|
Table of Content - Volume 18 Issue 2 - May 2021
Prospective study of functional outcome of proximal humerus fracture managed by various modalities
Nishad Situt1*, Shashikant Kukale2
1Junior Resident, 2Associate Professor, Department of Orthopaedics, Vilasrao Deshmukh Government Institute of Medical Science, Latur, Maharashtra, INDIA. Email: situt.nishad@gmail.com
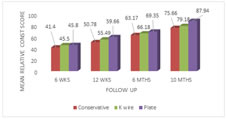
Abstract Background: The proximal humeral fractures are one of the common fractures and treatment of this fractures still remains a controversy. Present study is confined to analyse fracture of the proximal humerus that were treated with Consrvative method and Operative method. Aim: To study the functional outcome of proximal humerus factures managed with various modalities. Material and Methods: A total of 68 patients both male and female having proximal humerus fracture with or without associated injuries that were included. They were treated with Immobilization for one or two weeks, followed by physiotherapy Closed Reduction and Per-cutaneous Pinning(CRPP), Open Reduction Internal Fixation(ORIF) with locking plate. Patients were followed up for 10 months postoperatively. Result: The mean Relative Constant Murley Score On 10 months follow up 87.94 was the mean Relative Constant Murley Score for patients treated with plate, and for k wiring and conservative, it was 79.18 and 75.66 respectively. Conclusion: Functional outcome was best with ORIF with plate as compared to CRIF with k wire and conservative treatment, as per Constant Murley Score, however LCP fixation is associated with impingement due to improper surgical technique, needs more expertise as compared to K wiring and conservative treatment.
INTRODUCTION The proximal humeral fractures(PHF) are the most common fractures in elderly people. Fracture of proximal humerus, representing 5 % of all extremity fractures, is a common fracture in everyday clinical life.1, 2 3/4th of fractures occur in older individuals with an occurrence more often in women than in men. In the elderly population, most of these fractures are related to osteoporosis while injury in younger people is likely to be the consequence of high energy trauma.4 Because of increase in incidence of high velocity trauma, the fracture pattern in proximal humerus fractures are becoming complicated. Treatment of this fracture is guided by bone quality, fracture displacement, angulation, degree of comminution; patient factors such as age and baseline activity level, hand dominance as well as surgical experience of treating surgeon. Ultimate goal should be minimal pain and maximal range of motion. The superior management of displaced PHF in the elderly still remains a controversy.5Of all PHF, about 85–90% are considered suitable for non-operative treatment: immobilization for one or two weeks, followed by physiotherapy6. In these cases, fractures usually only show minor displacement, as well as little angulations, healing uneventfully in the future. A review of published results suggests that there is no universally accepted form of treatment.4 Surgical option include Closed Reduction and Per-cutaneous Pinning (CRPP), Open Reduction Internal Fixation (ORIF) with locking plate (LCP) and Hemiarthroplasty. Neer recommended open reduction and internal fixation for displaced two-part and three-part fractures2. One of the serious problems associated with proximal humeral fixation is the potential damage to the blood supply of the humeral head.7 Standard plates require extensive dissection potentially disrupting major vessels supplying to the humeral head and shaft.12 Recent trends shifted from open reduction and massive internal fixation towards closed reduction and minimal fixation, which is a less invasive method associated with less damage to the soft tissue and a low rate of avascular necrosis of humeral head.9Present study is confined to analyse fracture of the proximal humerus that were treated with Immobilization for one or two weeks, followed by physiotherapy; CRPP, ORIF with LCP and their clinical and functional outcome.
