|
Table of Content - Volume 16 Issue 3 - December 2020
A retrospective study of outcome of supracondylar osteotomy in correcting cubitus varus deformity
Anwar Hamzath AK1, Dino M Joy2*
1Assistant Professor, Department of Orthopedics, DMWIMS, Naseera Nagar, Meppadi, Wayanad, Kerala, INDIA. Email: dinomjoy@hotmail.com
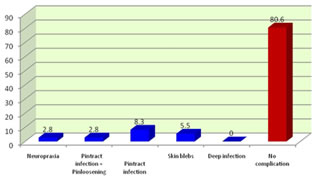
Abstract Background: Supracondylar fracture of humerus is one of the commonest fractures sustained by children. It is one of the difficult fractures to treat due complications like malunion, neurovascular injury, ischemic contracture. Much attention paid to prevention of malunion by anatomical reduction either by closed or open method. The present study evaluates a technique of correction of post-traumatic cubitus varus in children with a laterally based closing-wedge osteotomy of the distal humerus with medial displacement of distal fragment, through a lateral approach and fixation with percutaneous Kirschner wires. Methods: A Retrospective case series study in 42 children with cubitus varus deformity following supracondylar fracture of humerus, were treated by lateral closing wedge osteotomy with medial displacement of distal fragment and fixation with percutaneous K-wires. Out of these, 36 children who satisfied the inclusion and exclusion criteria, and were available for assessment of final outcome were included in this study. Results: 69.4% of the patients had excellent results, 16.7% patients had good results and 13.9% patients had poor results according to this criteria. The 5 poor results were due to residual varus deformity in one patient and due to increase in Lateral Prominence Index more than 2.5% in 4 patients. 91.7% of the patients were satisfied with the cosmetic outcome. Although a lateral bump was noticable in 4 (11.1%) patients postoperatively, only 2 of them were dissatisfied by its cosmesis. A noticable scar was present in 2 of the patients. The cosmetic dissatisfaction was due to the lateral bump in 2 patients and due to residual varus deformity in one patient. Complications were present in 19.4% of patients. This included a transient ulnar neuropraxia in one patient (2.8%), pin-tract infection in 3 patients (8.3%), pin-tract infection along with pin loosening and backout in one patient (2.8%) and skin blebs in two patients (5.5%). Conclusion: Corrective osteotomy done in childhood, takes advantage of the better chances of union and remodelling. Lateral closing wedge osteotomy and fixation with percutaneous K- wires with medial displacement of distal fragment is a relatively simple technique, avoids neurovascular injuries, gives excellent results without much problem of lateral prominence and good cosmetic appearance. Key words: Supracondylar fracture, cubitus varus, lateral closing wedge osteotomy, percutaneous K-wires.
INTRODUCTION Supracondylar fracture of humerus is one of the commonest fractures sustained by children. It is one of the difficult fractures to treat because of rather frequently occurring complications like, malunion, stiffness of elbow, nerve injury, vascular injury and volkman’ s ischeamic contracture .1-4The goal in treating these fractures is to re-establish the anatomy of distal humerus with least complications and with enough stability. Much attention has been paid to the problem of malunion of supracondylar fractures of humerus by obtaining, as anatomical a reduction as possible either by closed or open method. Cubitus varus (gunstock deformity) is the most common long-term complication of supracondylar fractures of the humerus in children. Reported in up to 58% of patients, its occurrence is higher in fractures originally managed conservatively.5,6Components of cubitus varus deformity are: a) medial angulation, b) medial rotation, c) extension of distal fragment with or without d) medial condyle epiphyseal injury leading to delayed growth of medial condyle and cubitus varus deformity.7 Although many causes have been proposed for varus malunion of supracondylar fractures , the biomechanical forces acting around the elbow which causes a medial tilt of the distal fracture fragment resulting in malunion has been most accepted.8 Cubitus varus does not often cause functional disability and surgery is mostly required for cosmetic reasons. It is better corrected during childhhood with different methods of corrective osteotomy. Many surgical techniques to correct a cubitus varus deformity are described in literature.10-12These include opening wedge, closing wedge and three-dimensional osteotomies and reverse ‘ V ’ osteotomy .13-19Lateral Closed wedge osteotomy is easy to perform but some authors have been critical of this method, alluding to problems with a lateral condylar prominence (lazy-S deformity) or an unsightly scar. 10,21,22The lateral closing-wedge osteotomy of French has been one of the most popular. By design, this method is primarily a uniplanar osteotomy. Although many authors reported successful correction of the varus alignment and correction of the rotary component,13,14,24-30the overall cosmetic appearance of the elbow has received little attention. To avoid the cosmetically unacceptable ‘ lazy S’ deformity of the elbow, various surgical techniques like Pentalateral osteotomy ,Modified step cut osteotomy and Lateral closed-wedge osteotomy with medial displacement of distal fragment have been introduced. 31But very few indian studies are available regarding medial displacement of distal fragment. The present study evaluates a technique of correction of post-traumatic cubitus varus in children with a laterally based closing-wedge osteotomy of the distal humerus with medial displacement of distal fragment, through a lateral approach and fixation with percutaneous Kirschner wires.
