Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 2 - August 2019
Ashish Dahiya1, Atul Singh2, Gaurav Akhand3, Navneet Goel4, Ashish Goel5, Gurwindar Singh6
1Senior Resident, 2,3Third Year DNB Resident, 4HOD & Specialist, 5Unit Head & Specialist, 6Assistant Professor, Department of Orthopedics, Dr. Baba Saheb Ambedkar Medical College and Hospital, Rohini, New Delhi, INDIA. Email: dahiyar.k.jh@gmail.com
Abstract The present study consisted of 75 cases of age group 18 years or above of either sex, with closed diaphyseal fracture of humerus, admitted in the Orthopaedics department of Dr. B.S.A. Hospital, Rohini, New Delhi. All of these patients were operated upon by open reduction and internal fixation using a locking compression plate. Conservative methods have inherent limitation that it can lead to malunion, joint stiffness and of limited value in poly-trauma patients. Open reduction and internal fixation of fractures with locking plates attains anatomical reduction, enhanced union rate, low complication rate, and a rapid return to function. In our study excellent results were obtained in 76 % of the cases and good in 24 % patients. Key Word: Diaphyseal, Humerus, Locking, Plate, Osteosynthesis, Fractures.
INTRODUCTION Diaphyseal fracture of humerus is easily amenable to conservative methods as the humeral shaft is well enveloped in muscle with excellent blood supply and can be easily splinted1. Moreover it is a non-weight bearing bone with some acceptability for shortening and angulatory, axial or rotational deformity due to mal-union. Conservative methods have inherent limitation in poly-trauma patients. Besides many other complications are associated with conservative methods like:
Open reduction and internal fixation of fractures with metal plates attains anatomical reduction, enhanced union rate, low complication rate, and a rapid return to function. The exploration and treatment of associated neurovascular injuries is possible and the fixation is stable enough to allow early usage of upper extremity in the multiply injured patients. Thus, Plate Osteosynthesis is the gold standard for operative treatment of diaphyseal fractures of humerus2, 3. Locking Compression Plates (LCP) represent the newest advance in plate technology. Locking Compression Plates are fracture fixation devices which are basically a modification of Dynamic Compression Plates, wherein they have threaded screw holes. These threaded holes allow screws to thread to the plate and the implant then functions as a fixed angled device4. These plates may also have a mixture of holes that allow placement of both locking and non-locking screws. The screws that are inserted into these combination holes (combi-plate) can act in a conventional compression fashion or in locking mode.5
MATERIAL AND METHODS The present study consisted of 75 cases of age group 18 years or above of either sex, with diaphyseal fracture of humerus, admitted in the Orthopaedics department of Dr. B.S.A. Hospital, Rohini, New Delhi. Exclusion criteria:
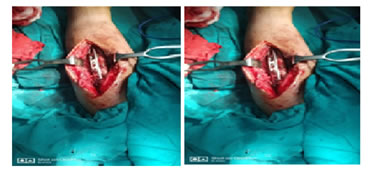
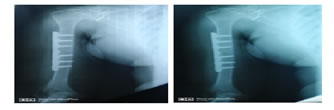
As per individual patient’s pre-anaesthetic evaluation and associated medical condition, brachial block or general anaesthesia was given. After proper painting and draping, the fracture site was exposed; using the anterio-lateral or posterior approach depending upon the type and pattern of fracture, the fracture was reduced and fixed by means of locking compression plate. Wound was closed in layers, leaving a negative suction drain in place. Intravenous antibiotics, analgesics, calcium carbonate and ascorbic acid were given post-operatively. Check radiographs were taken and passive physiotherapy was started at the earliest possible. Sutures were removed on the fourteenth day. All patients were subsequently assessed, after every 3-4 weeks in OPD, clinically as well as radiologically, for evidence of union and complications if any and the obtained data recorded and tabulated. The patients in study were evaluated clinically, radiologically and functionally for fracture union time, complications and functional outcomes. The Stewart and Hundley criteria were used to assess functional outcome6. Stewart And Hundley Criteria
RESULTS AND CONCLUSION The following inferences were drawn:
To conclude, Locking compression plate is a useful implant with good results in the treatment of diaphyseal fractures of humerus, especially when fracture is comminuted, in osteoporotic and in peri-implant fractures.
