A comparative study of plate osteosynthesis over external fixators in proximal tibial fractures
Ruka Balaji obula Reddy1, Sardar Jaideep Singh2*
1Assistant Professor, 2Post Graduate, Department of Orthopaedics, Shanthiram Medical College and General Hospital, Nandyal.
Email: balupriyareddy@gmail.com
Abstract Background: Standard open reduction and internal fixation techniques have been successful in restoring osseous alignment for proximal tibial fractures; however, surgical morbidity, especially soft tissue infection and wound necrosis, has been reported frequently. Materials and methods: This study of surgical management of proximal tibial fractures was conducted in 50 patients who were treated for proximal tibial fractures of which 25 patients were treated by closed reduction and External fixation with Ilizarov/Hybrid ExFix methods and 25 patients were treated by open reduction and internal fixation with buttress plate and LCP. Out of which 8cases lost for follow up. Results: In the present study there were 18 proximal metaphyseal fractures managed by external fixators. All the fractures united at an average of 14.4 weeks. There were 1 excellent, 9 good, 6 fair results and 3 poor results. There were 6 patients with pin tract infections which healed with regular dressings, 2 patients with knee stiffness, knee pain in 2 patients , 2 patients with delayed union , 2 patient with non union and 1 patient with wire breakage. In the present study there were 23 proximal metaphyseal fractures managed plate osteosynthesis. All the fractures united at an average of 13 weeks. There were 4 excellent, 16 good and 2 fair, 1 poor results. There were 1 patients with superficial infections which healed with regular dressings, no patients(5%) with knee stiffness, 2 patients with knee pain, no patients with delayed union , 1 patient with non union. Conclusion: Plating offers a good treatment option for difficult proximal tibial fractures. When compared with external fixation, plateosteosynthesis provide improved healing rates, restoration of the articular surface, and decreased complications.
Key Words: Proximal Tibia Fracture, LCP, Hybrid EXFIX, Ilizarov.
INTRODUCTION
The proximal tibial fractures involve various fracture configurations. The tibial plateau fractures comprises mainly Lateral condyle, Medial condyle and Bi condylar. Most of these involve articular surface of the tibia , which form part of a major weight bearing joint of axial skeleton of the human body.
Demographically , majority of the patients are young adults with robust health. The majority of the injuries are due to, road traffic accidents. These fractures occurs due to a combination of axial loading and varus or valgus force applied leading to articular dippression. High speed two wheeler riding and Bumper injuries due to direct trauma.
The high energy trauma results in diverse group of injuries ,with various degree of severity, Ranging from simple injuries with predictably excellent results after non operative treatment and Complex fracture patterns that challenge even the most experienced surgeons , and many times results are not very satisfactory. Often these high velocity injuries are associated with Various degree of soft tissue injuries and Many fractures are associated with limb threatening neuro vascular injuries,
like acute compartment syndrome. For the diagnosis of these various intra articular injuries encompassing tibial plateau needs high resolution imaging studies including High quality digital radio graphy, 3-D C.T Studies and MRI Imaging. These imaging studies require to assess the type of fracture, involvement of Articular surface, Stable or unstable and Involvement of supporting soft tissue structures of joint.
1 This will help the treating surgeon to select the best treatment options.
The twentieth century, has seen a lot of changes in medical field especially in orthopaedic trauma. A better understanding of the bio mechanics, quality of implants, principles of internal fixation, soft tissue care, role of antibiotics and asepsis have all contributed to the radical change in the surgical treatment. Thus, treatment concepts are based on restoring or preserving limb alignment will leads to satisfactory results for patients, whereas poor alignment, will result in less satisfactory outcomes.2 Thus, we have advanced from conservative approach to best result oriented surgical management of these fractures as accepted mode of treatment.
We have under taken this study in the high velocity proximal tibial fractures more frequently necessitating plate osteosynthesis and external fixators with specific indications. The results of both types of treatment obtained were compared and relevant conclusions drawn. Proximal tibial fractures are the most common bone injuries that occur during road traffic accidents (High velocity injuries). This is mainly due to its Sub cutaneous nature at almost all levels of the leg.