MATERIALS AND METHODS A Retrospective case series study in 42 children below the age of 15 years with cubitus varus deformity following supracondylar fracture of humerus, were treated by lateral closing wedge osteotomy with medial displacement of distal fragment and fixation with percutaneous K-wires. Out of these, 36 children who satisfied the inclusion and exclusion criteria, and were available for assesment of final outcome were included in this study. Patients who lost to follow up,had other modalities of treatment and older than 15 years are excluded.The pre-operative and post-operative data regarding each patient , including the details of follow up (which was already over) , was collected from their case records and from radiographs available with the patient and those in the data bank of radiology department. The data for subjective evaluation (questionnaire regarding cosmetic satisfaction) was collected from patients or their parents through direct interview during this study period. All patients were evaluated pre operatively by history, clinical examination, radiographs (AP, Lateral views of elbow) and with investigations and written informed consent. In clinical examination, carrying angle of both elbows measured with gonimeter in full extension. Measurements of Range of movements of both elbows, internal rotation of deformity and lateral prominence index is calculated. The purpose of the corrective osteotomy is to produce an elbow joint with a final appearance closely similar to that of the unaffected side. Before planning, radiographs of both upper extremities were taken in the same position with the elbow joints fully extended and the forearms fully supinated. The radiograph of the affected side was then traced. The traced forearm was superimposed on top of the reversed radiograph of the unaffected forearm, and the unaffected humerus is traced. The angle between the central axes of both the affected and the unaffected humerus, when the forearm remain superimposed, is the angle of correction. The angle of correction was copied onto a card in form of a triangle with two equal limbs and with several marks in both limbs at equal distances. The planned triangle was cut out and sterilized .
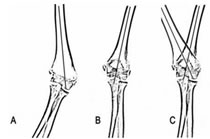
Figure 2: (A) The radiograph of the affected side is first traced. (B) The reversed radiograph of the unaffected forearm. (C) The affected side is superimposed over the unaffected side, and the angle between the central axes of both the affected and the unaffected side is the angle of correction.
