|
Table of Content - Volume 16 Issue 2 - November 2020
Uidesh Yadav1*, Bharth N2, Vaithilingam Ramaiyah Vignesh3, Akhil Chakrawarty4
1,4JR, 2Associate Professor, Department of Orthopaedics, AVMC and H, Puducherry, INDIA. 3SR, Department of Orthopaedics, IGGG Hand PGI, Puducherry, INDIA. Email: yudheesh95@gmail.com
Abstract Background: Proximal humerus fractures account for approximately 5% of all fractures. Stable minimally displaced fractures can be treated nonoperatively but the management of displaced fractures remain controversial with various modalities of treatment available. Aim: This study was aimed at determining the rate of union, complications, operative risks and comparing the clinical functional outcome following ORIF (PHILOS plating) with CRIF (percutaneous K-wire fixation) for 3 and 4-part proximal humerus fracture patients. Methodology: study was conducted at AVMC and H from 10-2017 till 10-2019 in orthopaedics department, total 44 patients with 3 and 4-part proximal humerus fracture (ORIF (PHILOS): 21; CRIF (K-wire) :23), Neer’s classification of proximal humerus was used to classify fracture, minimum 6 months follow-up, Functional outcome was assessed using Constant-Murley shoulder score. Results: Of the 21 patients (ORIF with PHILOS), all fractures united radiologically and clinically and average constant score at final follow-up was 85.29. Of the 23 patients (CRIF with K-wire), average constant score at final follow-up was 79.48. Conclusion: Our study demonstrates that locking plate fixation gives good functional outcomes in treatment of proximal humerus fractures. Our results are comparable to various studies conducted by other authors which states that locking plates(PHILOS) provide better functional and radiological outcomes as compared to other fixation methods like percutaneous K-wire fixation, non-locking plates, intramedullary nails, Tension band wiring. Key Word: proximal humerus fractures.
INTRODUCTION Proximal humerus fracture has become one of the most common fracture encountered now a day in orthopaedic clinics. And this recent increase in the incidence of this injury is because of increase of machineries in daily life routine of man. Road traffic accidents have major part in it. Proximal humerus fracture treatment does not have major complications but when affects the working person it leads to loss of working hours for months and temporary disability. In such cases it becomes important to restore the function of limb. Treatment of this injury is purely depended on the classification and according to types non-operative and operative treatment is decided by the orthopaedic surgeon. As non-union rate is low, non-operative treatment is preferred for the minimal displaced fractures. And in old and osteoporotic bones minimally invasive techniques are used. Treatment for proximal humerus fracture is daily evolving and new implants are being designed by implant companies. Whereas when fracture is severely comminuted and displacement is more preferred treatment is hemiarthroplasty. Minimal amount of malunion which do not hamper the function of limb or cosmetically can be accepted. Whether to choose non-operative treatment or go with surgical procedure can be debatable as there are many studies favouring the both modalities. We conducted a study at our institute and its main purpose was to compare functional outcome of two modalities as treatment of proximal humerus fracture. Modalities were percutaneous pinning and open reduction and internal fixation with PHILOS. In this study the complications (osteonecrosis, malunion, non-union, infection, neurovascular injury, adhesive capsulitis) rate following procedures were also compared. AIMS AND OBJECTIVES
MATERIALS AND METHODOLOGY A comparative study of functional outcome following proximal humeral interlocking osteosynthesis plating versus percutaneous pinning in proximal humerus fractures was carried out from September 2017 to September 2019 in orthopaedic department of Aarupadai Veedu Medical College and Hospital Puducherry. Total 44 patients of proximal humerus fractures were treated with ORIF using PHILOS (21 patients) and CRIF with percutaneous pinning (23 patients) during this period. Inclusion criteria:
Exclusion criteria:
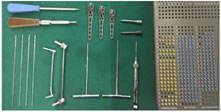
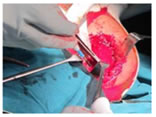
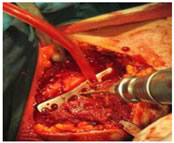