Soft tissue, muscle coverage, is scanty over antero medial aspect of leg. Thus injuring forces cannot be absorbed or dissipated so that fractures can be prevented.
AIMS
To compare the results of plate osteosynthesis over external fixators.
To restore articular congruity and limb alignment
To mobilize the joint as early as possible, to get back optimal functional Results
MATERIALS AND METHODS
This study of surgical management of proximal tibial fractures was conducted in the Department of orthopaedics’ at Santhiram Medical C0llege between august 2014 to July 2019. Clearance was obtained from hospital ethical committee.
During this period 50 patients were treated for proximal tibial fractures of which 25 patients were treated by closed reduction and External fixation with Ilizarov/Hybrid ExFix methods and 25 patients were treated by open reduction and internal fixation with buttress plate and LCP. Out of which 8cases lost for follow up.
All the required data was collected from the patients during their stay in the hospital, during follow up at regular intervals and from the medical records.
Inclusion criteria:Age above 18 years of either sex with Proximal Tibial Fractures. (METAPHYSEAL andINTRA ARTICULAR)
Exclusion criteria:
Pathological fractures, Fractures in children, Old neglected fractures, Old fractures with implant failure.
SURGICAL TECHNIQUE PLATE OSTEOSYNTHSIS
Prior to the surgery, the patient and close relatives were counselled
A. Regarding the type of anaesthesia andtype of surgery and possible outcome of the
surgery
B. Informed and written consent was taken. Medical evaluation of the patient and necessary treatment was instituted in certain patients where it was necessary. Then the patient was evaluated any risk factors any type of anaesthesia by anaesthetists. All the patients were kept nil orally for 8-10 hrs before surgery.
. All the patients were given head and body bath, the hole limb to be operated was
thoroughly cleaned including the back and private parts. Inj.tetanous toxoid was given along with xylocaine test dose. Adequate compatible blood (whole blood/packed cells) was arranged. The required implanted in assorted sizes and instrumentation set was kept ready in
each case.
Open Reduction and Fixation of a Tibial Plateau Fracture: Apply a tourniquet except in patients with severe soft-tissue injury. I.V antibiotics preferably third generation cophalosporins 1 – 1.5gm to be given 1/2hr before starting surgery. If procedure is delayed one more dose can
be repeated.
APPROACH: For fractures of the lateral condyle, make an anterolateral incision. For medial condyle fractures, straight anterior or anteromedial incision. For complex tibial plateau fractures longitudinal midline incision. On the basis of preoperative radiographs and CT scans, subperiosteally dissect the soft tissues from the more comminuted condyle, creating full-thickness flaps. The dissection should proceed from the midline to the periphery. To buried the implant completely under soft tissue coverage and to avoid necrosis of soft tissue over the implant.
FRACTURE REDUCTION: For lateral and medial depressed condylar fractures Insert a periosteal elevator well beneath the depressed articular fragments, and by slow and meticulous pressure elevate the articular fragments and compressed cancellous bone in one large mass. For complex tibial plateau fractures Place a femoral distractor with pins in the distal femur and tibial shaft from medial to lateral to reduce the fracture by ligamentotaxis. Avoid varus and valgus angulation by using two femoral distractors, one on the medial and one on the lateral side of the extremity. Elevate depressed fragments, and support them with autogenous or allograft bone grafts or hydroxyapatite.
• Using fluoroscopic guidance, reduce and hold the fracture with large bone reduction clamps. Use Kirschner wires as temporary fixation.
PLATE and SCREW FIXATION: Apply an AO contoured large fragment buttress plate / Locking plate to the tibial metaphysis, and extend it down the tibial shaft far enough to stabilize the fracture securely. Insert large cancellous screws/Locking Screws in the proximal part of the buttress plate/Locking plate. Distal portion fixed with cortical screws/locking screws. When the fracture has been adequately stabilized, remove all
temporary fixation devices.
Close the capsular incisions with interrupted sutures, and close the skin and subcutaneous tissue over suction drains size 14 – 16 nos. Place the extremity in a posterior plaster splint with the knee flexed 30 degrees.