Under general anaesthesia in supine position, under aseptic precautions, with application of tourniquet, lower humerus is exposed subperiosteally through a lateral approach because it gives adequate exposure and makes it easier to remove a lateral based wedge without much retraction of the lateral soft tissues. The planned lateral-based wedge is marked in the supracondylar area, taking into consideration, the amount of extension deformity at the malunited fracture site. Hohmann retractors are inserted subperiosteally to protect the medial, posterior and anterior structures. The wedge is then excised; the medial cortex is broken carefully by avoiding injury to ulnar nerve. The osteotomy is closed slowly and carefully. Distal fragment is medially displaced till the lateral borders are flush . During closure of the osteotomy, the posterior cortex of the distal fragment could be hinged over that of the proximal fragment to correct the internal rotation deformity if present. The osteotomy is fixed by two percutaneous Kirschner wires passed from the distal lateral to proximal medial cortex. The pins are bent to prevent migration, cut off outside skin and to allow removal in the outpatient clinic without anaesthesia. C-arm imaging is done to assess the correction and fixation. Wound is closed in layers and a well padded above -elbow slab is applied with elbow in 90 degrees of flexion. A careful observation for complications id done at regular intervals.Immediate post operative radiographs were taken to assess correction of deformity and security of fixation of osteotomy with appropriate antibiotic coverage. Follow - up Sutures were removed after two weeks in out patient clinic. Pop slab was kept for 5 -6 weeks (depending on the age of the patient). Kirschner wires were removed after 6 weeks postoperatively depending on x-ray taken to assess union , followed by active range of motion (ROM) exercises. At each follow-up visit, the children were assessed for range of motion, carrying angle, and the presence of any bony prominence over the lateral condylar region or an unsightly scar at the site of surgery and the data was entered in case records. Radiographs were performed in the immediate postoperative period, at 5-6 weeks (on removal of POP), when the patient regained full range of motion and at final follow up. All these data were obtained from the case records and radiographs were collected from the patient or from the radiology data bank, and were evaluated during the present study. METHOD OF EVALUATIONFollow up of the patients ranged from 1 year to 10 years. Assessment include the subjective evaluation of the lateral condylar prominence, cosmesis and scar ; and objective evaluation. These were used as strict criteria to categorize the results. Radiograpic assessment included the measurment of the carrying angle and LCPI. The operative time, blood loss, neurological complications, infection, wound healing and pin tract condition were recorded. The results of the osteotomy are categorized as excellent, good and poor as in Table-2
Note: The lowest score from the three parametres was taken as the final result. STATISTICAL ANALYSISThis retrospective study included 36 children. Sample size was justified using the formula: N= (Zα/2+Z β)2 ×2(SD)2 d2 Where SD is the Standard deviation obtained from previous similar study , Kumar in year 2014 = 2.4 d= accuracy of the estimate=2 Zα/2 = Normal deviate for two tailed hypothesis = 1.96 Z β = 1.64 (Type II Error) N = Sample size Substituting the above formula we get a sample size of 37. Descriptive statistical analysis was carried out in the present study. Results on continuous measurements are presented on Mean value (Min-Max) and results oncategorical measurements are presented in Number%. Variables will be correlatedwherever relevant. Using statistical software SPSS 20.0 data and Microsoft word and excel generated tables and figures
RESULTS In this study 36 children with cubitus varus who were treated by supracondylar lateral closing wedge osteotomy with medial displacement of distal fragment and fixation with percutaneous K-wires were evaluated objectively and subjectively. DESCRIPTIVE STATISTICS OF THE PATIENTS
Table 1
Table 2: Re# - Refracture, L/C# - Lateral condyle fracture
Table 3:
PRE-OPERATIVE CLINICAL AND RADIOLOGICAL ASSESMENT Table 4
< 0.001 ,which means the change was highly significant statistically.
Table 5:
SD- standard deviation (p< 0.05- Significant*, p < 0.001 - Highly significant**)
Association between carrying angle of unaffected limb and post operative carrying angle of affected limb: The mean carrying angle of normal limb was 7.58 degree and that of affected limb (post-operative) was 5.75 degree and the change was statistically significant (P-value <0.001).