MATERIAL AND METHODOLOGY It is a Prospective Observational Study conducted in tertiary care centre during December 2017 to September 2019, on 68 patients with closed proximal humerus fractue satisfying inclusion and exclusion criteria were included into the study after obtaining their consent. Inclusion Criteria:
Exclusion Criteria:
Preoperative assessment: The patients with PHF were admitted, detailed history was elicited from patient and/or attendants to reveal the mechanism of injury, severity of trauma and demographic data. Then patients were assessed clinically to rule out other significant injuries like chest, abdominal or head injury. Local examinations were done for evaluation of swelling and ecchymosis around shoulder, tenderness around proximal arm and palpable crepitus, neurological examination to rule out axillary nerve injury (regimental badge sign). The clinical diagnosis was confirmed radiologically by taking x-ray of shoulder with arm, in antero-posterior view and axillary view, and CT shoulder with 3D reconstruction in selected cases. Fractures were classified according to Neer’s Classification2. Affected shoulder was immobilized in universal shoulder immobilizer or POP U slab. Conservative treatment: It was given for following indications- 1) elderly patients with osteoporosis 2)severe co-morbid conditions 3)minimally displaced fractures 4)Impacted Valgus fractures 5)one part fracture. Affected arm was immobilized in Shoulder Immobilizer or U-POP Slab (Fig1) for 4 - 6 weeks. During which active range of motion exercises of the wrist, and hand was encouraged. Shoulder passive range of motion was started after 2 -3 weeks and after 6 weeks, active range of motion was started. Operative treatment: Choice of anaesthesia was decided by anaesthetists and the same informed to patient. CRPP: Manipulation of the proximal segment was performed with the use of percutaneously placed 2.5-mm K-wires, through anterior reduction portal just lateral to the biceps tendon. Once adequate reduction had been achieved, fixed with 2.5 mm terminally threaded 3 K-wires, one from anterior to posterior and two through the tuberosities into the medial proximal humeral cortex ORIF With LCP: Proximal humerus exposed with delto-pectoral approach19(Fig2) . The medial aspect of the surgical or anatomic neck was reduced and the tuberosities around the humeral head were reduced. Temporary fixation achieved with 2 – 2.7 mm K –wire(fig3). The plate position was also selected to avoid subacromial impingement. Screw placement was performed by drilling through the near cortex only. Two locking screws were placed into the proximal segment, second shaft screw was placed. Subsequently, minimum of five or six screws were routinely placed into the proximal segment(fig4).
Figure 1: POP ‘U’ Slab Figure 2: Exposure of fracture site Figure 3: Temporary fixation Figure 4:Final plate fixation AP View Postoperative rehabilitation: Patients were immobilized for 3 to 4 weeks in a sling, while active range-of motion exercises of the elbow, wrist, and hand were encouraged. Passive range of motion was started after 4 weeks and after 6 weeks active range of motion was started. Functional Outcome Evaluation: Patients were followed at 6 week, 12 week, 6 months, 10 months (minimum 10 months follow up) for clinical and radiological evaluation; including functional outcome evaluation with Constant-Murley Scoring System(CMSS).16
RESULTS Of 68 patients treated,10(14.71%) in age group of 18 to 30 yr, 26(38.24%) in 31 to 50 age group, 22(32.35%) in 51 to 70 yr age group, 10(14.71%) of > 70 yr age. Mean age was 50.53±16.96 years. 44 patients were male (64.7%) and 24 were female (35.3%). Fracture was found to be more on Right side (50 of 68; 73.53%), as compared to Left side (18 of 68; 26.47%). The most common mode of injury observed was road traffic accident (RTA) accounted for 39 out of 68(57.53%), self fall in 28 patients (41.17%) and sizure disorder in 1 patient. The incidence of 2 Part and 3 Part fracture pattern as per Neer’s Classification were found to have equal incidence 28 out of 68 (41.2%) (graph1).
Graph 1: Distribution of fracture pattern; Graph 2: Distribution of fracture type VS age group
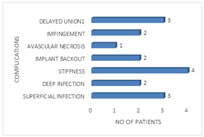
3 and 4 Part fractures were seen most commonly in elderly population (>50 years) accounting for 24 of 68 (36 %)(graph2). Associated injuries were seen in 7(10.29%) patients, 3 patients sustained clavicle fracture (4.4%), 2 patients with distal end radius fracture (2.9%), 1 with radius and ulna fracture (1.5%) and 1 sustained chest injury (1.5%). In the study 22 out of 68 patients (32.4 %) were managed conservatively, CRPP in 22 out of 68 patients (32.4 %) and ORIF with LCP was performed in 24 out of 68 patients (35.3 %)(Table-1). Stiffness is the most common conplication seen in 4 patients (5.9%) was associated with deep infection in 2 patients from k wire fixation group and seen in 2 patients from conservative group(graph-3).
TABLE 1: DISTRIBUTION OF TREATMENT MODALITY USED VS FRACTURE PATTERN
Graph 3: Distribution of complications The range of movement achieved by patients during follow up us given in table2, 3, 4, 5. The mean Relative-CMSS at 6 week follow up was maximum for patients treated with ORIF with LCP which was 45.8 . Mean Relative-CMSS at 12 week follow up was 59.66 for patients treated with ORIF with LCP which is maximum. At 6 month follow up mean Relative-CMSS of patients treated with ORIF with LCP was 69.35 which is maximum. On 10 months follow up 87.94 was the mean Relative-CMSS for patients treated with ORIF with LCP. For CRPP and conservative, it was 79.18 and 75.66 respectively(Graph 4).