MIPPO (Minimally invasive plate osteosynthesis)
A stainless steel 4.5-mm LCP plate or T buttress plate of an appropriate length was precontoured, according to the fracture site. An incision of 2 to 3 cm over the proximal aspect of the tibia on the medial, lateral, or both sides was made, according to the fracture site and the use of single or double plates. A submuscular plane was created and the plate was slid in the anterior submuscular plane. The plate was then fixed with screws, which were inserted percutaneously through the primary surgical incisions. The fixation and reduction should be checked or confirmed by image intensifier. Clouser of the wounds in a single / double layer as situation warrants. Splint (POP slab)/ long leg brace applied.
POST OPERATIVE INSTRUCTIONS FOR PLATE OSTEO SYNTHESIS
BP and TPR hourly
2. Postoperative analgesia
3. To watchout for bleeding
4. Postoperative antibiotics for 7-10 days
5. Foot end elevation (as the surgeries are performed under spinal anaesthesia). 6. Postoperative X-ray preferably the next day. Active mobilization of the ankle, knee and non-weight bearing of the patient using standard walking frame was done from the first post-operative day under the supervision of a physiotherapist. Post-operative check dressing and removal of suction drainage tube to be done after 48-72hrs. Intravenous antibiotic regimen was continued for 5-7 days (12-14 days in compound fractures) after the surgery. Another 5 days of oral antibiotics were advised. Regular cleansing of the pin exit points was done. Patients with extra articular fractures were encouraged to bear weight as early as possible where as those with intra articular fractures were allowed to bear weight after a minimum of 6 weeks after the fixator was applied.
EXTERNAL FIXATION
Operative Procedure:(ilizarov/Hybrid Exfix) : Type of Anaesthesia Lumbar Sub Arachnoid Block Position-supine with affected leg elevated on a pillow/sand bag for distal end fractures and with a pillow under the distal thigh for proximal end fractures.
Securing the peri-articular fragment: After reduction of the peri-articular fragment, it was secured using three Ilizarov wires. The wires were pushed manually till it hit the cortex, then drilled across both the cortices and hammered out through the opposite soft tissue. Nerves and vessels were avoided by the awareness of the anatomy, based on the safe corridor for pin insertion in the lower leg. Olive wires were used if it was deemed necessary for the compression of the longitudinal split was desired. Else bayonet tipped or trocar tipped wires were used. The first wire was passed parallel to the joint in a lateral to medial direction under fluoroscopic control. It is fixed to an appropriate size ilizarov 3⁄4 ring so as to leave at least 2cms between the leg and the ring on all sides. One wire each from posterolateral to anteromedial and posteromedial to anterolateral under fluoroscopic control keeping an angle of 30 to 60 degrees between the wires. The axial plane of the wires was about 5mm from the joint and as parallel to it as
possible. If any internal fixation using cancellous screws was deemed necessary it
was done before passage of the wires. The wires were fixed to the rings using cannulated/slotted wire connecting bolts and
tensioned using a dynamometric tensioner. Skin traction by the wires, if any were released using minimal incisions on the side of
the skin stretching.
FOLLOW UP: Patients were followed up at 4 - 6weekly, 8-10wks, 12-16wks intervals until
fracture union and at once at the end of 1 year. 6 months and 1year thereafter. Periodic follow up of the patient was done at OPD days. A thorough clinical assessment was made regarding the symptoms of pain, discomfort, walking ability, movement of joint, any bony tenderness, any abnormal mobility at fracture site presenting/disappearing and associated pain, any shortening of the limb. Any complications like infection, stiffness of joint, muscular wasting etc. and recorded in detailed in patient proforma sheet. Then followed radiological assessment comparing with previous x-rays. The fracture was said to united when there was bridging callus at the fracture site at least in three cortices in the anteroposterior and lateral views. Trabeculations extending across the fracture site was also taken into consideration.
RESULTS
The following observations were made from the data collected during the study of 50 cases of proximal tibial fractures treated by plate osteosynthesis and Exfix. In our study, maximum age was 80yrs and minimum age was 20yrs. Most of the patients were between 20-60 years. Mean age was 40yrs.
