|
Table of Content - Volume 17 Issue 3 - March 2021
Short term study of novel technique of ultrasonography guided hydrodistension for acute adhesive capsulitis
Shripad Joshi1, Kaiwan Randeria2*, Abhishek Kulkarni3
1Associate Professor, 2Resident, Department of Orthopaedics, MGM College & Hospital, Aurangabad, INDIA. Email: shripadjoshi2007@gmail.com
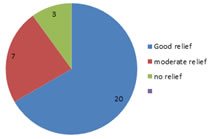
Abstract Background: Adhesive shoulder capsulitis, or arthrofibrosis, describes a pathological process in which the body forms excessive scar tissue or adhesions across the glenohumeral joint, leading to stiffness, pain and dysfunction. Painful stiffness of the shoulder can adversely affect activities of daily living and consequently impair quality of life. This study was taken up to establish the efficiency of our novel method of hydrodistension wherein we used a mixture of bupivacaine, triamcinolone acetate and lignocaine. 30 patients were taken up for the study in which we observed that 60-70% of the patients had good relief [quickDash score improved by 60-75 points] 10-20% of the subjects had moderate relief [quickDash score improved by 40-50 points] 10% of the subjects had no relief at all. The non responders were also investigated for the poor outcome. We concurred that hydrodistension is an efficient and short timed procedure having significant improvement in functional outcome of patients. Also, our novel mixture was found to be superior in comparison to mixtures used in studies done worldwide. Keywords: hydrodistension, acute adhesive capsulitis.
INTRODUCTION Adhesive shoulder capsulitis, or arthrofibrosis, is a pathological process during which excessive scar tissue or adhesions are formed across the glenohumeral joint, leading to stiffness, pain and inability to carry out daily activities. Painful stiffness of the shoulder can adversely affect activities of daily living and consequently impair quality of life. ‘Scapulohumeral Periarthritis’ or frozen shoulder describes a painful shoulder syndrome that is distinct from arthritis with general radiographic preservation of the joint.1 According to the research so far, FS can be divided into three phases: freezing (insidious onset of shoulder pain with progressive loss of motion), frozen (gradual subsidence of pain, plateauing of stiffness with equal active and passive ROM), and thawing (gradual improvement of motion and resolution of symptoms).2. The prevalence rate of FS is 2%–5%, and it occurs more commonly in women.3. The most common association is diabetes mellitus and the incidence is reported to be 10%–36%.9) Thyroid disease, adrenal disease, cardiopulmonary disease, and hyperlipidemia are also known to be related.4 Adhesive capsulitis can be primary or secondary. Primary (or idiopathic) adhesive capsulitis can occur spontaneously without any specific trauma or inciting event. Secondary adhesive capsulitis is often observed after periarticular fracture dislocation of the glenohumeral joint or other severe articular trauma. It can also be a severe complication after open or arthroscopic shoulder surgery, including rotator cuff repair and shoulder arthroplasty. The incidence of adhesive capsulitis in the general population is approximately 3% to 5% but as high as 20% in patients with diabetes. Idiopathic adhesive capsulitis often involves the nondominant extremity, although bilateral involvement has been reported in up to 40% to 50% of cases. Adhesive capsulitis is often regarded as a self-limiting disease that resolves between 1 and 3 years. However, various studies have shown that between 20% and 50% of patients may go on to develop long-lasting symptoms. In this patient population, both non-operative and operative interventions are needed to ensure acceptable functional outcomes. Patients had been divided into acute and chronic adhesive capsulitis.
AIMS To evaluate the functional outcome of hydrodistension in patients suffering from adhesive capsulitis
OBJECTIVES To check the age wise incidence of adhesive capsulitis Efficacy of hydrodistension as a treatment modality To establish the efficacy of novel mixture of triamcinolone, lignocaine and bupivacaine
METHODS AND MATERIALS A study was conducted among the patients who visited MGM AURANGABAD opd with complaints of shoulder pain and restriction in movements around the shoulder joint.These patients’ were given a standardized questionnaire which ruled out any infective, traumatic cause and evaluated any underlying co morbidities. The inclusion criteria was patients having painful restriction of movements around the shoulder joint and with clinical diagnosis of adhesive capsulitis . patients were divided into acute and chronic adhesive capsulitis on the basis of symptomatology i.e acute adhesive capsulitis is condition in which patients has rest pain with disturbed night sleep with 24X7, chronic adhesive capsulitis is condition in which patients has restricted movements with pain during movements of shoulder The most common patients in our study where acute adhesive capsulitis ,followed by chronic adhesive capsulitis type presenting within a span of 6months and not relieved by conservative treatment. Exclusion criteria comprised of patients on anticoagulation, having coagulopathy, systemic sepsis, allergies to steroid or local anesthetic and patients with adhesive capsulitis secondary to trauma. Over a period of 6 months, 30 patients were included in the study as subjects. These patients underwent a high frequency USG to confirm the diagnosis of adhesive capsulitis. The patients were evaluated using a QuickDash self assessed questionnaire just prior to the hydrodistension procedure. After the procedure, the patient was given a single day dosing of IV analgesics and discharged on oral analgesics for 5 days. The patients were then evaluated post operatively with followup on 14 days, 1.5 months and 3 months. On each followup, the QuickDash score was reassessed and the symptomatic improvement in shoulder ROM and activities of daily living were assessed. Procedure For the procedure, a USG guided steroid injection was injected into the shoulder capsule by posterior approach. The injection comprised of 2ml of Triamcinolone Acetate, 4ml of Injection Lignocaine and 6ml of Injection Bupivacaine and 30 ml of sterile Normal Saline. (4) METHOD The patient first undergoes a diagnostic USG to rule out any rotator cuff tear. If there is only isolated adhesive capsulitis then only shall the patient be included in the study. PROCEDURE: The patient is taken in lateral decubitus on the table Primary painting and draping is done, leaving the shoulder joint exposed and posteriorly the border of acromion. We locate the posterior glenohumeral articulation with the probe around 2cm below the posterolateral area of acromion in horizontal position. The position of the needle is confirmed on USG. Also back flow of fluid from the needle hub confirms that the needle is in the joint. Out of plane technique is performed using a high frequency USG probe. Then we instill 30ml of Normal Saline into the joint and distend the capsule.