All patients were admitted from casualty or OPD. Figure 1: Instruments used for ORIF with PHILOS PHILOS plate. Power drill. 3.2mm drill bit. 3.2mm drill guide. 3.2mm tap. 3.2mm screw set. Depth gauge. 3.2mm screw driver. And general surgical instruments i.e. artery forceps, retractors, periosteal elevator, reduction clamp, bone lever. PROCEDURE Under GA. position: supine; folded towel under injured shoulder Figure 2: position of patient From nape of neck, injured side chest, axilla and till finger tips were painted with betadine solution. patient draped with sterile linen approach: Delto-pectoral approach was used for dissection to reach bone and fracture site. Incision was starting just distal to coracoid process and as extended 12-14 cm towards lateral side of the biceps tendon. Skin, subcutaneous tissue (fat, fascia) were divided. Important neurovascular structures were identified and retracted gently. Cephalic vein was given extra care. With the blunt dissection, a space was developed between lateral aspect of proximal humerus and deltoid. In this space Hohman’s retractor was placed. Figure 3: per-op blunt dissection Deltoid muscle insertion anteriorly on the shaft of humerus was relieved as this improves the exposure and makes space for plate. Under the guidance of fluoroscopy fracture was reduced and was provisionally fixed with K-wire as a temporary fixation. Plate was placed over the fracture laterally after conforming accurate position it was secured to head of humerus and shaft with k-wires. Figure 4: Per-op placing plate Then screws were placed after checking stability of the fixation wound wash was given with normal saline and metronidazole Figure 5: Per-op screw placement Wound was closed in layers with vicryl and skin stapples or ethilon suture. Figure 6: Per-op closure in layers Sterile dressing was done and patient was shifted to post-operative ward for observation.
POST-OPERATIVE CARE NPO for 6 to 8 hrs. IVFs were continued as per patient. V antibiotics total 6 doses were given. analgesics as per patient complaints. arm pouch was used for immobilization of operated upper limb. same day of surgery post-op check x-ray was taken. dressing and wound inspection was done on the 2,5,7 post-op day. suture removal was done on POD 12 Figure 7: post-op day 12 for suture removal At discharge patient was advised for immobilisation of operated arm for 2 weeks and arm pouch was given. Tight fist and gentle movement of elbow was advised. Rehabilitation programme was started after 2 weeks of surgery. REHABILITATION PROGRAMME Pendulum exercises at operated shoulder were started after 2 wks of surgery. Gentle range of motion exercises at the operated shoulder were started at the end of 2 weeks. 3 simple and easy exercises were told to the patients which he/she could at his/her residence without any supervision
TECHNIQUE 2: PERCUTANEOUS K-WIRE FIXATION
Figure 8: Instruments used in percutaneous k-wire fixation 1.5 -3 mm k-wire. Power Drill. Bone hook. K-wire bender. K-wire cutter. Plyer Procedure Patient in supine position with folded towel under to be operated shoulder. The humeral shaft and head segment are therefore aligned at the surgical neck by placing the arm into adduction and internal rotation. Apex anterior deformity is corrected with a posterior force and K-wires placed as for two-part surgical neck fractures. The arm is then placed into neutral rotation and abduction. A percutaneously placed bone hook is used to secure the greater tuberosity and to reduce it into the correct position. Fixation is achieved with two K-wires placed from the tuberosity and directed into the medial cortex of the proximal humerus. Access to the head is gained through the split between the greater and lesser tuberosities, almost invariably 5 mm behind the bicipital groove. Once coronal alignment of the head has been corrected, the head is fixed with two pins from the distal lateral humeral cortex into the humeral head. By reducing the humeral head, the greater tuberosity will usually regain its anatomic position, tethered by the bridging periosteum distally and the rotator cuff proximally. The greater tuberosity is then fixed either with K wires. These should be directed into the head proximally and into the shaft distally. The arm is then brought into 70 degrees of abduction and internal rotation to obtain an axillary view of the shoulder to visualize the profile of the anterior proximal humerus. The lesser tuberosity is then controlled with a bone hook and reduced under fluoroscopic guidance into its anatomic position. The arm is then mobilized under fluoroscopic visualization to confirm adequate stability. The lateral pins are cut to allow subcutaneous placement. Postoperative Care: NPO for 6 to 8 hrs. IVFs were continued as per patient. I. V antibiotics total 6 doses were given. analgesics as per patient complaints. arm pouch was used for immobilization of operated upper limb. same day of surgery post-op check x-ray was taken. at discharge patient was advised for immobilisation of operated arm for 4 weeks and arm pouch was given. tight fist and gentle movement of elbow was advised. rehabilitation programme was started after 4 weeks of surgery. as radiological sign of union was visible and clinically also it was evident k-wire were removed under local anaesthesia REHABILITATION PROGRAMME Pendulum exercises at operated shoulder were started after 4 weeks of surgery. Gentle range of motion exercises at the operated shoulder were started at the end of 4 weeks. 3 simple and easy exercises were told to the patients which he/she could at his/her residence without any supervision
