|
Table of Content - Volume 19 Issue 1 - July 2021
Prospective study of vacuum assisted closure in treatment of soft tissue injuries associated with compound fractures
Kartik Ghate1, Nishad Situt2*
1Junior Resident 3, Department of Orthopaedics, Vilasrao Deshmukh Government Institute of Medical Science, Latur, INDIA. 2Assistant Professor, Department of Orthopaedics, Swami Ramanand Teerth Rural Medical College, Ambajogai, INDIA. Email: situt.nishad@gmail.com
Abstract Background: Open fractures are injuries in which skin and soft tissue are disrupted and the underlying bone is exposed to the external environment. Vacuum-assisted closure (VAC) is new in the armamentarium of managing wounds acute and chronic. Aim: Vacuum-assisted closure (VAC) is new in the armamentarium of managing wounds acute and chronic. To study the duration required for making the wound fit for skin cover procedures. Material and Methods: A total of 50 patients with Compound fracture were included in the study , their wound were debrided and VAC dressings applied, each dressing for 72 hrs till healthy granulation appear. Follow up of patients were done till definitive skin cover procedures like split skin graft or skin flap are done. Result: the prevalence of infection was 12%. The duration required for healthy granulation tissue and for making the wound fit for skin cover procedures was 9 days i.e. 45(90%) and12 days in only 5(10%) patients. Conclusion: With VAC dressing the granulation tissue formed was healthy and uniform. The wound was fit for definitive skin cover procedures like split skin grafting and flap cover at a faster rate.
INTRODUCTION Open fractures are injuries in which skin and soft tissue are disrupted and the underlying bone is exposed to the external environment. This leads to contamination by micro-organisms that can cause deep and superficial infection. The management of severe open fractures of the lower leg remains a major challenge in surgery, and adequate treatment of the concomitant soft tissue injury is of the highest priority, since it determines the fate and outcome of bone and extremity.1 Open fractures are classified according to Gustilo-Anderson classification system4. High-energy open fractures require both skeletal stability and adequate soft tissue coverage2. In such injuries, debridement of all non-viable tissue can produce significant soft tissue defects. Various surgical methods have been developed to obtain coverage in these difficult situations, including skin grafts, local rotation flaps, and myocutaneous or fasciocutaneous tissue transfers. Although skin grafts are readily obtainable, they are dependent on the vascularity of its recipient bed and may be contraindicated when exposed bone, cartilage, tendons, or surgical implants exist.5 In such situation, a local rotation flap may be needed when the soft tissue defect prevents local coverage.6 Wound healing is a complex and dynamic process. The sequence begins with removal of debris, control of infection, granulation, contraction, remodelling of the connective tissue matrix, and maturation. When wound fails to undergo this sequence of events, a chronic open wound without anatomical or functional integrity results .3 The treatment of chronic open wounds is variable and costly, demanding lengthy hospital stays or specialized home care requiring skilled nursing and costly supplies. Rapid healing of chronic wounds could result in great decrease in the risk of infection, amputation, and length of hospital stay and result in an estimated potential annual savings of billions of rupees of healthcare cost .7 Vacuum-assisted closure (VAC) is new in the armamentarium of managing wounds acute and chronic. VAC also called negative pressure wound therapy(NPWT) is a procedure in which vacuum with intermittent 125 mmHg negative pressure effect is used to enhance wound healing. The negative pressure is maintained by an apparatus, this promote healing in various kinds of wounds. It also helps in wound debridement by removing fluid, decreases edema, increases blood circulation and decreasing bacterial counts. The technique is less expensive than conventional management of complex wounds.8 The present study deals with the outcome of soft tissue injuries with open fracture treated with VAC.