TABLE 2: MEAN FEXION OF VARIOUS MODALITIES ON FOLLOW UP
TABLE 3: MEAN ABDUCTION OF VARIOUS MODALITIES ON FOLLOW UP
TABLE 4: MEAN INTERNAL ROTATION OF VARIOUS MODALITIES ON FOLLOW UP
TABLE 5: MEAN EXTERNAL ROTATION OF VARIOUS MODALITIES ON FOLLOW UP
Graph 4: Mean relative constant murley score at follow UPS
DISCUSSION PHF account for 5% of all extremity fractures1,2. The commonest cause in older population being osteoporosis and younger being high velocity injuries. 80-85% of these fractures are amenable to conservative treatment, remaining 15-20% are significantly displaced and require some type of internal fixation. The treatment modalities used in this study are conservative, CRPP and ORIF with LCP. The basis for using the said modality also depended on various factors like age of the patient, type of injury, type of fracture and compliance of the patient. 2 Part and 3 Part fracture pattern as per Neer’s Classification were found to have equal incidence, 28 out of 68(41.2%) of each type, may be due to small sample size. 4 Part fracture was found to be least common accounting for 12 out of 68(17.6 %). In studies done by R Shahid et al.14, 28 in a series of 50 patients studied 11(22%) were 2-part fractures, 21(42%) were 3-part fractures and 18(36%) were 4-part fractures. In a study by MA Fazal et al.13, 32 out of 27 cases 13(48%) were 2-part fractures, 12(44.5%) were 3-part fractures and 2(7.5%) were 4-part fractures indicating that the incidence of type of fracture is nearly consistent with the studies in literature. The most common mode of injury was RTA, 39 out of 68(57.53%). Self fall in 28 out of 68(41.17%) of total patients and 1 patient had a history of seizure disorder. High energy trauma was more common in males 33 out of 68(48.5%) as compared to females 6 out of 68. Whereas self-fall is the most common mode of injury among females accounting for 18 out of 68(26.47%) patients. The incidence of fracture due to road traffic accident is more in the young age population (18–50 years) accounting for 25 out of 68(36.76%). In a study conducted by Sudkamp et al.16, most common mode of trauma was low energy trauma in 162(87%), high energy trauma in 25(13%). In study conducted by F Muncibì17, accidental falls were seen in 37 patients, motorcycle accidents in 2 and sports-related injuries in 2 patients. In a study conducted by Ge et al.18 on 189 2-part or 3-part fractures, mean flexion at 6 month was 148.8o for patients treated with ORIF with plate and 140.7o with conservative treatment, whereas mean flexion at 10 months was 153.45o for patients treated with ORIF with plate and 152.3o with conservative treatment. Mean external rotation at 6 month was 41.4o for patients treated with ORIF with plate and 37.2 o with conservative treatment, whereas external rotation at 10 months was 44.7o for patients treated with ORIF with plate and 40.4o with conservative treatment. The comparisson of movements at 10 to 12 mth follow up in patients treated with ORIF with LCP of our study with Gerber et al.11 has been given in table-6
TABLE 6: Comparisson of movements at 10 to 12 mth follow up in patients treated with ORIF with LCP
Treatment related complications in present study were seen in 15 patients out of 68 patients accounting for 22.05%. In the study conducted by Sudkanp et al.16, 62 complications were observed out of 155 patients, out of which 25 (40%) were due to selection of incorrect surgical technique, with most common complication being intra operative screw perforation seen in 21 out of 155 (14%). R Shahid et al.14 conducted prospective study of 41 patients, 1 showing delayed union, avascular necrosis in 1 patient (1.4%) from LCP fixation group. The mean Relative-CMSS in present study at 6 week follow up was maximum for patients treated with plating which was 45.8 as compared with conservative and k wiring which was 41.4 and 45.5. Mean-CMSS at 12 week follow up was 59.66 for patients treated with plating which is maximum followed by k wiring which was 55.49 and for conservative was 50.78. Comparison of Relative-CMSS of our study has been compared with various other studies in table-2.
TABLE 2: FUNCTIONAL OUTCOME BASED ON CONSTANT MURLEY SCORE
CONCLUSION Functional outcome was best with ORIF with LCP as compared to CRPP and conservative treatment, as per Constant Murley Score. As Locked Compression Plate provides stable anatomical reduction, it is preferred in unstable 3-part and 4-part fractures as well as osteoporotic bones. However ORIF with LCP is associated with impingement due to improper surgical technique, needs more expertise as compared to CRPP and conservative treatment.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home