|
Table of Content - Volume 15 Issue 2 - August 2020
Prediction of radiological measurements of proximal humerus fractures treated with PHILOS plate using a prognostic multiplication factor
Charles Abraham1, Nithin Thomas Philip2*, Pramod Thomas3, Sherin Rebeka Philip4, Prem Kishore5, Anmaria Babu6
{1Associate Professor, 2Assistant Professor, 4,5Junior Resident, 6Pharm D Intern, Department of Orthopaedics} {3Biostatistician, Department of Community Medicine} Believers Church Medical College Hospital, Thiruvalla 689103, INDIA. Email: drcharlesabraham@gmail.com, drnithintphilip@gmail.com
Abstract Background: The increased incidence of osteoporosis and advanced age predisposes to an increase in Proximal Humerus fractures. It accounts for about 4-5% of all fractures and is the third most common fracture in patients above 65yrs of age. This study was planned to evaluate the short term and long-term radiological results of PHILOS (Proximal Humerus Internal Locking System) plating in fractures of proximal Humerus and to formulate a multiplication factor that determine the prognosis of the fixation as early as 6 weeks for early intervention and management. Materials and Methods: This is a cross sectional analytical study conducted in our institution using data obtained from radiological evaluation of patients who were treated for proximal humerus fracture between August 2016 and August 2019 with open reduction and internal fixation with PHILOS plating. Results: A total of 83 patients were included in the study, out of which 27(32.53%) were males and 56(67.47%) females. The height loss and angle loss in immediate post op to 6 weeks (height (P =<0.001), angle (P= <0.001)), 6 weeks to 3 months (height (P= 0.001), angle (P=<0.001)) and total loss from immediate post (height (P= <0.001) angle (P=<0.001) were statistically significant. Linear regression analysis method was used to obtain a multiplication factor 0.98 with a constant value 6.001 by keeping the humeral head height loss at 1 year as dependant variable and that of 6 week as independent variable with confidence interval 0.885 to 1.069. Conclusion: There is a significant height and angle loss in 0 to 6 weeks post fixation and thereafter it remains stable. Based on the 6 weeks, percentage height and angle loss at 1-year can be calculated by the multiplication factor (0.98 +6.001) for height with confidence interval 0.885 to 1.069 and (0.992 +3.843) with confidence interval 0.915 to 1.070 for angle so that if its more than 50 percent then early intervention can be done to prevent fixation failure. Key Word: proximal humerus fractures.
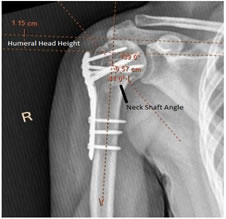
INTRODUCTION The increased incidence of osteoporosis and advanced age predisposes to an increase in Proximal Humerus fractures. It accounts for about 4-5% of all fractures and is the third most common fracture in patients above 65yrs of age. Undisplaced or Minimal displaced fractures can be treated conservatively with closed reduction and cast or sling application but displaced fractures require anatomical reduction with internal fixation Depending upon the patients age, level of activity, medical co-morbidities and fracture pattern various treatment modalities had been proposed which include conservative treatment , percutaneous fixation , Internal fixation with PHILOS plating and joint replacement , . Conservative management and percutaneous K-wire fixation has limited indications and may not ensure anatomical reduction and early mobilisation. It is also associated with a long recovery period5. Better clinical results were obtained by many authors with open reduction and internal fixation and claim to have the advantages of anatomical reduction and early mobilisation. The introduction of PHILOS systems has redefined the treatment of proximal humerus with the advantage of increased skeletal anchorage and higher resistance to failure by increasing the axial and angular stability ( , ). These plates do not compromise periosteal blood supply as the biomechanics does not depend on friction or compression between the plate and bone to stabilize the fracture ( , ). The aim of this study was to evaluate the short term and long-term radiological results of PHILOS (Proximal Humerus Internal Locking System) plating in fractures of proximal Humerus and to formulate a multiplication factor that determine the prognosis of the fixation as early as 6 weeks for early intervention and management. MATERIALS AND METHODSThis is a cross sectional analytical study conducted in our institution using data obtained from radiological evaluation of patients who were treated for proximal humerus fracture between August 2016 and August 2019 with open reduction and internal fixation with PHILOS plating. Post Op X-rays were collected from PACS software database for immediate post op (n=83), 6 weeks(n=82), 3 months(n=65), 6 months(n=39) and 1 year (n=13). The age of the patients was divided into 3 groups (up to 60yrs, 61-70yrs, more than 71yrs) and their significance with total height and angle loss percentage were assessed. Humeral Head Height and Neck Shaft angle were calculated by 3 different individuals and the average is taken for statistical analysis. In our study the percentage loss of total humeral head height and neck shaft angle was classified into mild (0 -30%), moderate (31-49%) and severe (more than 50%) for analysis purpose. The fracture was classified based on Neer`s classification and presence of calcar screw and the number of screws were also noted for further statistical correlation in each sub-group. Using SPSS software statistical analysis was done to find the relation of humeral head height and neck shaft angle with number of screws, Neer’s classification subgroups and the presence or absence of calcar screws. In addition to the descriptive measures we applied independent t test, paired t test and analysis of variance.