MATERIALS AND METHODOLOGY In our institution 50 patients with Compound fracture were selected for this prospective study. The study period is from January 2019 to June 2020 All patients were selected based on our inclusion and exclusion criteria. Inclusion criteria: Patients with Compound Open fractures, where primary closure is not possible and requires surgical debridement Exclusion criteria: Pathological fractures with untreated osteomyelitis. Presence of a thick, necrotic eschar in wound. Patients with hemophilia or haemoglobinopathies. Open fractures that could be closed in initial surge Assessment of wound before applying VAC therapy: The patients with compound fracture were admitted, detailed history was elicited from patient and/or attendants to reveal the mechanism of injury, severity of trauma and demographic data. Then patients were assessed clinically to rule out other significant injuries like chest, abdominal or head injury. Local examinations were done for evaluation of wound location, number, dimentions, bleeding vessels, contamination, exposed tendons or fracture fragments, palpable crepitus, neurological examination to rule out nerve injury. The clinical diagnosis was confirmed radiologically by taking x-ray of limb segment with proximal and distal joint in 2 views. Initially the wound is thoroughly debrided and all the infected and foreign materials like mud etc are removed and through wound wash is given. Antibiotics are given as soon as the patient is received in the emergency ward. Initially broadspectrum antibiotics are given and later specific antibiotics are given according to sensitivity profile. Investigations: 1)Pus C/S 2)ESR 3)CRP Electronic vacuum assisted closure system: Specifications:
Timing of application of VAC therapy: Among the 50 patients for 14 patients VAC dressing was applied within 24 hrs of admission in our hospital and for 3 patients who had already developed superficial infection, the wound was thoroughly debrided and then VAC dressing was applied. Procedure: Choice of anaesthesia was decided by anaesthetists and the same informed to patient, repeat dressings were applied without any anesthesia.
Protocol after each dressing:
Skin cover procedures if needed: Follow up of patients were done till definitive skin cover procedures.
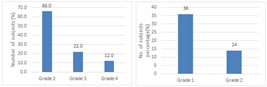
RESULT We included total 50 patients with Compound Open fractures, where primary closure is not possible and requires surgical debridement. Out of 50 patients, majority were from 20-30 years age group i.e. 17(34%) followed by 15(30%) from 41-50 years, 9(18%) from 31-40 and 51-60 years age groups each. Mean age of the participants was 38.08±10.88 years. Majority of the patients in our study were males i.e. 41(82%) and remaining were females i.e. 9(18%). Males were predominant in our study with male to female ratio was 4.55:1. Road Traffic Accident(RTA) was predominant mode of injury with 43 patients affected i.e. 86% followed by Train Traffic Accident(TTA) with 5(10%) patients and 2(4%) with Accidental Fall. Site involved was leg in majority of the patients i.e. 23(46%) followed by forearm in 11(22%), foot in 10(20%) and thigh in 6(12%) cases. Assessment of wound before procedure as per Gustilo-Anderson classification system revealed Grade 2 in 33 patients i.e. 66% followed by Grade 3 in 11(22%) and Grade 4 in 6(12%) (fig 1). Assessment of wound after procedure revealed Grade 1 in majority of the cases i.e. 72% and Grade 2 in 14(28%) cases (fig 2). Additional procedures performed on the patients are, 47 patients (94%) received split skin grafting and flap in 3 patients (6%) (Table 1).
Figure 1: Wound grade before procedure Figure 2: Wound grade after procedure
Table 1: Additional procedure performed Table 2: Duration of skin cover procedures
Table 2
Post-operative infection was seen in 6 patients in our study. So the prevalence of infection was 12%. In majority of the patients, duration required for healthy granulation tissue and for making the wound fit for skin cover procedures was 9 days i.e. 45(90%) and in only 5 patients i.e. 10% it was 12 days (Table 2). Table 3: Descriptive statistics of the variables
Mean Age of the patients was 38.08±10.88; Mean Size reduction (mm) was 14.12±3.31; Mean Hospital stay was 15.76±1.36 days Table 4: Prevalence of infection according to site
Chi square test-3.52, p-0.31 (>0.05), Not significant Out of 6 patients with post-operative infection, in most of the patients’ forearm was injure i.e. 3 patients (50%), legs in 2 patients i.e.33.3% and foot in one patient i.e.16.7%
Figure 3: Pre vac status After 1st vac dressing Figure 4: After second vac dressing After split skin grafting
