Official Journals By StatPerson Publication
|
Table of Content - Volume 13 Issue 3 - March 2020
Principle of ligamentotaxis in management of fractures of metacarpals and phalanges of the hand - A review of techniques
Shyam Prasad Parimala1, Avinash Reddy Pashap2*
1,2Assistant Professor, Department of Orthopaedics, Rajiv Gandhi Institute of Medical Sciences, Adilabad, Telangana, INDIA. Email: drshyam09@gmail.com
Abstract Background: Fractures of metacarpals and phalanges are the most common among upper limb bony injuries. It is important to consider soft tissue healing along with fracture healing in a hand, because successful outcomes require the return of functional integrity to both the tissues. Ligamentotaxis using closed reduction manoeuvres are gaining familiarity in treating comminuted fractures and intra articular or juxta articular fractures of the hand. A total of 24 fractures of metacarpals and phalanges of hand were treated surgically with principle of closed reduction with ligamentotaxis and internal fixation using k-wires or ligamentotaxis with external fixation using mini-external fixator or ligamentotaxis with double parabolic k-wire application as dynamic distraction. 10 patients had associated soft tissue injury of the hand. The patients were followed up to a period of 6 months (range: 5-14 months) on monthly basis and were evaluated with x rays and range of movements and ability to hold objects. Among 3 patients treated with dynamic double parabolic k wire fixation, 2 cases (66.6%) had good results and 1 case had poor result (33.3%). In 3 cases of 1st carpo meta carpal joint injuries who were treated with closed reduction and ligamentotaxis with k-wire application plus cross pinning stabilisation method, functional outcome was excellent in 1 case (20%) and good in 4 of them (80%). Of the 16 cases with mini external fixation 5 cases (33%) had excellent result, 7 (42%) had good, 3 (18%) had fair and 1 (16,25%) had poor results. These minimally invasive procedures respect the soft tissues and prevent damage to complex intrinsic anatomical structures thereby preventing open reduction to achieve alignment. Moreover external hardware application enhanced the ease of regular antiseptic dressings, thereby promoting faster wound healing in cases of associated soft tissue injuries of the hand. Key Word: fractures, metacarpals, phalanges Fractures of metacarpals and phalanges are the most common among upper limb bony injuries and contribute to about 10% of total fractures among them1. It is important to consider soft tissue healing along with fracture healing in a hand, because successful outcomes require the return of functional integrity to both the tissues2. It is well recognized that soft tissue scarring affects hand function more than fracture healing, and joint stiffness is the most frequent complication of fractures3. Successful rehabilitation of hand fractures addresses the need to (a) maintain fracture stability for bone healing, (b) introduce soft tissue mobilization for soft tissue integrity, and (c) remodel any restrictive scar from injury or surgery4. The challenges in treating metacarpal and phalangeal injuries of hand is to design intervention protocols that recognize the need to maintain fracture stability for maximal bone healing, while also introducing early, controlled-motion protocols to preserve soft tissue integrity and facilitate scar remodelling. Ligamentotaxis involves moulding fracture fragments into alignment by applying tension across the fracture using surrounding intact soft tissues5. The pull and the counter pull restore the length and guides alignment of the fracture fragments, which are otherwise difficult to control. This tissue tension can be maintained by external fixator or by a distractor5,6. Ligamentotaxis using closed reduction manoeuvres with external or internal fixators are gaining familiarity in treating comminuted fractures and intra articular or juxta articular fractures of hand8,9,10. Ligamentotaxis in management of metacarpal and phalangeal fractures of hand can be achieved externally by a mini external fixator frame acting as a distractor9, and internally by dynamic application of k-wires7,8,9.
METHODOLOGY A total of 24 fractures of metacarpals and phalanges of the hand were treated surgically with principle of closed reduction with ligamentotaxis and internal fixation using k-wires or ligamentotaxis with external fixation using mini-external fixator or ligamentotaxis with double parabolic k-wire application as dynamic distraction. The average age was 27 years (range, 19–42 y). Out of 24, 13 were metacarpal injuries that were fixed with mini external fixator frame and the rest 11 were phalangeal injuries. 10 patients had associated soft tissue injury of the hand. Indications for surgery included failure to achieve closed reduction, comminuted shaft fractures with displacement, rotational deformity, intra articular and juxta articular involvement of fractures. The average time from the injury to the surgery was 6 days (range, 1–14 d). The patients were started with active range of movements from the next day of surgery and after implant removal they were subjected to vigorous hand rehabilitation exercises. The patients were followed up to a period of 6 months (range: 5-14 months) on monthly basis and were evaluated with x rays and range of movements and ability to hold objects.  Figure 1: Figure 1A: Applying k-wire K1 across the head of the proximal phalanx and K2 over the head of the middle phalanx; Figure 1B: Bending K1 perpendicularly 1cm away fromphalanx; Figure 1C: Hair pin bending dorsally of K1 5-8m away from K2; Figure 1D: Achieving ligamentotaxis and engaging K2 in hair pin bend of K1 with longitudinal traction applied to distal phalanx
1. Surgical Technique: Ligamentotaxis using double parabolic K-wires in Intra / Juxta articular fractures of proximal interphalangeal joints of the hand.( Fig 1)8 A K-wire (K1) is placed transversely through the centre of the head of the proximal phalanx under fluoroscopic guidance. A second K-wire (K2) is then driven through the head of the middle phalanx (Fig 1a). The first wire (K1) is left long enough on both sides so the ends can be bent 90° distally to lie parallel and 1 cm away from the middle phalanx (Fig 1b). A Hair pin bend is made dorsally on the K1 wire approximately 5-8mm distal to K2 wire (Fig 1c). Traction is then applied on the middle phalanx so that K2 wire is engaged in the hair pin bend of K1 wire of the proximal phalanx, achieving the ligamentotaxis (Fig 1d). As a further stability ends of K2 wires are also bent to maintain the engaged initial pin. Intraoperative C-arm images are obtained at this point to evaluate the distraction at the joint space and to confirm that the articular surface of the base of the middle phalanx is not in contact with the condyles of the proximal phalanx. Passive range of PIP joint flexion-extension are checked. Active range of motion at proximal interphalangeal joints are started from the next post operative day. This fixation provides active longitudinal traction while preserving the joint space and allowing PIP joint motion. The fixator is removed after 4 weeks. 2. Surgical Technique: Ligamentotaxis using k-wires in fixation of base of metacarpal fracture-dislocations.(Fig 2)9
Figure 2: Figure 2A: Transfixation of K-wire to the 2nd metacarpal after applying longitudinal traction and achieving reduction of fracture at the base of the 1st metacarpal. Figure 2B: Stabilising the fixation by transfixing the base of the 1st metacarpal to the trapezium.