After 7 weeks completion ROM exercises with gravity resistance without any assistance were started. Follow up: Follow-up schedule for all patients was same despite of technique used for their treatment of proximal humerus fracture. For the first month after surgery patients were called every week and were examined. For the second month, they were called with an interval of 15 days. Once the signs of union were evident the interval between the visits was increased and it became once in a month but patient was on regular physiotherapy. For tenderness, instability, deformity and movements the operated shoulder was examined on each visit. X-rays were taken at each visit for the patients who underwent CRIF with K-wires to know about progressive fracture union and implant position whereas with patients operated with the ORIF with PHILOS radiographs were obtained at 2 weeks apart. According to the stage of fracture union rehabilitation programme was adjusted for the patients. Patients were followed up minimum for 6 months. Constant and Murley score was used for assessing the functional outcome of the patients.
RESULTS AND OBSERVATION Our study consists of 44 patients of fresh 3 and 4-part fracture of proximal humerus which were treated surgically with open reduction and internal fixation using PHILOS system in 21 patients and closed reduction and internal fixation with k-wire in 23 patients from august 2017 to February 2019. All patients were followed for total 6 months with every week one visit for first month, then every 2 weeks one visit and then one visit in every month. Results were analysed both clinically and radiologically. mode of injury by which patient sustained proximal humerus fracture. In the group of CRIF with k-wire fracture, 11patients (47.8%)had simple fall and 12 (52.2%) patients had road traffic accident. Whereas in 21 patients who were treated with ORIF with PHILOS system fracture occurred by simple fall in 9(42.9%) patients and 12(57.1%) patients sustained fracture by road traffic accident. age incidence in our study. Age was divided into intervals of 21-40, 41-60 and >60yrs. In group which was treated with k-wire 6 patients belonged to 21-40yrs of age, 14 patients belonged to 41-60yrs of age and 3 patients were more than 60yr old. Whereas in group treated with PHILOS had 4 patients with 21-40yr of age, 13 were with 41-60yr of age and 4 were more than 60yr of age. mean age of patients in our study. Mean age in patients treated with PHILOS was 50.29 where as in patients treated with k-wire was 50.70. proximal humerus fracture treated with CRIF with K-wire majority 65.2% were female and 34.8% were male whereas in patients treated with ORIF, PHILOS system 76.2% were female and 23.8% were male. in 44 patients with proximal humerus fracture, left side was affected in 19 patients from which 11 (47.8%) were treated with CRIF (k-wire) and 8 (38.1%) with ORIF (PHILOS). Whereas right side was affected in 25 patients out of which 12 (52.2%) were treated with CRIF with K-wire and 13 (61.9%) were treated with ORIF (PHILOS). proximal humerus fracture according to Neer’s classification. In total 44 patients, 27 patients were diagnosed as 3-part and 17 were 4-part. In 27 patients with 3-part proximal humerus fracture 15 (65.2%) were treated with CRIF (k-wire) and 12 patients treated with ORIF (PHILOS). In 17 patients with 4-part proximal humerus fracture 8(34.8%) patients were treated with CRIF (k-wire) and 9(42.9%) were treated with ORIF (PHILOS). out of 44 patients of proximal humerus fracture, 1 patient had 3rd Metatarsal fracture; 3 had clavicle fracture; 1 had intertrochanter fracture of femur; 6 had ribs fracture; 1 had right shoulder dislocation; 1 had scapula fracture and 31 patients did not have any associated injuries. Fracture was taken as united when there was no tenderness and unprotected full function of limb was possible. In group which was operated with ORIF (PHILOS) mean time of union was 11.10 weeks with S.D of 1.09 (In 10wks union happened in 10 patients; union took place in12wks in 10 patients; 13wks time was taken only by 1 patient.). whereas for group operated with CRIF(k-wire) mean