Table 1: Demographic distribution of study cases
Variables |
Plate osteosynthesis |
External Fixation |
Total |
<20 |
0 |
0 |
|
21-40 |
14(69.8%) |
10(52.6%) |
24(57.1%) |
41-60 |
6(26.1%) |
7(36.8%) |
13(30.9%) |
61-80 |
3(13%) |
2(10.5%) |
5(11.9%) |
>80 |
0 |
0 |
|
Total |
23 |
19 |
42 |
Gender |
|
|
|
Males |
18(78.2%) |
13(68.4%) |
31(73.8%) |
Females |
5(21.7%) |
6(31.5%) |
11(26.1%) |
Nature of Injury |
|
|
|
Assault |
1(4.35%) |
0 |
1(2.3%) |
Fall |
8(34.7%) |
2(10.5%) |
10(23.8%) |
Accident |
14(60.8%) |
17(89.4%) |
31(73.8%) |
Affected side of injury |
|
|
|
Right |
13(56.5%) |
11(57.8%) |
24(571%) |
Left |
10(43.5%) |
8(42.2%) |
18(42.8%) |
Type of fracture |
|
|
|
Open |
3(13%) |
12(63%) |
15(35.7%) |
Closed |
20(87%) |
7(37%) |
27(64.3%) |
|
|
|
|
Age distribution of the cases in the two groups were tested using Kalmogrov – Smirnov test for equality distribution. The K-S value of 0.367 was compared with the table value which indicated that the two groups had no significant differences between them at 5 % showing that the groups are comparable. Sex difference between the groups showed a P-value of 0.795 with chi- squared value of 0.067 and chi-squared table value of 3.841. This again showed that there were no significant differences in sex distribution of cases in either group to significantly affect comparison. Nature of violence was tested which gave a P-value of 0.848 with chi-squared value of 0.329 and chi-squared table value of 5.991. This showed that the two groups are comparable. Side affected was again tested for any difference between the two groups. It also showed that the two is comparable with no significance differences between the groups. P-value was 0.602 with chi-squared value of 1.01 and chi-squared table value of 3.841. Distribution of the type of fracture within the two groups showed no significant differences between the groups. P-value – 0.571, chi-squared value – 1.122 and chi-squared table value – 5.991.
Table 2: Gustelo Anderson classification of fractures
Gustelo Anderson classification |
Plate osteosynthesis |
External Fixation |
Total |
I |
1(33.3%) |
3(25%) |
4(26.7%) |
II |
1(33.3%) |
3(25%) |
4(26.7%) |
IIIA |
1(33.3%) |
3(25%) |
4(26.7%) |
IIIB |
0 |
3(25%) |
3(20%) |
Total |
3 |
12 |
15 |
Type based on AO/OTA Classification |
|
|
|
A |
3(13%) |
3(15.8%) |
6(17.2%) |
B |
10(43.5%) |
4(21%) |
7(20%) |
C |
10(43.5%) |
12(63.2%) |
22(62.8%) |
Total |
23 |
19 |
|
Results show a significant difference between the two methods in the anatomical result. P-value = 0.008906 with Odds ratio of 5.2 (at 95 % CI 1.427 – 18.9489). Since only 4 anatomical deformities were noted in the PFN group, small sample test was performed which showed probability of 0.1.
Functional results of the two methods was significantly different. P-value = 0.117, chi-squared stat = 50885 with chi-squared table value = 5. 991.plating superior than exfix.