Figure 1 Figure 2 Figure 3 Figure 4 Figure 5
Following which, a solution of 2ml Triamcinolone acetate, 6ml Bupivacaine and 4ml Lignocaine is injected into the joint.(4) The joint ROM is assessed immediately after this technique Triamcinolone acts by anti-inflammatory properties thus relieving capsular inflammation, Lignocaine acts as a local anaesthetic whereas Bupivacaine is a long acting anaesthetic. This combined formulation had a supraadded effect in overall relief of the capsular inflammation. The volume used-42 ml was derived from the fact that a normal shoulder joint can accommodate upto 15ml of fluid. Thus this formulation provided adequate distension. Usually, a 26G spinal needle is used for the procedure which was found to be adequate but in obese patients, a 18G spinal needle had to be used due to increased fat around the area.
RESULTS We conducted a study on 30 patients amongst which 19 patients were above the age of 50 with the mean age being 55 years showing the the incidence of adhesive capsulitis increases with the age. From the 30 patients, 20 of them were females showing a female preponderance as seen with other studies. In the aforementioned study conducted,we decided to measure the outcome in terms of improvement in the quickdash scores. It was observed that :
We tried to investigate the reason of having a poor relief post procedure and the cause was that the non responders usually had a thickened capsule due to which adequate distension was unable to be achieved and thence the poor outcome.
Figure 1: Comparing outcome in terms of improvement in QuickDash scores.
DISCUSSION This procedure is preferred because it provides immediate relief for acute frozen shoulder patients. During this procedure, a 20ml leur lock syringe is used as it provides adequate saline pressure required for hydrodistension. For the procedure, the needle was inserted from the posterior aspect and the flow was injected anteriorly thus allowing the full pressure force to directly face the capsule thus allowing proper distension Our unique formulation works extremely well because Lignocaine provides immediate short term anaesthetic relief, Bupivacaine provides a longer acting anaesthetic relief whereas Triamcinolone acts by suppressing inflammation; thus the patient compliance is increased, there is improved cooperation with physical therapists too as the formulation provides a long term relief and this helps in faster recuperation. In our study, we also injected a mixture of 2ml Triamcinolone acetate with 2ml Lignocaine into the bicipital sheath and this showed better results than the other studies. In one randomized clinical trial of 40 patients performed by Lorbach6 et al. patients with idiopathic FS were treated with an oral corticosteroid treatment regimen (20 patients) or intra-articular injection of corticosteroid (20 patients). In the patients treated with the oral regimen, significant improvements were found for pain and functional outcomes at the 4-week follow-up. However, the patients treated with an intra-articular injection showed superior results in objective shoulder scores, ROM, and patient satisfaction compared with the oral steroid group.7 Buchbinder et al.8 reported the results of oral prednisolone for the treatment of FS in a randomized, double-blinded, placebo-controlled study and found significant improvement in the study group at 3 weeks. As described in the previous studies, oral steroid treatment seems to provide early benefit both in terms of pain relief and functional outcomes; however, long-term benefit has not yet been established Following this procedure, a vigorous physiotherapy programme was done with the help of physical therapists for a span of one month. This also helped in maintaining the long term efficacy of the procedure. Good results have been reported with physiotherapy itself or in comparison with other conservative management.9,10,11 Russell et al. conducted a blinded, randomized, controlled study comparing the efficacy of three treatment regimens: exercise class plus home exercises, individual multimodal physiotherapy plus home exercises, and home exercises alone. They found the exercise class group showed significant improvement in Oxford and Constant scores. The improvement in ROM was significantly greater in the physiotherapy group than the exercise alone groups. Similarly, steroid injection used in combination with physiotherapy resulted in better outcomes compared to injection alone.12,13,14 In the non responders, a repeat procedure was done in an interval of 3 weeks. This repeat procedure showed improvement in around 80% of the non responders. The reason for this was looked into and we found that most of the non responders were patients presenting 3 weeks after the capsulitis onset. This lead to a well thickened capsule which was unable to be ruptured during the procedure and hence a repeat procedure, when undertaken with higher saline pressure successfully ruptured the capsule providing relief. Hypopigmentation was also noted at the needle injection site. This was due to extravasation of the mixture subcutaneously In diabetic patients who were maintaining their blood sugar levels on oral hypoglycemics, it was noted that the blood sugar levels were raised for the first 14 days post procedure despite of their usual dose of hypoglycemic medication; however, these sugar levels came back to normal within 3 weeks of the procedure. Hence it is advisable to keep the procedure in conjunction with regular checkup with a diabetologist pre and post procedure. It was noticed that the patient had good range of motion intraoperatively once the capsule was distended but on post operative day 2 onwards there was a 30 percent reduction in the range of motion as compared to that achieved intraoperatively; however the patients had around 80% increase in range of motion (as compared to pre operative ROM) by 3 weeks post procedure.
CONCLUSION From this study, we can conclude that the procedure of hydrodistension shows significant improvement in adhesive capsulitis patients, our novel mixture of lignocaine, triamcinolone and bupivacaine works extremely well and is a good modality to use in conjunction with post procedure physiotherapy.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home