DISCUSSION Complex musculoskeletal wound due to high energy poses a challenge to the treating surgeons regarding wound healing, coverage and reconstruction. The concept of using negative pressure to create a suction force, enabling the drainage of surgical wounds in order to promote wound healing, is well documented in the literature.9,10 The application of negative pressure removes excess fluid thus promote better capillary circulation and hyperaemia, decreases bacterial load and risk of bacterial colonization and had mechanical effect in drawing wound edges closer. Microscopically application of VAC therapy also showed increase in formation of new blood vessels and formation matrix tissue but the wounds treated by saline dressing showed inflammatory tissue and fibrous tissues as compared by above studies. The uniform negative pressure delivered by the VAC therapy to the wound bed plays a significant role in formation of new healthy granulation tissue. We included total 50 patients with Compound Open fractures, where primary closure is not possible and requires surgical debridement. Out of 50 patients, majority were from 20-30 years age group i.e. 17(34%) followed by 15(30%) from 41-50 years, 9(18%) from 31-40 and 51-60 years age group. Mean age of the participants was 38.08±10.88 years. Majority of the patients in our study were males i.e. 41(82%) and remaining were females i.e. 9(18%). Males were predominant in our study with male to female ratio was 4.55:1 Raj M. et al..11 included 14 males and 6 female patients in the study. The average patient age was 36.15 years (range 18 to 62 years). Venu Madhav HV et al..15 reported that 17 patients were treated with VAC therapy of age between 21yrs to 60yrs. Among the 17 patients 15 were male and 2 were female. Mean age of the group is 40.5 years. The age group 30-50 dominates the series accounting for 44% among the cases. Mode of injury RTA was predominant mode of injury with 43 patients affected i.e. 86% followed by TTA with 5(10%) patients and 2(4%) with fall. Site involved was leg in majority of the patients i.e. 23(46%) followed by forearm in 11(22%), foot in 10(20%) and thigh in 6(12%) cases. Raj M. et al.11 reported that mmajority of patients with open injury presents due to road traffic accident (70%), followed by patient who had fall from height (30%). Venu Madhav HV et al.15 reported that road traffic accidents include 14 cases (82.35%), train traffic accident 2 cases (11.76%) and accidental fall 1 case (5.88%). He also reported that majority of the cases site of injury was leg in 47.05%, forearm in 23.52%, foot in 17.64% and thigh in 11.76%. These findings are similar with our study findings. Wound characteristics Assessment of wound before procedure revealed Grade 2 in 33 patients i.e. 66% followed by Grade 3 in 11(22%) and Grade 4 in 6(12%). Assessment of wound after procedure revealed Grade 1 in majority of the cases i.e. 72% and Grade 2 in 14(28%) cases Urschel et al.12 proposed that the negative pressure had mechanical effect on the wound bed. The negative pressure causes the contact wound dressing to collapse; the force of this collapse is transferred on to the wound edges; which draws them close together. In the present study there was decrease in wound size attained by VAC therapy ranged from 2.6 to 24.4 cm2, with an average reduction of 11.2 cm2. Similar results were achieved by other authors also. McCallon et al.13 reported an average decrease in wound surface area of 28.4% (SD 24.3) using topical negative pressure. Joseph et al.14 reported a significant reduction in wound volume of 78%in the TNP group compared with 30% in the gauze group within 6 weeks (p=0.038). Post-operative infections Post-operative infection was seen in 6 patients in our study. So the prevalence of infection was 12%. Venu Madhav HV et al.15 reported the prevalence of infection in his study as 11.7% which is similar to our findings. Charalambous et al.16 reported prevalence of 27% and Gopal et al..17 reported prevalence of 27.4% % which is very high as compared to our findings. Henley et al.18 reported prevalence of infection as 34.7% which is very high as compared to our findings. Duration required for healthy granulation tissue In our study, majority of the patients, duration required for healthy granulation tissue and for making the wound fit for skin cover procedures was 9 days i.e. 45(90%) and in only 5 patients i.e. 10% it was 12 days. Venu Madhav HV et al..15 found that the mean duration required for formation of healthy uniform granulation bed was 10.5 days (9-12 days) which is consistent with our study findings. Similar studies were conducted by Morykwas MJ et al..19 showed that VAC proved effective in shrinking of the diameter of the wound size and formation of healthy granulation tissue when compared to normal saline dressing methods.
CONCLUSION The rate of wound infection was significantly reduced. Hospital stay was reduced. The granulation tissue formed was healthy and uniform. The wound was fit for definitive skin cover procedures like SSG and flap cover at a faster rate.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home