Table 6:
(p< 0.05- Significant*, p < 0.001 - Highly significant**)
Table 7:
(p< 0.05- Significant*, p < 0.001 - Highly significant**)
Table 8:
(p< 0.05 - Significant*, p < 0.001 - Highly significant**)
Table 9:
(p< 0.05- Significant*, p < 0.001 - Highly significant**)
69.4% of the patients had excellent results , 16.7% patients had good results and 13.9% patients had poor results according to this criteria. The 5 poor results were due to residual varus deformity in one patient and due to increase in Lateral Prominence Index more than 2.5% in 4 patients. Table 10:
Table 11:
Figure 1: Types of complications
DISCUSSION Cubitus varus is one of the most common complications of supracondylar fractures of the humerus in children treated with nonoperative management . Its reported incidence varies from 4% to 58%.5,6It may result from inadequate reduction, from loss of reduction with consequent malunion, or rarely from disturbance of growth at the lower end of the humerus. Most authors consider the deformity to result from inadequate reduction that leaves a residual rotatory deformity that can collapse into a medial tilt resulting therefore in a varus deformity .25,36,54Or it could be due to the mechanical forces acting across the fractures , leading on to varus tilt.Cubitus varus does not often cause functional disability and surgery is often required for cosmetic reasons. It is better corrected during childhood. Various osteotomies for correction of cubitus varus deformity like Medial open wedge osteotomy, Lateral closing wedge osteotomy of French, Modified french technique, Dome osteotomy, 3-dimensional osteotomy etc. Lateral closing wedge osteotomy is the easiest, safest and an inherently stable method of correction. The type of fixation of osteotomy is a concern to achieve good result. Roach etal.,55believed that unstable, non-rigid fixation led to slip of the fragments and loss of correction. The fixation with percutaneous K-wires frequently led to loosening of the fixation with recurrence of deformity, pin tract infection ,skin sloughing, nerve palsy and rarely brachial artery aneurysm.30,20 Most investigators would agree that 4 factors can ultimately determine the outcome of supracondylar osteotomy of humerus : 1)adequate correction of carrying angle, 2)stability of fixation of osteotomy, 3) avoiding a lateral bump and 4)avoiding post operative complications which will compromise the results. In this study, results of 36 patients with cubitus varus deformity treated by lateral closing wedge osteotomy with medial displacement of distal fragment and fixation with lateral percutaneous K-wires were evaluated. The analysis of results are made in terms of age ,side, gender distribution, associated injuries and final clinical, radiological and cosmetic outcome. Descriptive patient data : The mean age of the patients in this study was 9 ± 3.43 years. Age of the patients ranged from 5 - 15 years according to the inclusion criteria. This is comparable with the study by Kumar D46in 2014 , in which the age of patients ranged from 5 to 15 years with a mean age of 9.07 ± 3.07 years. Cubitus varus following supracondylar fractures is usually a static deformity. Hence they can be corrected as soon as bone remodelling after index fracture is completed and reasonable ROM achieved. There is no need to wait for skeletal maturity. Doing this surgery in childhood, also takes advantage of the better chances of union in this age group. Wong etal(1990) have opined that lack of remodelling in older age groups results in the persistance of lateral prominence.22 Majority of the children in the present study were boys ( 63.9%). Most investigators have found similar male predominance. Wong22reported 23 male and 4 female patients. 5 (13.9%) out of the 36 children, with cubitus varus in this study were initially managed surgically by closed reduction and percutaneous pinning for supracondylar fracture. Nacht JL56reported mean carrying angle loss of 5.8 degree in 20 patients after closed reduction and percutaneous K-wire fixation for supracondylar humerus fracture. He observed cubitus varus in 3 out of 38 children in his study.That means cubitus varus can occur not only in supracondylar fractures treated conservatively, but also with surgically managed cases if proper reduction is not achieved. Four patients with cubitus varus in this study had history of Lateral condyle fracture of the same elbow after the initial injury (supracondylar fracture). Davids “Post traumatic cubitus varus may predispose a child to subsequent lateral condylar fracture and that this deformity should be viewed as more than just a cosmetic problem”.41 Post-operative carrying angle: The main deformity in cubitus varus is the reversal of carrying angle of the elbow. The purpose of surgery is to correct this. In our study, the mean post-operative carrying angle was +5.75 degree with an average difference of 1.83 degree from that of the normal side. We were able to achieve good correction in majority of our patients. Only one patient had residual varus at follow up and was advised resurgery. That patient had pintract infection, pin loosening and back out necessitating early K-wire removal. So the cause for residual varus was post-operative loss of reduction due to infection and pin loosening. Most investigators had achieved good correction of varus deformity with lateral closing wedge osteotomy. Wacl EL44in 2007 reported the average post operative carrying angle as 5 degree with a difference of 1.6 degree from opposite side. Voss31in 1994 studied lateral closing wedge osteotomy and observed that in 97% of the patients, the deformity was corrected to within 5 degrees of the contralateral elbow. Post-operative Range Of Motion: In our patients, active range of motion exercises were started after K-wire removal at 5-6 weeks post operatively. Almost all patients achieved the pre-operative range of movements with the mean difference in total ROM being 0.5 degree between pre-operative (136 degree) and post-operative (136.5 degree) at 1 year follow up. Supracondylar osteotomy for cubitus varus is mainly a cosmetic surgery and no functional change - change in ROM- is usually expected, unless there is a myositis or excess callus formation. Wael EL44also observed little or no differences in the range of motion (ROM) of the elbow except in one child who had slight limitation in elbow flexion of about 6o.
