamic mode Figure 6: 1. Hammer assembly 2. Zig
Figure 7: 1 - Solapur protection sleeve 2 and 3 - Sleeve for guide wire and reamer for proximal screw 4 - Reamer for 6.5 mm de-rotation screw 5 - Reamer for 8mm lag screw Pre-operative routine investigations were done. Informed consent was obtained by patient for both surgical procedure and participation in the study. After anaesthetic fitness all cases were operated under combined spinal and epidural anaesthesia on fracture table using standard protocol. Post-operative antero-posterior and lateral view x-rays of the operated hip were taken. Post-operatively static exercise in bed for glutei, hamstrings, quadriceps and breathing exercises were started next day of surgery. Sitting was allowed on next day of surgery with passive exercises in bed. Drain if inserted was removed after 48 hours. ROM exercises were started actively. The protocol for weight bearing, in stable fractures is to start partial weight bearing next day after surgery and full weight bearing was started after 6 weeks, while in unstable fractures, non-weight bearing walking was allowed on operated side with the help of a walker or crutches next day after surgery, partial weight bearing after 6 weeks and full weight bearing was started after 3 months approximately. However, weight bearing was modified as per the type of fracture, stability of internal fixation, fracture union and tolerance of the patient. Post-operative dressings were done on 2nd and 5th day. Suture removal was done on or after 14 days. Follow up was done at 2nd, 4th, 6th week, 3 months, 6 months, and 1 year after the surgery. The patients were assessed functionally on the basis of Harris Hip Score and radiologically. The post-operative pain was assessed as per Hip Score criteria at the end of 1 year along with post-operative gait assessment. Union was decided on the basis of obliteration of fracture line with bridging callus so as to allow unprotected function of the limb. Harris Hip Scoring System: Formulated by W. H. Harris6 it incorporates all-important variables into single reliable figure, which is both reproducible and reasonably objective.
Table 1: Point scale with maximum of 100 points:
Table 2: Harris hip score
Table 3: The score is reported as 6
RESULTS This study was conducted on 60 patients (30 patients were in PFN group and 30 patients were in DHS group). Male: Female ratio was 2.75:1 in PFN group and 9:1 in DHS group.
Table 1: Distribution of cases according to gender among both groups
Table 2: Distribution of cases according to age group
In PFN group 15 cases (50%) were having Right side involvement and remaining 15 cases (50%) were having Left side involvement whereas in DHS group 16 cases (53.33%) were having right side involvement and remaining 14 cases (46.67%) were having Left side involvement with p-value =0.796 (NS). Table 3: demonstrates distribution of cases according to fracture
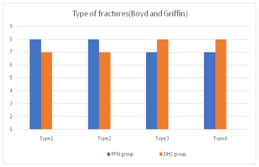
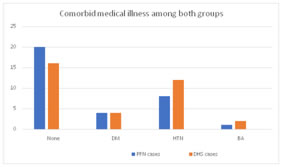
Figure 8 Figure 9 Figure 8: Distribution according to type of fractures (Boyd and Griffin classification) among both groups Figure 9: Co-morbid medical illness in both groups Table 4: Average surgical operative time
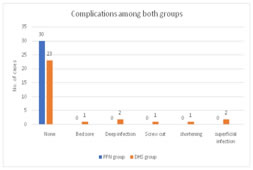
Figure 10: Average blood loss among both groups Figure 11: Shows complications among both groups
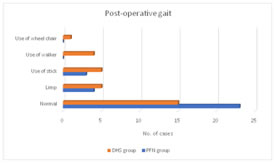
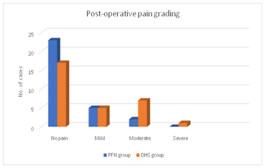
Figure 12: Shows post-operative gait among both groups Figure 13: Shows post-operative pain among both groups
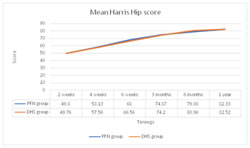
Table 5: Comparison of Mean Harris Hip score
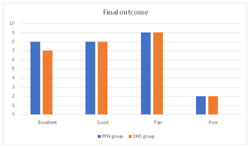
Figure 14: Mean Harris hip score among both groups Figure 15: Shows final outcome among both groups Table 6: Association between final outcome and fracture outcome
Table 8: Comparison of Mean Harris Hip score in stable and unstable cases after 1 year
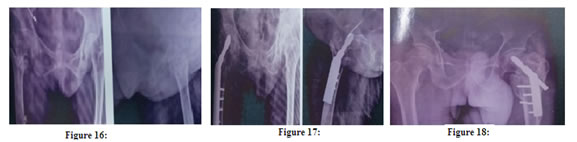
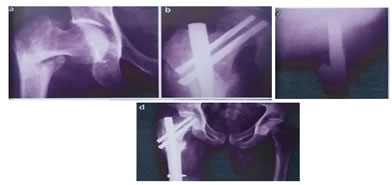
Figure 16: Pre-operative AP and Lateral radiographs; Figure 17: Post-operative AP and Lateral radiographs; Figure 18: Complication of excessive collapse of DHS screw leading to shortening of 3cms A 41 - year old female with right sided stable intertrochanteric fracture treated with PFN. (Fig. 19)
DISCUSSION With all the advancement in the field of technology, the road traffic accidents are increasing day by day. With modern methods of treatment along with awareness of healthy living, average life expectancy of Indian population has almost doubled from 35 years to 64 years resulting in tremendous increase in osteoporotic population and osteoporotic fractures. Increasing life expectancy, sedentary and busy life style along with increasing traffic on road and lack of observing traffic rules result in increased incidence of fractures. Trochanteric fractures are most frequently encountered fractures by orthopedic surgeons worldwide. Before the invention of operative treatment, conservative treatment in the form of prolonged traction was preferred, however this treatment was associated with complications like bed sores, deep vein thrombosis, bronchopneumonia. Elderly people could not tolerate prolonged immobilization. This led to evolution of operative treatment. Operative treatment permits fixation of fracture, not only anatomical or in near anatomical position but also allowed rapid mobilization. Since 20th century numerous operative treatment modalities have been evolved like smith Peterson nail (S P Nail), Jewett nail, Enders nail, Asnis screw, Medoffs plate etc. amongst them Dynamic hip screw (DHS) is most frequently used device. Proximal femoral nail has been recently introduced in 1996 by AO/ASIF, has begun to compete with Dynamic hip screw in treatment of proximal femoral fractures. This intramedullary device has following advantages