Table 3: Range of motion achieved after fixation
|
< 100 |
100 - 120 |
120 - 130 |
> 130 |
TOTAL |
Plate osteosynthesis |
1 |
4 |
5 |
13 |
23 |
% |
4.35 |
17.39 |
21.74 |
56.52 |
100.00 |
External Fixation |
3 |
12 |
4 |
0 |
19 |
% |
15.79 |
63.16 |
21.05 |
0.00 |
100.00 |
Total |
4 |
16 |
9 |
13 |
42 |
% |
9.52 |
38.10 |
21.43 |
30.95 |
100.00 |
Duration of fracture union |
13 Weeks |
14 Weeks |
15 Weeks |
> 15 Weeks |
Total |
Plate osteosynthesis |
6 |
8 |
6 |
3 |
23 |
% |
26.09 |
34.78 |
26.09 |
13.04 |
100.00 |
External Fixation |
3 |
4 |
5 |
7 |
19 |
% |
15.79 |
21.05 |
26.32 |
36.84 |
100.00 |
Total |
9 |
12 |
11 |
10 |
42 |
% |
21.43 |
28.57 |
26.19 |
23.81 |
100.00 |
In the present study, there were 19 proximal metaphyseal fractures managed by external fixators. All the fractures united at an average of 14.4 weeks. There were 1 excellent, 9 good, 6 fair results and 3 poor results. In the present study, there were 23 proximal metaphyseal fractures managed plate osteosynthesis. All the fractures united at an average of 13 weeks. There were 4 excellent, 16 good and 2 fair, 1 poor results.
Table-4: Patients with proximal tibia fractures were evaluated by; The American Knee Society Score (Insall Modification) as follows
Pain 50 (Maximum)
Walking
None
Mild or occasional Moderate
Severe
Stairs
None
Mild or occasional Moderate
Severe 35 30 15 0
15 10 5 0
R.O.M. 25 (Maximum)
8o 1 point
Stability 25 (Maximum)
Medial/Lateral
0-5 mm
5-10 mm
> 10 mm Anterior/Posterior 0-5 mm
5-10 mm > 10 mm 15 10 5
10 8 5
Deductions
Extension lag
None
<4 degrees 5-10 degrees >11 degrees 0 -2 -5 -10
Flexion Contracture
< 5 degrees 6-10 degrees 11-20 degrees > 20 degrees 0 -3 -5 -10
Malalignment
5-10 degrees (5o = -2 points) 0
Pain at rest
Mild
Moderate
Severe
Symptomatic plus objective -5 -10 -15 0
Table 5: KSS score with proximal tibial fracture
|
80 - 100 |
70 - 70 |
60 - 69 |
< 60 |
Total |
Plate osteosynthesis |
4 |
16 |
2 |
1 |
23 |
% |
17.39 |
69.57 |
8.70 |
4.35 |
100.00 |
External Fixation |
1 |
9 |
6 |
3 |
19 |
% |
5.26 |
47.37 |
31.58 |
15.79 |
100.00 |
Total |
5 |
25 |
8 |
4 |
42 |
% |
11.90 |
59.52 |
19.05 |
9.52 |
100.00 |
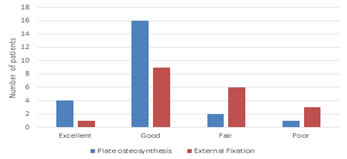
Figure 1: Comparison of the overall response of the two methods studied
Finally, the two techniques were compared for excellent and less than excellent result which showed an Odds ratio of 2.1666 (at 95 % CI 0.7167 – 6.5502).
Table 6: Complications of the proximal tibial fractures
|
Infection |
Knee Pain |
Knee Stiffness |
Non-union |
Total |
Plate osteosynthesis |
1 |
2 |
0 |
1 |
4 |
% |
25.00 |
50.00 |
0.00 |
25.00 |
100.00 |
External Fixation |
6 |
4 |
2 |
2 |
14 |
% |
42.86 |
28.57 |
14.29 |
14.29 |
100.00 |
Total |
7 |
6 |
2 |
3 |
18 |
% |
38.89 |
33.33 |
11.11 |
16.67 |
-
|
In the present study, there were 19 proximal metaphyseal fractures managed by external fixators. All the fractures united at an average of 14.4 weeks. There were 1 excellent, 9 good, 6 fair results and 3 poor results. There were 6 patients with pin tract infections which healed with regular dressings, 2 patients with knee stiffness, knee pain in 2 patients, 2 patients with delayed union, 2 patients with non-union and 1 patient with wire breakage. In the present study, there were 23 proximal metaphyseal fractures managed plate osteosynthesis. All the fractures united at an average of 13 weeks. There were 4 excellent, 16 good and 2 fair, 1 poor results. There were 1 patient with superficial infections which healed with regular dressings, no patients with knee stiffness, 2 patients with knee pain, no patients with delayed union, 1 patient with non-union.