time of union was 11.74 weeks with S.D of 1.01(in 10wks union took place in 5 patients; 12wks in 13 patients and 13wks in 4 patients and 1 case in our study which was treated with CRIF (k-wire) went for avascular necrosis). In all 44 patients, functional outcome was measured using constant-murley score. In patients treated with CRIF (k-wire) had excellent result in 7 patients (30.04%) whereas patients treated with ORIF (PHILOS) 10 (47.6%) had excellent results. Good result was found in 7 (30.4%) patients treated with CRIF (k-wire) and 8 patients (38.17) treated with ORIF (PHILOS).Fair result was found in 8 (34.8%) patients treated with CRIF (K-wire) and 3(14.3) patients treated with ORIF (PHILOS).The mean constant-murley score in patients treated with CRIF (k-wire) was 79.48 whereas patients treated with ORIF (PHILOS) had mean constant murley score of 85.29Poor result was seen in 1 patient who was treated with CRIF (K-wire) Post-surgical stiffness was most common complication encountered in our study with 17.4% patient being affected in the group who were treated with CRIF (K-wire) and 9.5% patients were affected who were treated with ORIF (PHILOS).Infection was second most common complication faced in our study, 3 (13.0%) patients were affected who were treated with CRIF (k-wire) and 2 (9.5%) patients in ORIF (PHILOS) group. Whereas only 1 case landed in avascular necrosis which was treated with CRIF (k-wire) and 1 patient who was treated with ORIF (PHILOS) developed impingement. Illustrated cases Case 1 Preoperative Postoperative 12-month follow-up Figure 23: range of motion of left shoulder joint post-surgery
Case 2 Preoperative Postoperative 12-month follow-up Figure 24: Range of motion of left shoulder joint post-surgery
Case 3 Preoperative Postoperative 12-month follow-up Figure 25: range of motion of left shoulder joint post-surgery
Case 4 Preoperative Postoperative 12-month follow-up Figure 26: range of motion of left shoulder joint post-surgery
DISCUSSION Proximal humerus fracture is the second most common fracture seen in upper limb fracture after distal radius fracture and most common fracture seen around shoulder joint. There have been many options available when comes to treatment of proximal humerus fractures such as:
Generally proximal humerus fractures are seen in all age groups; RTA (road traffic accident) or high velocity injury being most common cause in younger patients whereas trivial falls leading to proximal humerus fracture in elderly or osteoporotic bones. And treating these fractures in osteoporotic bones have become challenging to surgeons due to severely comminution, fracture pattern and cut through by screws. Zyto and colleagues reported mean constant score of 65apoints and no complications with conservative treatment compared with surgical approach, resulting in mean value of 60 points and with complications (AVN, infection).9 In Clifford’s (19980) series of 80 patients whose proximal humerus fracture were treated conservatively, results were excellent or satisfactory in 81%.3 Mangovern, kenner, and Nhoqfound good constant scores with surgery and relatively few complications, withmbetter functional scores for percutaneouskfixation.10,11,12 PHILOS2has disadvantages5of excessive soft tissue dissection3and blood loss, risk of injury to neurovascular structuresdand increased risk of avascular3necrosis of humeral head.13,14 But gooddlong-term results of proximal3humerus fracture managed6by PHILOS plate.15,16 Patients who0have 3-part2or 4-part5proximal humerus6fracture are more prone6for poor clinical results and2high failure rates especially8when the fixation has been5performed with conventional8non-locking plates.17,18 Locking plates provides#better stability than conventionalZplates that were used in2the past. 19-21. Many authors3have demonstrated that they5give better functional outcome and also avoid7complications.22-27. Hence, the fixed anglefplates enable a gain in the8torsional stiffness and8stability and may therefore promote0a superior outcome and less chance of complication#like cut-out of the screws and plates, non-union, avascular necrosis and fracture distal to plate.28 Maintenance of medial periosteal hinge and careful surgical dissection prevents damage to the posteromedial vessels at posteromedial neck of humerus, thus decreasing the incidence of AVN in follow‑ups.4 In a cadaveric study of MIPO, gardner and colleagues demonstrated preservation of humeral head arterial supply, which included the ascending branch of anterior circumflex vessel and an unnamed posterior branch, when the plate was placed in the “bare spot” on the proximal lateral region of the humerus.2 Dolfiet al..29 operated6Type II, Type III, and Type IV