Figure 1
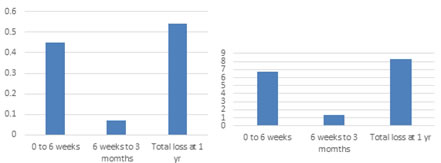
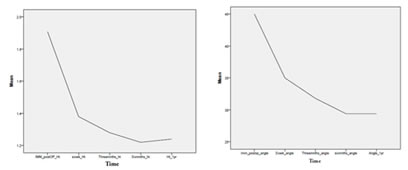
RESULTSA total of 83 patients were included in the study, out of which 27(32.53%) were males and 56(67.47%) females. Patients which has no follow-up and non-standard AP X-rays were excluded from the study. Total average height loss percentage in males was (25.7±21.5) and that of females were (36.6±26.5). Similarly, the total average angle loss percentage in males was (22.6±19.8) and in females (18.6±15.2) at the end of 1 year. Both being not statistically significant using paired t test. The age of the patients were also categorized into 3 groups (up to 60yrs, 61 to 70yrs and more than 71yrs) and the relation of the age with percentage height and angle loss were assessed using ANOVA and found that it’s not significant. The height loss and angle loss at immediate post op to 6 weeks, 6 weeks to 3 months and total loss from immediate post op till one year was calculated. Statistical analysis using paired t test shows that the height loss and angle loss in immediate post op to 6 weeks (height (P =<0.001), angle (P= <0.001)), 6 weeks to 3 months (height (P= 0.001), angle (P=<0.001)) and total loss from immediate post (height (P= <0.001) angle (P=<0.001) were statistically significant. Figure 2: Height loss Figure 3: Angle loss We also found the relationship between humeral head height and neck shaft angle loss percentage at 6 weeks to that of 1 year as a prognostic factor for early intervention. Linear regression analysis method was used to obtain a multiplication factor 0.98 with a constant value 6.001 by keeping the humeral head height loss at 1 year as dependant variable and that of 6 week as independent variable with confidence interval 0.885 to 1.069. Hence the humeral head height loss percentage at 6 weeks multiplied by 0.98 +6.001 can give the total height loss percentage at 1 year. Similarly, the neck shaft angle loss percentage linear regression analysis was done to obtain a multiplication factor 0.992 with a constant value of 3.843 by keeping the neck shaft angle loss at 1year as dependant variable and that of 6 weeks as independent variable with confidence interval 0.915 to 1.070. Hence the neck shaft angle loss percentage at 6 weeks multiplied by 0.992 + 3.843 gives the angle loss percentage at 1 year. The total height and angle loss percentage was divided into 3 sub-groups of (0 to 30%) mild (nHeight =62, nAngle=45), (31 to 49%) moderate (nHeight=17, nAngle=15) and (50% or more) severe (nHeight=4, nAngle=22). 54.4% total height loss and 74.7% total angle loss in patients was in the 0 to 30% or mild group, suggesting good angular stability of the fixation.