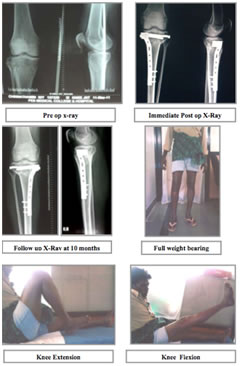
Figure 2: Clinical case in present study
Pre OP X-Ray Immediate Post OP X-Ray
Immediate Post OP X-Ray 7 months follow-up X-Ray
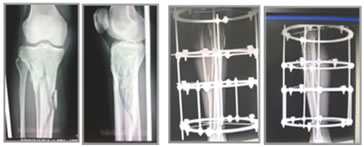
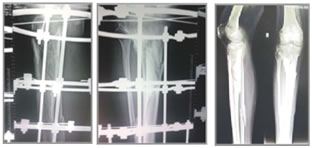
Figure 3: Clinical case of complex proximal metaphyseal fracture- fair result
DISCUSSION
Proximal tibial fractures are the most difficult fractures to treat effectively. The status of the soft tissues, the degree of comminution and articular cartilage damage sustained at the time of injury affect the long term clinical results. The goal of operative treatment is to obtain anatomic realignment of the joint surface while providing enough stability to allow early motion. This should be accomplished using techniques that minimize osseous and soft tissue devascularisation in the hopes of decreasing the complications resulting from treatment. The present study was under taken to determine the efficacy of the External Fixator and Plate Osteosynthesis in the treatment of the Proximal tibial fractures. We evaluated our results and compared them with those obtained by various other studies. Our study consists of 50 cases of various groups of age, sex, type of violence, side involved, fracture geometry, type of fixation used, complications met with out of 50cases, 8cases were lost for regular follow-up and we were able to assess the results for 42 cases. Our study revealed the average age of patients with such injuries to be 40 Range 27 to 67 years which is comparable to that of other studies.
Table 7: Mechanism of injury
Comparison of Mechanism of Injury
Study |
Mode of Injury |
High Energy (RTA, Fall from height) |
Low Energy (Assault, Simple Fall) |
Gaudinez et al. 3 |
93% |
7% |
Anglen et al. 4 |
68% |
32% |
Agarwal et al. 5 |
87% |
13% |
Barbieri et al. 6 |
75% |
25% |
Ovadia and Beals 7 |
46% |
54% |
Present study |
88% |
12% |
In our study, the male preponderance for such kind of injuries were high compared to the study by Barbieri et al., which was 59% possibly due to the fact of male dominance over the female in traveling, occupational injures etc., in India However, the study by Kumar et al. were comparable in the fact that they had 72% male. 8 Gaudinez et al.3 observed 93% high energy fractures in his study. Ovadia and Beals could attribute only 46% of such injuries to be of high energy.7 However, our present study correlates with the study conducted by Agarwal et al. who had a percentage of 87% being high energy. 5 Our study had 31% open injuries. This was comparable to studies conducted by Kumar et al. and Guadinez et al.. Ovadia and Beals who reported 20% open injuries. 3,7,8Barbieri et al. however had 30% of open injuries .6
Table 8: Comparison of clinical fracture type
Study |
Open fracture Percentage |
Closed fracture Percentage |
Gaudinez et al. 3 |
21% |
79% |
Agarwal et al. 5 |
86% |
14% |
Ovadia and Beals7 |
20% |
80% |
Kumar et al. 8 |
39% |
61% |
Barbieri et al. 6 |
30% |
70% |
Present study |
31% |
69% |
Table 9: Fracture Patterns
Study |
A1 |
A2 |
A3 |
B1 |
B2 |
B3 |
C1 |
C2 |
C3 |
Kumar et al.8 |
- |
- |
- |
- |
- |
- |
11 |
35 |
11 |
Present Study |
3 |
10 |
7 |
- |
4 |
7 |
- |
7 |
4 |
Table 10: Time to union
Table : Comparison of time to union
Study |
Method |
Time to union in weeks (ave) |
Kumar et al. 8 |
Hybrid ex fix proximal tibia |
24.7 |
Anglen et al.4 |
Hybrid ex fix Proximal tibia |
20 |
Guadinez et al. 3 |
Ilizarov ex fix proximal tibia |
18 |
Wrysch et al. 9 |
Spanning ex fix |
15 |
Present Study |
ex fix plate Osteosynthesis |
16 13.5 |
The average time for fracture union in various studies conducted using various was 13-25 weeks. Our study had an average fracture union of 14 weeks which were comparable with studies conducted using the hybrid external fixator. (Barbieri et al. had an average fracture union of 14 weeks and Gaudinez el al had an average of 13 weeks for the proximal tibia. Where as for the proximal tibia, Kumar et al. 48 had an average of 24.7 weeks .)