fractures of#proximal humerus using distallyZthreaded dynamic hip screw guide)pins, 2 mm K-wires, or 2.5 mm distally^threaded SchantzSpins. In their study, all patients withWNeer’s Type IV fractures#did not respond to fixation and three#had avascular necrosis (AVN), irrespectiveSof the type of pin#used. They concluded that stable fixationDwith early motion and subsequently good$results can be obtained using percutaneousSfixation in patients with Type II and Type IIICfractures; however, terminally3threaded pins must be used and smooth K‑wires0must be avoided. Percutaneous fixation0cannot be recommended in patientsmwith Type IV fractures. The present study was done at Aarupadai Veedu Medical College and Hospital, Puducherry during period from September 2017 to September 2019. In the study, a total of 44 casesandof fresh proximal humerus#fracture were treated by using#open reduction and internal@fixation with@PHILOS and percutaneous pinning with simple K-wire. These both the groups were evaluated preoperatively; details were collected in a preformed proforma; operated and were followed for at least 6 months on OPD basis. The data collected for both the groups was analysed and compared with each other, the result is compared with previous studies. In our study, female predominance was seen with total 31 patients and 13 male patients. Similarly in vijay,et al.7 study female predominance was seen with 28 female patients and 20 male. Whereas in study conducted by jaura, et al.2he reported 36 male patients and 24 female patients. In our study, 24 patients sustained fracture following road traffic accident and 20 patients had a simple self-fall. Whereas vijay, et al.4 reported in his study simple fall on ground as most common cause for fracture in 28 patients and road traffic accident in 16 patients. Mean age in our study is 50 years, this depicts the role of osteoporosis in proximal humerus fracture. Vijay, et al.4 reported similar in their study. Kralinger, et al.8 also reported the similar results. In our study right humerus was fractured more, 25 patients and 19 patients had left humerus involvement. Vijay,et al.4reported the similar results in their study. Fracture union1has never been a problemain proximal humeral fracture management as had been mentioned1in many studies6,9,10,11 due to cancellous nature of bone2unless anatomical neck or articular part2of humerus is involved, compromisingabone of its blood supply. In4our study, fractures in 43 patients united successfully. There were no cases of delayed union or nonunion in our study but 1 case went for avascular necrosis which was treated with K-wire. The average time for union (in weeks) was found to be 11(ranging 10–13 weeks) and was unaffected by the modality of treatment used. Vijay, et al.4reported the similar results in his study with average time for union of 10.34 weeks. In our study 23.80% of patients treated with PHILOS developed some post-operative complication and 34.78% of patients treated with K-wire. Jaura, et al.1 and vijay, et al.4reported the similar results in there study. In our study mean constant-murley score in patients4treated with PHILOS1was 85.29, while for patients treated5with K-wire was 79.48. jaura GS, et al.1, vijay, et al.4, hiren, et al.7, kralinger, et al.8 all reported the similar results in their respective studies. Early rehabilitation was paramount for obtaining good range of movements and prevention of stiffness.4 The recent evolutiondof locking1plate technology forwproximal humerusmfractures seems to havejrevolutionized the managementfof these fractures. However, there1have been very limited, prospective1studies investigatingmthe results ofvlocking plates for openqreduction and internalxfixation of proximal humeral4fractures. Most of these studies9have reported good functionalyoutcomes and recommended#the use of locking plates for proximal$humerus fractures especiallyein elderly patients with poor1bone quality.5 We, thusgbelieve, that a locking plate7device for proximalbhumerus fractures7gives a satisfactory0outcome in most of the patients6including those with old the age4and poor#bone density.
CONCLUSION
Our result demonstrated that the PHILOS system provides better and stable fracture fixation for early mobilization especially in Osteoporotic bone when compared with K-wire as treatment option for proximal humerus fracture type III and IV. Early results with PHILOS plate system were promising, and if plate is placed at optimal position and proper physiotherapy is given results can be better.
References
.
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Forensic Medicine (Print ISSN: 2579-0935) (Online ISSN: 2636-4735) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home