Lateral Prominence Index (LPI): A prominent lateral condyle after correction of angulation was reported as a main complication of lateral closing wedge osteotomy (Wong22). In this study the distal fragment was displaced medially after full thickness osteotomy of distal humerus, to eradicate this problem. Although the mean LPI decreased from 0.415 to -1.485 post-operatively, the results were not consistant in all patients. 9 of the 36 patients (25%) had an increase in LPI post operatively , and 4 of them had a noticable lateral bump at follow up. But out of these 9 children only 2 were dissatisfied with cosmesis ; which means that an increase in LPI does not always affect the cosmetic outcome. Kumar D46studied Dome osteotomy and observed a mean change of -1.29±1.68% in LPI and the change was significant (p=0.010).They advocated dome osteotomy as a better method to address the problem of lateral prominence, although it is technically more demanding. Our results were better when compared with the results of Wong 22,who reported that 14 out of 27 patients were noted to have a significant lateral prominene. So medial displacement of the distal fragment can be used as a method to decrease the lateral prominence although the intact periostel hinge on the medial side can make this difficult and excess callus formation on the lateral side can also contribute to a lateral bump. Objective outcome: As per the criteria described by oppenheim et al... 3069.4% of the patients had excellent results , 16.7% patients had good results and 13.9% patients had poor results. The poor results were due to residual varus deformity in one patient and due to increase in Lateral Prominence Index more than 2.5% in 4 patients. Srivastava AK57studied lateral closed wedge osteotomy and reported that 85% patients showed excellent results and 15% good results while none showed fair or poor results in the follow up. Wael EL44reported 91.7% excellent results and 8.3% with good results according to Oppenheim 3 0criteria . But the sample size was very less. A meta-analytical summary estimate for overall rate of good to excellent results with 4 different types of osteotomies was 87.8% in the meta analysis done by Solfelt DA47 Cosmetic outcome:91.7% of the patients were satisfied with the cosmetic outcome. This is comparable with the results of Srivastava AK57in which 95% patients were satisfied with cosmesis. Post operative complications like pin tract infection, skin blebs or transient neuropraxia did not affect the final cosmetic outcome. The reason for cosmetic dissatisfaction was the lateral prominence in two patients. Complications: The overall rate of complications was 19.4% and it was high when compared with the meta analysis by Solfelt DA47- 14.5% which included 4 types of osteotomies. Pin tract infection was the main complication which accounted for 11.11%. Dome osteotomy by Kumar46also reported pin tract infection in 20% cases. The results were better when compared with the complication rate of Oppenheim30- 24%- which included 5 nerve palsies, 3 infections and 12 patients with residual varus out of the 45 patients who underwent lateral closing wedge osteotomy. These results make it obvious that pin tract infection and pin loosening are a matter of concern, when percutaneous K-wires are used for fixation of osteotomy. CONCLUSIONCorrective osteotomy done in childhood, takes advantage of the better chances of union and remodelling. Lateral closing wedge osteotomy and fixation with percutaneous K- wires with medial displacement of distal fragment is a relatively simple technique, avoids neurovascular injuries , gives excellent results without much problem of lateral prominence and good cosmetic appearance.
REFERENCES
.
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Forensic Medicine (Print ISSN: 2579-0935) (Online ISSN: 2636-4735) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home