Sixty patients of trochanteric fractures managed operatively by internal fixation with Dynamic Hip Screw and Proximal Femoral Nail during the course of this study were sorted and each was followed for at least 1 year. Follow up of all patients in both groups were carried out regularly with clinical and radiological assessment at successive visits till patients achieved maximum possible functions of the injured limb. The data collected from patients of these two groups was analysed, evaluated and compared with each other. Age distribution Most of patients in present study were from age group of 6th to 8th decade. Mean age in years for group operated by PFN is 52.70. Mean age in years for group operated by DHS is 55.17. This signifies the fact that patients from these age groups are involved in low energy trauma like domestic fall (fall at home)4,7,8,9,10 Gallaghar et al11 (1980) reported an eight-fold increase in trochanteric fractures in men over 80 years and women over 50 years of age.Average age reported by other workers is as follows
Cleveland et al12 pointed out the inherent weakness of the bone structure of elderly, predisposing them to injury. More wide spread measures to correct or prevent osteoporosis should be instituted. The elderly should be freed from potential danger of poor lighting, slippery floor, wet slippers etc. For some patients whose general condition makes them vulnerable to fall and fracture, total restriction of independent ambulation is indicated. Due to early fixation of such fractures and early mobilization, these patients could gain full range of movement at an early date with minimal loss of productivity.Sex distribution: Most of patients from present study were males. There was a male preponderance in our patients. The ratio of males to female was 2.75:1 in PFN group and 9:1 in DHS. This reflects the preference and better acceptance of surgery by males and higher incidence of trochanteric fractures of femur in male population due to their more active lifestyles. David G. Lovelle14 found trochanteric fractures more common in women than men by a margin of three to one. Melton J.L., Ilistrup DM, Riggs BL et al11 (1982) released a study titled 'fifty years trend in Hip fracture incidence' and reported a female to male ratio of 1.8:1. This variation is probably because our study measured the male female ratio amongst operated fractures that reported for follow up and not the actual sex incidence for all trochanteric fractures. Majority of patients in this series were male as they are more outgoing and engaged in activities like agriculture, driving of motor vehicles and are more likely to be involved or prone to accidents/ fall. Females play a more dormant role and are involved more in household activities. B. B. Ohari and Hatim Shaikh from Indore (1957) also found males predominantly affected in their series. Ratio of males: females in other series is given below
Type of fractures: In our present study, out of 60 intertrochanteric fractures, 30 cases were of unstable fracture pattern and 30 cases were of stable fracture pattern. Out of which 16 (54.33%) of stable and 14 (46.67%) of unstable fracture pattern are treated by PFN. 14 (46.67%) of stable and 16 (54.33%) of unstable fracture pattern are treated by DHS. According to Mervyn Evans4 the Intertrochanteric fractures are considered as stable or unstable depending upon integrity of posteromedial cortex. Fractures with intact posteromedial cortex are considered as stable fractures while fractures with loss of posteromedial cortex are considered as unstable fractures. Postero medial cortex constitutes mainly the lesser trochanter.16,17,18,19Wound complications: Superficial wound infection was seen in 2 cases operated by DHS whereas no cases operated by PFN were having it. These 2 cases had superficial wound infection at suture site. This may be attributed to low immunity status of patient as the patient was of asthenic built and belonging to low socioeconomic status with soft tissue exposure, which is more in cases operated by DHS. In all these patients, treatment of IV Antibiotics was prolonged, as per our protocol we gave IV antibiotics for 5 days but in presence of wound infection we continued its use for 10 days. Dressing of wounds were done as per necessity. In all these cases, the wound healed in the end. In the series of patients operated by DHS by Dr. G.S Kulkarni20, there were two cases of deep infections which were treated by removal of implant. The infected sinuses thus healed after implant removal. Average time of Fracture Union: Average time of union was about 12 weeks in PFN and 14.85 weeks in DHS. We have used criteria for union as presence of bridging callus at fracture site. Clinically, absence of pain at fracture site.
Radiological time of union in other series
Range of Movement (As per Harris Hip Scoring system): The range of movement calculated by the Harris Hip Scoring system treated by both the implants i.e. PFN and DHS was good and almost same. The range of movements namely flexion, extension, external and internal rotation was good in most cases, excellent in a few. In very few cases, there were poor results. The poor result was attributed to other associated factors namely a long interval between trauma and surgery and development of post-operative infection.
Technical and Mechanical complications of PFN published in the literature
In present study, Boyd and Griffin type I, II, III fractures were there. This classification is easy to understand, recollect and apply. We found no cases with screw cut out, fracture below the tip of nail and Z effect. There were 2 cases of reverse Z effect and 1 case of breakage of nail in between proximal screw and distal lock.
CONCLUSION PFN has following advantages over DHS in treatment of intertrochanteric fractures
However, the difference in functional outcome is not statistically significant and thus requires a larger group of study to prove significance.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home