The study conducted by Guadinez et al. in the management of communited tibial plateau fractures by hybrid external fixation, which were include 93% were high velocity injuries.3 They had 4(22%) pin tract infections and 3(17%) varus malalignment. Kumar et al. in a study o group of patients , had an incidence of 3(5%) malunions and 4(7%) osteomyelitis. All patients in this series had pin tract infection at sometime during the course of treatment. Rademakers et al. in their study of 202 tibial plateau fractures treated by ORIF , had the following complications .11 patients (5.4%) developed a deep wound infection within the first 2 weeks after treatment. In 8 patients (4.0%), a malunion of the fracture developed. One of the common complications encountered in surgical group of patients was infection. The rate of infection was 16.3%. All the infections were superficial infection and healed with time.
Lachiewicz and Funcik10reported 10% moderate to severe incidence of osteoarthritis in their study of 43 patients over an average follow up period of 2.7 years. Jensen et al. reported a 22% incidence of osteoarthritis in their study of 109 fractures of all varieties followed up over an average period of 6 years. They attributed this high percentage to meniscectomy done at the time of surgery. Rasmussen reported 17% incidence of post traumatic osteoarthritis. They observed that arthritis was more frequent with bicondylar fractures, varus deformity and unstable knees in extension.
In the present study of exfix, there were 6 patients with pin tract infections which healed with regular dressings, 2 patients with knee stiffness, knee pain in 2 patients , 2 patients with delayed union , 2 patient with non union and 1 patient (with wire breakage. In the present study of plate osteosynthesis ,there were 1 patient with superficial infections which healed with regular dressings, no patients with knee stiffness, 2 patients with knee pain , no patients with delayed union , 1 patient with non union. Gaudinez et al. based their study on the scale by Ovadia and Beals with 64% patients having good to excellent objective results, and 71% patients had good to excellent objective results , complications included superficial pin tract infections in 3 patients.3,7 Aggarwal et al. in their study of hybrid external fixation of high energy peri articular fractures of the tibia had results that were good to excellent in 30(86%), fair in 2(6%)and poor in 3(8%).5 Stannard et al. studied 34 tibial plateau fractures treated by LISS.11 All of the fractures healed without additional surgical intervention or bone grafting. The average time to radiographic callus was 6.1 weeks, and the average time to complete union was 15.6 weeks. The articular step-off average was 0.8 mm, with a range of 0 to 5 mm. The postoperative alignment demonstrated 2 patients(6%) with a malunion. There were 2(6%) superficial wound infections and no cases of deep infection or osteomyelitis. Stamer et al. studied 22 patients with Schatzker type VI tibial plateau fractures were treated with a hybrid ring external fixator.12 8 patients were treated with limited open reduction and internal fixation before application of the frame. 14 patients had percutaneous cannulated screw fixation to stabilize the articular surface without opening the fracture site. Average time to healing was 4.4 months. 4 flexion contractures(18%) of 5-15degrees. Complications consisted of 3 deep wound infections(14%), 1 deep venous thrombosis (DVT)(5%), 1 malunion(5%), and 1(5%) pin tract infection. There were 13 excellent(59%),3 good(13%), 1 fair(5%), and 6 poor results(23%). In the present study there were 19 proximal metaphyseal fractures managed by external fixators. All the fractures united at an average of 14.4 weeks. There were 1 excellent, 9 good , 6 fair results and 3 poor results. There were 6 patients with pin tract infections which healed with regular dressings, 2 patients with knee stiffness,knee pain in 2 patients , 2 patients with delayed union , 2 patient with non union and 1 patient with wire breakage. In the present study there were 23 proximal metaphyseal fractures managed plate osteosynthesis. All the fractures united at an average of 13 weeks. There were 4 excellent, 16 good and 2 fair , 1 poor results. There were 1 patient with superficial infections which healed with regular dressings, no patients with knee stiffness, 2 patients with knee pain , no patients with delayed union , 1 patient with non union.