DISCUSSION In the present study the age incidence ranged between 19-70 years with an average age of 42.64 years. McCormack et al7 reported 44.25 years as an average age while Kumar et al8 observed average age of 36.6 years in their study which is comparable to the findings of our study. In our study diaphyseal fracture of humerus was most frequently seen in the 4th and 5th decade of life. 63 patients (84%) were less than 50 years of age which can be explained on the basis of maximum outdoor activity being undertaken by this age group. Amongst the 75 patients included in our study, 24 patients (32%) had associated injuries. Radial nerve palsy was present in 15 patients (20%). Amongst these 15 patients having radial nerve palsy there were 8 poly-trauma patients. Sharma et al10 in their study reported associated injuries in 21% patients with 10% patients having associated radial nerve palsy. Radial nerve exploration was done in 15 cases followed by cock-up splint application. Radial nerve recovered in all 15 cases with an average time interval of around 6 weeks. Bell et al9 reported recovery in 7 out of 8 cases of radial nerve palsy in their study and Sharma et al10 reported recovery in 9 out of 10 cases of radial nerve palsy in 3-12 weeks in their study. This may be explained by the fact that in all 15 cases of radial nerve palsy in our study, on exploration, the nerve was found to be macroscopically intact indicating neuropraxia or axonotemesis as the underlying pathology. Moreover radial nerve being a predominantly motor nerve carries excellent prognosis in case of any injury in continuity. Complete fracture union (consolidation) is defined as complete healing with ossified callus with near obliteration of fracture line. In our study of 75 patients, 51 patients (68%) had union within 16 weeks, 21 patients (28%) between 17-20 weeks and 3 patients (4%) between 21-24 weeks. The average time for union was 16.1 weeks. No patients had non-union. Kumar et al7 by using internal fixation and plate osteosynthesis obtained union in an average of 12.4 weeks. Singh et al12 in their study observed fracture union in 17.2 weeks with a range of 10-48 weeks using locking compression plate while Bell et al9obtained union in their study in an average of 19 weeks. As regarding the range of motion at the elbow joint, we observed in our study that 57 patients (76%) had full movement at elbow while 18 patients (19%) had slight limitation of movements of elbow. As for the shoulder too, 57 patients (76%) had full range of movement in flexion at the shoulder while 18 patients (24%) had deficient movement at the shoulder. Bell et al9 in their study observed normal shoulder function in 76.5% patients. Abaloet al11 reported normal shoulder function in 89% and normal elbow function in 65% patients. Celebiet al13 in their study documented normal elbow function in 91% patients. In our study, 6 patients (8%) had superficial infection which responded to antibiotics alone while 3 patients (4%) developed iatrogenic radial nerve palsy. Bell et al9 reported iatrogenic radial nerve injury in 1 case among the 34 cases operated in their study. Sharma et al10 reported incidence of same in 1 case amongst the 44 cases undergoing plating. Singh et al12 in their study observed iatrogenic radial nerve palsy in 3.63% patients undergoing surgery for diaphyseal fracture of humerus using locking compression plate. The incidence of iatrogenic radial nerve palsy was 4.24% in a study by Wang et al14 As regarding the functional results, by applying the Stewart and Hundley criteria we obtained excellent results in 56 patients (76%) and good results in 18 (24%) patients. Abalo et al11reported excellent results in 52.2% patients and good results in 30.4% patients applying the Stewart and Hundley criteria. Celebi et al13 too, applying the same criteria, obtained excellent results in 83.3% patients and good results in the remaining 16.7% patients in their study. In our study, we did not have any case of implant failure in the form of plate loosening or breakage or bending or any screw loosening or breakage or bending, which can be attributed to the inherent strength of the locking screw and plate. We did not encounter any case of peri-implant fracture or osteolysis which can be ascribed to principle of internal splintage working in locking compression plate vis-a-vis rigid stable fixation in dynamic compression plate. There was no case of delayed union, mal-union or non-union which can be attributed to meticulous surgical technique and implant design. Thus, the highlights of the present study are consolidated union in all 75 patients with an average time of 16.1 weeks, no case of implant reaction, no implant failure in the form of implant loosening, implant breakage or screw pull-out, minimal superficial infection with excellent overall results. Age Incidence: The youngest patient encountered in our study was 19 years old and the oldest was 70 years of age as shown in table 1. Table 1: Age Incidence
Time For Complete Union (Consolidation): Complete fracture union (consolidation) is defined as complete healing with ossified callus with near obliteration of fracture line. As shown in table 2, out of 75 patients, 51 patients (68%) had consolidation within 16 weeks, 21 patients (28%) between 17-20 weeks, and 3 patient (4%) between 21-24 weeks. The average radiological complete union time was 16.1 weeks. No patient had implant failure or non-union.
Table 2: Time For Complete Union (Consolidation)
COMPLICATIONS: In our study, 6 patients (8%) had superficial infection and 3 patient (4%) developed iatrogenic radial nerve palsy as shown in table 14. The superficial infections responded to antibiotics alone while the iatrogenic radial nerve palsy recovered spontaneously between 11-12 weeks.
Table 3: Complications
RESULTS By applying the Stewart and Hundley criteria the following results were obtained we obtained excellent results in 57 patients (76%) and good results in 18 patients (24%). Table 4: Results (Using Stewart And Hundley Criteria)
PRE-OP
INTRA-OP POST-OP
REFERENCES
|
|
 Home
Home