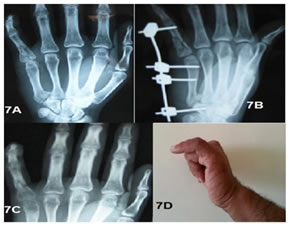
3. Surgical Technique: Ligamentotaxis using mini external fixator in metacarpal and phalangeal fractures. (Fig 3)10 Figure 3: Applyimg threated k wires and connecting to a rod after application of traction and achieving reduction. RESULTS 3 patients with articular and comminuted juxta articluar involvement of the proximal interphalangeal joint were treated with dynamic double parabolic k wire fixation. The average range of motion of the PIP joint at the final follow-up evaluation was 35° to 89° with 2 cases (66.6%) having good results and 1 case had poor result (33.3%). (Fig 4) 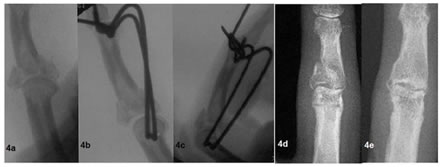 Figure 4: Figure 4A: Complex intra-articular pattern treated with dynamic double parabolic k-wires; Figure 4B: Lateral view showing reduction after ligamentotaxis; Figure 4C: Joint space and fracture alignment is maintained even on flexion of PIP joint; Figure 4D: 5 weeks after removal of the hardware. Figure 4E: 6 months postoperative film shows healing. 3 cases of Bennett fracture- dislocations and 2 cases of the 1st carpo meta carpal joint dislocation were treated with closed reduction and ligamentotaxis with k-wire application plus cross pinning stabilisation method. Functional outcome was excellent in 1 case (20%) and rest 4 cases had good outcome (80%).( Fig 5) Figure 5: Figure 5A: Bennett's fracture dislocation; Figure 5B: Treated with ligamentotaxis with k-wires; Figure 5C: Functional outcome of the thumb with healed pin tracts. Figure 6: Figure 6A: Preop Xrays; Figure 6B: Fracture fixation; Figure 6C: Xray on implant removal after 4 weeks; Figure 6D: Good range of movement 16 cases were fixed with mini external fixation in which functional outcome was excellent in 5 cases (33%) (Fig 6), good in 7 (42%), fair in 3 (18%) and poor in 1 (16,25%). The mean fracture healing was 3.04 weeks and mean soft tissue healing in cases of compound injuries was 15.06 days. Variation in fracture healing, functional outcome was independent of method of application of ligamentotaxis. Gross stiffness of the joint in the cases where mini external fixator was spanned across the joint was probably due to limitation of movements during fracture healing.(Fig 7) Complications included pin loosening in 3 cases of mini external fixation which required re fixation and pin tract infection in 1 case, and poor patient compliance of maintaining mini external fixation in 1 case. There were no complications in k-wire group while 1 patient in dynamic double parabolic distractor group had failure of hardware (k1 wire) which had to be reapplied.
DISCUSSION AND CONCLUSIONS Any attempt to regain good joint function necessitates anatomical reduction of the articular fragments and restoration of joint congruity and a stable functional arc of motion while the fixation device is providing stability for early mobilization11. Application of principle of Ligamentotaxis in injuries of hand fulfils the above mentioned criteria of fixation promoting function12,13,14. These minimally invasive procedures respect the soft tissues and prevent damage to complex intrinsic anatomical structures thereby preventing open reduction to achieve alignment15,16,17.
Figure 7: Figure 7A: Preop Xray; Figure 7B: Fixator across MCP joint; Figure 7C: Xray after implant removal; Figure 7D: Restricted flexon of the MCP joint Treatment by mini external fixation had better results in metacarpal fractures than phalangeal fractures in terms of functional outcome as they provide good basis for bone healing but not in terms of good range of motion. Whereas ligamentotaxis with k-wires used in treating juxta and intra articular phalangeal fractures promoted functional viability during fracture union. Moreover external hardware application enhanced the ease of regular antiseptic dressings, thereby promoting faster wound healing in cases of associated soft tissue injuries of the hand. REFERENCES
Policy for Articles with Open Access: |
|
 Home
Home