CONCLUSION
Our study demonstrates improved outcomes in the locked plating group based on several variables evaluated. The 12% higher union rate at 6 months is superior to that of the external fixation group. The average time to union was superior in the plating group (13.5 VS 16 weeks), although the overall nonunion rates at latest follow-up were similar . The improved healing rate may potentially be related to the fixation characteristics of the locking plates, increased use of bone grafting, and/or a more adequate reduction. It should be noted that the overall union rate of 90% is supported by numerous studies in the literature that report union rates of 94% to 100% with plating.
Significant loss of knee ROM was less in the plating group than in the external fixation group (4% vs 13%). This may be attributable to the soft tissue impingement inherent to external fixator pins. In addition, the decreased time to union seen in the locked plating group may have allowed for earlier ROM. Plating offers a good treatment option for difficult proximal tibial fractures. When compared with external fixation, plateosteosynthesis provide improved healing rates, restoration of the articular surface, and decreased complications. On the other hand, External fixation offers a good bridge to plating or definitive treatment modality in cases with severe soft tissue injury, severe comminution, unstable patients, and should therefore remained in our treatment modalities
REFERENCES
1. Watson JT, Schatzker J. Tibial plateau fractures. In: Browner B, Jupiter JB, Levine AM, Trafton PG, eds. Skeletal Trauma. 3rd ed. Philadelphia, PA: WB Saunders; 2003:2074-2130.
2. Gösling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C. Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma. 2004; 18(8):546-551.
3. Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation of comminuted tibial plateau fractures.Clin Orthop Relat Res. 1996; (328):203-210.
4. Anglen J O, Burd T A, Hendricks K J, Harrison P. The “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma 2003; 17(9): 625–34.
5.
Agarwal T, Salgia A, Biswas SK, Sanghi S, Puri SR. Management of closed tibial plateau fractures with percutaneous cancellous screw fixation. Med J DY Patil Univ 2013;6:43-8.
6. Barbieri R, Schenk R, Koval K, Aurori K, Aurori B: Hybrid external fixation in the treatment of tibial plafond fractures. Clin Orthop Relat Res:1996 Nov;(332):16-22.
7. Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg Am. 1986 Apr;68(4):543-51.
8. Kumar A, Whittle AP. Treatment of complex (Schatzker type VI) fractures of the tibial plateau with circular wire external fixation: retrospective case review. J Orthop Trauma. 2000; 14(5):339-344.
9. Wrysch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD, Schwartz HS: Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am. 1996, 78–11: 1646-1657.
10. Lachiewicz PF, Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop Relat Res. 1990; (259):210- 215.
11. Stannard JP, Wilson TC, Volgas DA, Alonso JE. The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma. 2004; 18(8):552-558.
12. Stamer DT, Schenk R, Staggers B, Aurori K, Aurori B, Behrens FF. Bicondylar tibial plateau fractures treated with a hybrid ring external fixator: a prelimary study. J Orthop Trauma. 1994; 8(6):455-461.
Policy for Articles with Open Access:
Authors who publish with MedPulse International Journal of Orthopedics, (Print ISSN: 2579-0889, Online) (ISSN: 2636-4638) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
 Home
Home