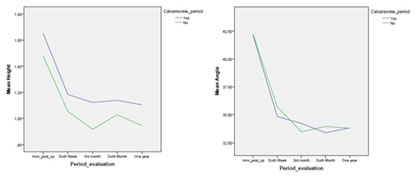
Figure 4; Figure 5 52 (62.65%) patients had right sided injury and 31(37.35%) had left side injury. No significant difference in height and angle loss percentage were noted for the side of injury. Using Neer’s classification the fractures were divided into two part (n=13), three part (n=56) and four part (n=14) with maximum number of cases in the three-part group. We also tested whether there is any significant difference in fracture fixation stability according to Neer`s classification on total percentage height loss (p-value >0.05) and angle loss (p-value >0.05) using Analysis of variance test and could not find a statistically significant difference. The presence (n=39) or absence (n=44) of the calcar screw in each classification group was also noted and the total percentage height and angle loss was calculated for the groups with (31.7±25.6, 19.2±18.6) and without (34.2±15.5, 20.5±15.2) calcar screw. Even though the mean total height and angle loss percent was less in the group with the calcar screw, we were not able to find statistically significant difference in the groups with (P=0.65) and without (P=0.74)calcar screw using paired T-test.
Figure 6; Figure 7 Using ANOVA test the statistical significance of calcar screw in each Neer’s classification group was analysed. Even though it was found to be not statistically significant (P value >0.05) the percentage height loss and angle loss was little in all sub-groups with calcar screw. Table 1
Patients were divided into 3 groups according to the number of screws used for their fracture. Group 1 (n=22) with 2, 3 or 4 screws, group 2 (n=45) with 5 or 6 screws and group 3 (n=16) with 7 or 8 screws. The mean total height and angle loss percentage respectively for Group 1 (27.8±21.2, 21.1±17.8), Group 2 (37.4±27.5, 19.9±17.6) and Group 3 (28.0±22.3, 18.2±13.8), were also not statistically significant. Although we had no Avascular necrosis of the humeral head in our study group there were three patients with implant cut out in our study. DISCUSSIONWith the increased use of angular stable plate osteosynthesis, the need for calcar screws, number of screws and fracture type has been studied by many authors for height and angle loss after fixation. The need for a prognostic factor to determine the early intervention was not stressed upon. We found a multifaction factor for height and angle loss percentage calculation at the end of 1 year using the 0 to 6 weeks height and angle loss percentage so that early intervention can be done at 6 weeks itself if the results at 1 year is not in the acceptable limits. Osterhoff in his study showed that the placement of calcar screws is associated with less secondary loss of reduction by providing inferomedial support but suggested a larger period of follow-up but Katthagen in his study showed that additional calcar screws alone did not improve the initial biomechanical properties of an unstable 2-part proximal humeral fracture model. The use of calcar screws in humerus with varus deformity showed no biomechanical superiority was suggested by Bai, Lu MD et.al. In our study also we could not establish a significant difference in the percentage loss of height and angle with calcar screw placement, Neer’s classification subgroups and the number of screws applied. This may be due to the multifactorial nature of the stability of fixation which depends on inferomedial cortical contact, good anatomical reduction, valgus fixation, co-morbidities, and surgical approach. Moreover, the method of measuring the head-plate distance has been described previously but highly depends on a similar humeral rotation on the true AP radiographs ( , ) defined by rotating the patient 40° towards the affected side ( , ).Though we had no radiological evidence of AVN in 1year x-ray for our patients, 3 patients had implant loosening and cut out which may be attributed to the severity of the fracture (Type 3 and 4), inadequate number of screw fixation (4-5 screws), no calcar screw and severe osteoporotic bone quality. CONCLUSIONIn our study we found that there is a significant loss of humeral head height and neck shaft angle in 0 to 6 weeks and 6 weeks to 3 months post fixation and thereafter it remains stable. Based on the 6 weeks percentage height and angle loss 1-year approximate percentage loss can be calculated by this multiplication factor 0.98+6.001 for height with confidence interval 0.885 to 1.069 and 0.992 +3.843 with confidence interval 0.915 to 1.070 for angle. Hence if the percentage height and angle loss at 1 year calculated using 6 weeks data is more than 50 percent then early intervention can be done to prevent fixation failure. Follow up study is planned to validate the above findings. Though the maximum number of patients with percentage height and angle loss percentage were in the mild group for those with calcar screw, we were not able to establish a statistical significance. This may be due to a good anatomical reduction with infero-medial support and adequate screw placement in the head to prevent collapse. A larger study population may be needed to establish a significant difference about the calcar screw placement. Although we had 3 patients with aseptic implant loosening none of our patients had avascular necrosis.
.
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Forensic Medicine (Print ISSN: 2579-0935) (Online ISSN: 2636-4735) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home